Case Report - International Journal of Clinical Rheumatology (2021) Volume 16, Issue 1
Ankylosing spondylitis: Diagnosis in sub-saharan african setting
- Corresponding Author:
- Abilo Tadesse
Department of Internal Medicine
College of Medicine and Health Sciences
University of Gondar, Ethiopia
E-mail: abilo.tadesse@yahoo.com
Abstract
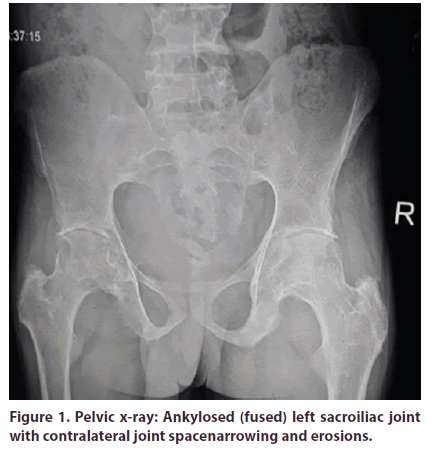
Background: Ankylosing spondylitis is a subset of spondyloarthritis, characterized by chronic inflammatory back pain in adolescents or young adults. ‘Imaging arm’ of ASAS classification criteria established ankylosing spondylitis as radiographic sacroiliitis. Case presentation: A 29-year-old man presented to university of Gondar hospital, Northwest Ethiopia with inflammatory back pain of 15 years duration. Radiographic imaging revealed grade 3 sacroiliitis (left sacroiliac joint ankylosis and contralateral joint space narrowing and erosions). Other supporting clinical findings were peripheral arthritis, anterior uveitis, elevated ESR, and family history of inflammatory back pain.In sum, ‘imaging arm’ of ASAS classification criteria established radiographic axial spondyloarthritis and modified New York diagnostic criteria diagnosed ankylosing spondylitis.He had physical disability with BASFI score of 5/10 on initial evaluation. He was treated with topical steroid eye drops for uveitis and oral NSAIDs for spondyloarthritis. Physical therapy was initiated as rehabilitative measure. He got symptomatic benefit with above therapeutic regimen. He waslinked to Chronic Illness Care Clinicand Ophthalmology Clinic of the hospital for follow-up. Conclusion: Ankylosing spondylitis had significant impact on physical function and quality of life in African setting.Possible reasons could be late diagnosis due todelayed radiographic evidences and limited access to magnetic resonance imaging, inadequate therapy with available NSAIDs and unavailability of biologic DMARDs.
Keywords
ankylosing spondylitis ● Northwest Ethiopia
Abbreviations
AS: Ankylosing Spondylitis ● ASAS: Association of SpondyloArthritis International Society ● BASDAI: Bath Ankylosing Spondylitis Disease Activity Index ● BASFI: Bath Ankylosing Spondylitis Functional Index ● bDMARDs: biological Disease Modifying Anti-Rheumatic Drugs ● CRP: C-Reactive Protein ● ECG: Electrocardiography ● ECHO: Echocardiography ● ESR: Erythrocyte Sedimentation Rate ● IL-i: Interleukin inhibitors ● HLA: Human Leukocyte Antigen ● NSAIDs: Non-Steroidal Anti-Inflammatory Drugs ● SpA: Spondyloarthritis ● TNF-i: Tumor Necrosis Factor inhibitors
Introduction
Ankylosing spondylitis (radiographic axial spondyloarthritis) is a potentially disabling,chronic inflammatory arthritis of the spine and sacroiliac joints. Genetic, immunologic and environmental factors were thought to play a role in causation of ankylosing spondylitis. The classic clinical description of ankylosing spondylitis was made in the late1800s. Chronic inflammatory back pain ≥ 3 months in a young adult and radiologicor MRI-evidenced sacroiliitis in the presence of one or more other spondyloarthritis features classify as radiographic axial spondyloarthritis and confirm diagnosis of ankylosing spondylitis [1-6]. Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) and biological Disease Modifying Anti-Rheumatic Drugs (bDMARDs) are therapies available for ankylosing spondylitis to provide symptomatic benefit and retard progressive spinal damage [7-10]. Here, we discuss the clinical presentation, diagnosis and treatment of a rare, potentially disabling rheumatologic disorder in sub-Saharan African setting.
