Research Article - Diabetes Management (2017) Volume 7, Issue 2
Adherence to self-care among individuals with diabetes with and without diabetic foot complications: objective and self-report measures
- Corresponding Author:
- Rachel Natovich
Department of Public Health
Ben-Gurion University of the Negev, Israel
E-mail: rnatovich@gmail.com
Abstract
Aim: Adherence to self-care recommendations is a key factor in ulcer healing and prevention. There is paucity of data regarding adherence in this high risk group. We compare self-care adherence levels among adults with diabetes, with and without the diabetic foot (DF) complication. Methods: Case-control study conducted among adults with diabetes. 99 individuals with (cases) and 95 without DF (control) were recruited. Groups were matched for gender and diabetes duration. Adherence was inferred from self-reported activities, using the Summary of Diabetes Self-Care Activity questionnaire and two objective measures of treatment efficiency: Body Mass Index, and glycated hemoglobin level (HbA1c). Results: DF adhered significantly (p<0.01) less than controls to physical activity, but more (p<0.5) to performing blood tests. HbA1c levels were significantly (p<0.001) higher in the DF group (x Ì… 8.8 vr. 7.3). Differences persisted in a multivariable analysis after adjusting for several confounding factors. Conclusions: our data show that individuals with DF had the same or lower levels of adherence in all domains, aside for better adherence to blood tests. Thus, the presence of DF does not seem to act as a "wake up call" and is not translated into better adherence.
Keywords
diabetic foot, self-care, adherence, physical activity, glycemic control
Introduction
Diabetic foot (DF) is one of the most severe and costly long term complications of diabetes, associated with a 2 fold increase in morbidity and mortality [1]. Since the 1990s’ famous St Vincent Declaration [2] that set a target to ‘reduce the numbers of limb amputations for diabetic gangrene by 50% in a five-year period,’ there has been a worldwide effort to attain this goal. It has since been shown that the implementation of comprehensive programs focusing on foot care can prevent or reduce the development of this and other diabetes complications [3].
The American Diabetes Association (ADA) and the International Working Group on the Diabetic Foot (IWGDF) have periodically published treatment recommendations containing evidence-based guidance for the management and prevention of diabetic foot [4,5]. These recommendations specifically emphasize the importance of self-care management for achieving positive outcomes. An important advantage of self-care management is that it can reduce the gap between patient needs and available health care services to meet those needs [6].
Good adherence to self-care was found to be positively correlated with good glycemic control and improved quality of life [7], as well as reduced risk for diabetes complications and death [8]. In a prospective study [9], 1257 people with diabetic foot were followed for 18 months. Research results showed that high adherence to medical advice was associated, in this group, with a significantly higher rate of ulcer healing and a lower chance of developing new ulcers or requiring surgical procedures. In another study, proper foot self-care behaviors were found to reduce the risk of injury, infection, and amputation in this high risk group [10].
Given the existence of evidence-based recommendations for self-care and the substantial evidence for its efficacy in the prevention of occurrence or recurrence of foot complications, one would expect a “wake up call” in the form of an ulcer to be translated into high levels of adherence to self-care among individuals with DF. On the other hand, adherence to self-care among individuals with diabetic foot may be compromised since the DF condition per se significantly increases the burden of illness and of self-care imposed on the individual with diabetes. After all, self-care is a complex, multifaceted task which involves a variety of health promoting activities such as keeping a proper diet, engaging in physical activity, adhering to a medication plan, medical surveillance, and self-inspection. However, there is a paucity of research regarding adherence in the high-risk group of individuals with diabetic foot.
In this paper we compared self-care adherence levels among adults with diabetes, with and without the DF complication.
Material and methods
▪ General
This was a case-control study of adherence to self-care recommendations, conducted among adults with diabetes, with (cases) and without (control) diabetic foot (DF), after matching for gender and diabetes duration. Adherence was ascertained from self-reported activities and by two objective commonly used measures of treatment efficiency: Body Mass Index (BMI), and glycated hemoglobin level (HbA1c).
▪ Population
Included in the study were individuals aged 45-75 with a diagnosis of Type 2 diabetes, who was able to speak and write in Hebrew. Excluded were people with significant visual, hearing, or motor impairments that could hinder responding to self-report questionnaires.