Case Presentation
A 29-year-old man presented to University of Gondar hospital, Northwest Ethiopia with long standing repeated episodes of low back pain of 15 years duration. The back pain woke him up at night and had morning stiffness. He had episodes of painful, bilateral ankle joint swelling in the past 5 years. He had associated low grade fever, malaise, fatigue and weight loss. He had recurrent painful, red eye with photophobia and blurred vision during flare up of spinal and peripheral joint pain. There was characteristic inflammatory low back pain among the family members. He was treated for skeletal tuberculosis 4 years back but there was no significant clinical improvement after completion of 6 months of anti-tuberculosis therapy. He quitted farming activities due to illness. He was repeatedly treated with non-steroidal anti-inflammatory drugs and benefited him to relieve the symptoms. He had no history of recurrent diarrhea and abdominal pain, urethral discharge or painful urination, skin lesions or oral ulcers. He never smoked cigarettes and was casual alcohol consumer. Serologic test for HIV infection was negative. He was evaluated in ophthalmology clinic for painful, red left eye and diagnosed to have anterior uveitis. He was treated with topical steroid eye drops and scheduled for follow-up.
On physical examination, he was nourished, conscious, and oriented. His Blood Pressure (BP) was 100/70 mmHg, Pulse Rate (PR) 90 beats per minute, Respiratory Rate (RR) 16 breaths per minute, and temperature (T°) 36.5°C. His arterial oxygen saturation (SaO2) was 94% with room air. There were no scalp lesions or hair loss. On ophthalmic examination, he had painful, red left eye with OD 6/6 and OS 6/6. He had irregular pupil, keratic precipitates on the left eye on slitlamp examination. The chest was resonant to percussion and clear to auscultation. S1 and S2 were well heard, and no murmur or gallop on cardiovascular examination. No abnormality noticed in abdominal examination. On musculoskeletal examination, he had limitation of anterior spinal flexion (positive modified Schober’s test). He had tenderness, swelling and limitation of movement of bilateral feet joints. There were no skin lesions or nail deformities on integumentary system. Nervous system examination showed no abnormality.
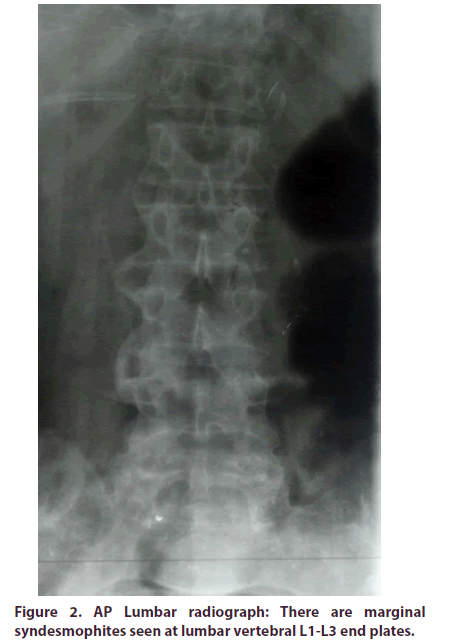
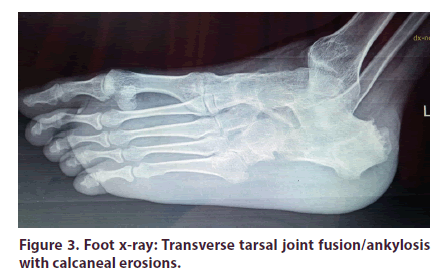
A laboratory examination revealed hemoglobin 12 gm/dl (normal, 12–18 gm/dl), total leukocyte count 7,500/μl (normal, 4000–11,000/μl; granulocyte 54%, lymphocyte 35%), and platelet count 350,000/μl (normal, 150,000–450,000/μl), ESR 85 mm in first hour, and Rheumatoid Factor (RF) was non-reactive. Serum biochemical tests were within normal range. Radiography revealed ankylosed (fused) left sacroiliac joint and contralateral joint space narro wing and erosions (Figure 1). Marginal syndesmophites were seen at the lumbar vertebral L1-L3 end plates(Figure 2). There was bilateral transverse tarsal joint ankyloses with calcaneal erosions (Figure 3). No abnormal findings on radiography of hands and chest.ECG and ECHO were done and revealed no abnormalities. Genetic testing for HLA-B27 was not done due to limited clinical setup. Thus, presenting clinical and imaging features established radiographic axial spondyloarthritis using ASAS classification criteria and ankylosing spondylitis using modified New York diagnostic criteria. He scored 5/10 using BASFI scoring system on initial evaluation to determine degree of functional limitation. He was treated with Indomethacin, 25 mg po four times daily for two weeks, and then started physical therapy. The drugwas continued until severe symptoms subside. He got symptomatic benefit with above therapeutic regimen, and then referred to chronic illness care clinic for follow-up.