▪ Procedure
Ninety-nine individuals with DF were recruited from in-hospital orthopedic departments and diabetic outpatient foot clinics in two hospitals. Ninety-five individuals with diabetes without DF were recruited from several community based diabetic clinics in the biggest HMO in Israel. The existence or absence of DF was determined by the treating physician. Patients found eligible by their treating physician were contacted by telephone and invited to participate in the study. Each participant was invited for a personal interview with a psychologist who administered the questionnaires and assessed depression. Medical indices were collected from participants’ medical records. The study was approved by the appropriate ethics committees.
▪ Measures
Self-report measures of adherence
The Summary of Diabetes Self-Care Activity (SDSCA) [11] was used to assess the level of adherence in specific domains. The SDSCA is a brief, reliable, valid, and multidimensional self-report measure of adherence to nutrition, physical activity, blood tests, medication plan, and smoking status. Participants reported how many days in the prior week they had engaged in each of the activities.
Objective measures of adherence
As the SDSCA is a self–report adherence measure, two additional objective measures of adherence were also collected from the participants’ electronic medical records: BMI and HbA1c. HbA1c is a well validated measure reflecting mean glucose levels in the 3 preceding months [12]. There is a strong relationship between HbA1c values and adverse outcomes in people with diabetes, including incident retinopathy, nephropathy, and cardiovascular disease [13]. BMI as well is considered a measure of treatment efficacy, and the ADA recommends that individuals with diabetes achieve or maintain a normal weight. A J-shaped association was found between BMI immediately before a diagnosis of Type 2 diabetes and allcause mortality [14].
Additional medical measures
Medical indices related to disease severity and treatment effectiveness were also collected from the electronic medical records of the research participants. For the purpose of this analysis, hypertension was defined as elevated blood pressure requiring medical therapy, and dyslipidemia was defined as elevated LDL or triglycerides requiring medical therapy. Data on prevalent retinopathy, nephropathy, and neuropathy were collected from the medical records. Macro-vascular disease was defined as reported angina, Myocardial Infarction (MI), or Peripheral Vascular Disease (PVD).
Depression
The Patient Health Questionnaire (PHQ- 9) was used to assess depression. The PHQ-9 is a 9 item depression screening instrument that asks about the frequency of symptoms of depression over the past 2 weeks. PHQ- 9 score ≥10 has shown a sensitivity of 80% and a specificity of 92% for major depression [15,16].
Statistical analysis
The differences between the groups with and without DF in the specific adherence domains were first examined with Student’s t-tests. Multiple linear regression analyses were used to test the differenc e between the groups, using consecutive models, after adjustment for age, depression status, smoking, macro vascular disease, retinopathy, and nephropathy. Neuropathy was not added to the regression model because of Multicollinearity with the DF group (Pearson’s correlation 0.732, p<0.001).
Results
This analysis pertains to 99 individuals with DF and 95 individuals with diabetes without DF (general diabetes, GD), matched for sex and diabetes duration. As can be seen (TABLE 1), individuals with DF were younger and had more diabetes complications than those without DF.
| DF | Diabetes | |
|---|---|---|
| n | 99 | 95 |
| Sex (% male) | 77 | 80 |
| Age (mean years) | 58.04 (6.87) | 61.3 (7.03)*** |
| Education (mean years) | 12.4 | 14.5*** |
| Current smoking (%) | 26.3 | 21.1 |
| Depressive symptoms (mean) | 6.13(5.97) | 4.73 (4.26) |
| Insulin use (%) | 81.8 | 25.3*** |
| Hypertension (%) | 76.8 | 60* |
| Dyslipidemia (%) | 76.8 | 68.4 |
| Retinopathy (%) | 51.5 | 9.5*** |
| Neuropathy (%) | 88.9 | 15.8*** |
| Nephropathy (%) | 33.3 | 3.2*** |
| Macro-vascular disease (%) | 88.9% | 51.6%*** |
Table 1: Socio-demographic and medical variables by group.