Discussion
Ankylosing spondylitis (radiologic axial spondyloarthritis) represents auto-immune inflammatory arthritis that manifests as chronic back pain and stiffness of the spine. Immune mediated mechanisms involving HLA-B27, cytokines (TNF and ILs), inflammatory cells infiltrate, and genetic and environmental factors were thought to play key roles in pathogenesis of AS [1-6]. HLA-B27 is virtually absent in most of the Sub-Saharan African population, making ankylosing spondylitis a rare disease in the region (0-8 per 10,000) [11-14]. Inflammatory back pain ≥ 3 months in a young adult andradiographic- or MRI-evidenced sacroiliitis in the presence of one or more other spondyloarthritis (SpA)feature ssuggest radiographic axial spondyloarthritis[1-6]. SpA features include articular manifestations (inflammatory back pain, peripheral arthritis, dactylitis, or heelenthesitis), extra-articular features (anterior uveitis, psoriasis, or inflammatory bowel disease), inflammatory markers (elevated ESR or CRP), HLA-B27 positivity, good response to NSAIDs, and family history of spondyloarthritis. Inflammatory back pain should exhibit at least four of the following five features, and include age at onset <45 years, insidious onset, improvement with exercise, no improvement with rest, and pain at night (with improvement upon arising). Radiographic features should fulfill bilateral sacroiliac jointerosions and sclerosis (grade 2), or unilateral or bilateral sacroiliac joint ankylosis(grade 3-4). MRI features should reveal subchondral bone marrow edema in active inflammation and structural lesions (bone erosions, sclerosis, new bone formation, fat infiltration) in chronic inflammation to diagnose sacroiliitis.Our patient had all features of inflammatory back pain. Radiologic imaging revealed grade 3 sacroiliitis (leftsacroiliac joint ankylosis with contralateral joint narrowing and erosions). He had other SpA features such as peripheral arthritis, anterior uveitis, elevated acute phase reactant (ESR) and family history of SpA. In sum, he metASAS classification criteria for radiographic axial spondyloarthritis, and ankylosing spondylitis using modified New York diagnostic criteria. Possible differential diagnoses were shown in Table 1. Although few African case studies reported ankylosing spondylitis as variably mild to severe disease, older age at presentation, and lacked family history and extraarticular features like uveitis, our case presented with typical features of ankylosing spondylitis with significant functional limitation (BASFI score=5/10)[11-14]. Primary goals of therapy in ankylosing spondylitis include improving health-related quality of life through control of symptoms, prevention of spinalstructural damage, and maintaining the ability to work. NSAIDs and physical therapy are corner stone therapies of choice in ankylosing spondylitis. There is increasing evidence that Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) are highly effective not only to control symptoms but also retard spinal structural damage. Physical therapy as well reduces painful symptoms and improved spinal mobility and function. Biological Disease Modifying Anti-Rheumatic Drugs (DMARDs (TNF-i, IL-i)) are indicated in persistentand progressivespinal disease activity (BASDAI ≥ 4) despite adequate NSAIDs therapy (no response to at least 2 NSAIDs for at least 4 weeks in total) (11-14). In conclusion, Ankylosing spondylitis had significant impact on physical function and quality of life in African setting. Possible reasons could be late diagnosis due to delayed radiographic evidences and limited access to magnetic resonance imaging, inadequate therapy with available NSAIDs and unavailability of biologic DMARDs.
Table 1. Differential diagnoses of ankylosing spondylitis.
| Characteristics | AS | Psoriatic arthritis | Reactive arthritis | Enteropathy-assoc. arthritis |
|---|---|---|---|---|
| Age (years) | 17-45 | 30-40 | 20-40 | 20-30 |
| Gender (M:F ratio) | 1:1 | 1:1 | 1:1 | 1:1 |
| Preceding symptoms | None | Psoriasiform skin lesions | Bowel symptoms & urethritis | Bowel symptoms |
| Associated features | None | Skin, digit & nail changes | Keratodermablennorrhagica | Bowel sxs& skin lesions |
| Sacroiliitis | Symmetrical | Asymmetrical | Asymmetrical | Symmetrical |
| Syndesmophytes | Marginal & Symmetrical | Non-marginal & asymmetrical | Non-marginal & asymmetrical | Marginal & symmetrical |
| Uveitis | Acute & Unilateral | Chronic & bilateral | Acute or chronic uveitis & unilateral | Chronic, bilateral |
| Arthritis | Oligoarthritis | Oligo/Polyarthritis | Oligoarthritis | Oligo/Polyarthritis |
| HLA-27 (%) | 75-90% | 50-70% | 30-50% | 30-70% |
M:F ratio: Male-to-Female ratio;Â Sxs: symptoms
Conclusion
Ankylosing spondylitis had significant impact on physical function and quality of life in African setting. Possible reasons could be late diagnosis due to delayed radiographic evidences and limited access to magnetic resonance imaging, inadequate therapy with available NSAIDs and unavailability of biologic DMARDs.
Authors’ contributions
YM, AA, and AT performed clinical diagnosis and participated in patient care. TY performed radiologic diagnosis. AT wrote the initial draft of thecase report. All authors reviewed and approved the final case report.
Ethics approval and consent to participate
The authors declare that ethics approval was not required for this case report as we did not use any new procedures or treatment, which wasnot approved for clinical use in our institution.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Competing interests
The authors declare that they have no competing interests.
References
- Rudwaleit M, van der HD, Landewé R et al. The development of Assessment of SpondyloArthritis International Society Classification Criteria for axial spondyloarthritis (part II): validation and final selection. Ann. Rheum. Dis. 68(6), 777–783 (2009).
- Rudwaleit M, van der Heijde D, Landewe R et al. The Assessment of SpondyloArthritis International Society Classification Criteria for peripheral spondyloarthritis and for spondyloarthritis in general. Ann. Rheum. Dis. 70(1), 25–31 (2011).
- Van Der Linden S, Hans A, Valkenburg et al. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis. Rheum. 27(4), 361–368 (1984).
- Taurog JD, Chhabra A, Colbert RA. Ankylosing spondylitis and axial spondyloarthritis. N. Engl. J. Med. 374, 2563–2574 (2016)
- Proft F, Poddubnyy D. Ankylosing spondylitis and axial spondyloarthritis: recent insights and impact of new classification criteria. Ther. Adv. Musculoskel. Dis. 10(5-6), 129–139 (2018).
- Dean LE, Jones GT, Mac Donald AG et al. Global prevalence of ankylosing spondylitis. Rheumatology. 53, 650–657 (2014)
- Poddubnyy D. Axial spondyloarthritis: is there a treatment of choice? Ther. Adv. Musculoskel. Dis. 5(1), 45-54 (2013).
- Van Der Heijde D, Ramiro S, Landewe R et al. 2016 update of the ASAS-EULAR management recommendations for axial spodyloarthritis. Ann. Rheum. Dis. 76, 978–991 (2017).
- Poddubnyy D, Rudwaleit M, Haibel H et al. Effect of non-teroidal anti-inflammatory drugs on radiographic spinal progression in patients with axial spondyloarthritis: results from the German Spondyloarthritis Inception Cohort. Ann. Rheum. Dis. 71, 1616–1622 (2012).
- Kroon F, Landewe R, Dougados M et al. Continuous NSAID use reverts the effects of inflammation on radiographic progression in patients with ankylosing spondylitis. Ann. Rheum. Dis. 71, 1623–1629 (2012).
- Belachew DA, Sandu N, Schaller B et al. Ankylosing spondylitis in Sub-Saharan Africa. Post. Grad. Med. J. 85(1005), 353–357 (2009)
- Tikly M, Njobvu P, Mc Gill P. Spondyloarthritis in Sub-Saharan Africa. Curr. Rheumatol. Rep. 16(6), 421–429 (2014).
- Mijiyawa M, Oniankitan O, Khan MA. Spondyloarthropathies in Sub-Saharan Africa. Curr. Opin. Rheumatol. 12(4), 281–286 (2000)
- Chalmers IM. Ankylosing Spondylitis in Black Africans. Arthritis. Rheum. 23(12), 1366–1370 (1980).