Adherence to treatment, self-report measures
TABLE 2 shows the results of comparisons between the two groups in the different adherence domains. Two important differences were found between the two groups. The DF group showed significantly (p<0.01) less adherence to physical activity than controls. This pattern was maintained after adjustment for several possible confounding factors, including education, smoking status, symptoms of depression, and micro and macro vascular disease. On the other hand, DF were significantly (p<0.05) more adherent to blood tests. This pattern was also maintained after adjusting for all the above confounding factors, excluding retinopathy and nephropathy. No difference was found between the groups in adherence to diet and medications.
| Adherence Domain* | Model 0 | Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Beta | t | Beta | t | Beta | t | Beta | t | Beta | t | |
| Physical act | –0.827 | –3.225** | –0.827 | –3.217** | –0.814 | –3.159** | –0.814 | –3.119** | –0.829 | –2.847** |
| Blood test | 1.179 | 2.510* | 1.179 | 2.508* | 1.158 | 2.456* | 1.079 | 2.270* | 0.479 | 0.917 |
| Medicine use | 0.152 | 0.562 | 0.152 | 0.561 | 0.155 | 0.567 | 0.106 | 0.384 | 0.040 | 0.130 |
| Diet | –0.514 | –1.885 | –0.518 | –1.916 | –0.498 | –1.840 | –0.500 | –1.824 | –0.546 | –1.767 |
Linear regression, **p<0.01, *p<0.05; Model 0: After adjustment for age and education, Model 1: After adjustment for Model 0+current smoking status, Model 2: After adjustment for model 1+depressive symptoms, Model 3: After adjustment for Model 2+macrovascular disease, Model 4: After adjustment for Model 2+retinopathy+nephropathy.
Table 2: Between-group comparisons of self-reference adherence domains.
Objective measures of adherence/treatment efficacy
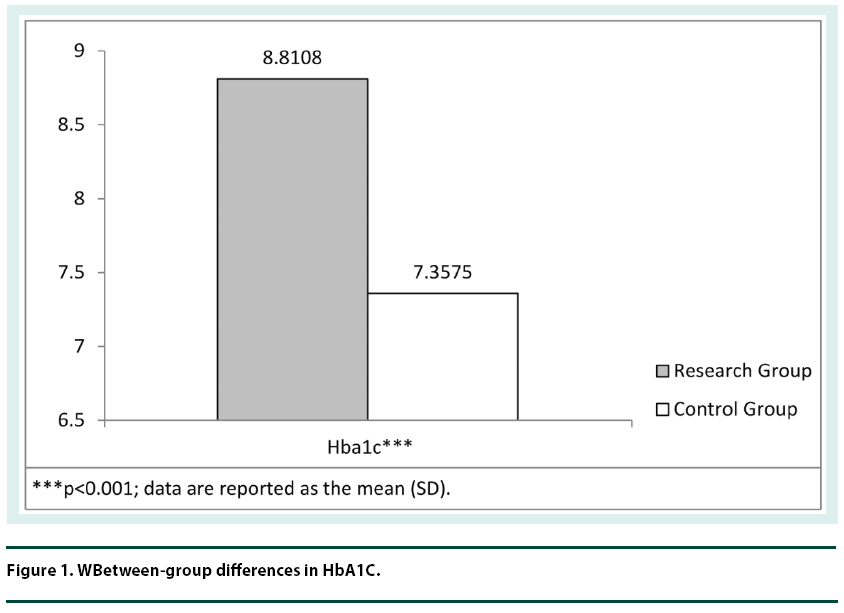
FIGURE 1 shows the differences between the groups in HbA1C levels. HbA1c was significantly (p<0.001) higher in DF than in the control group even after adjustment for several possible confounding factors, including smoking status, depression symptoms, and micro and macro vascular disease. No differences were found between the groups in BMI levels (p>0.16).
Discussion
This is one of the first studies to investigate multi-faceted adherence in individuals with DF, compared to adults with diabetes who do not have this severe complication (GD). The main goal of this study was to examine whether the “wake up call” generated by the development of diabetic foot complication translates into increased adherence to health promoting behaviors. The adherence profile arising from our research data portrays individuals with DF as more adherent to blood tests, but significantly less adherent to physical activity recommendations, in comparison to the GD group. No differences were found between the groups in adherence to medication and diet. In addition, groups were found to be similar in BMI. However, the glycemic control (HbA1c) of the DF group was found to be significantly poorer. Though this finding is in itself not surprising, as poor metabolic control is a risk factor for development of diabetic foot, the continued raised HbA1c, after the appearance of diabetic foot, is puzzling: Despite DF reporting better adherence to blood tests, which mirrors better control, their glycemic control was poorer. Isn’t the whole purpose of constantly accepting the unpleasantness of having your finger pricked to attain the required behavior change and enhance health? This contradiction may have several plausible explanations.
First, the results may imply that DF individuals may have a problem linking test results to related behavioral implications. Indeed, in a recent study, DF participants were found to be challenged with more severe cognitive difficulties compared to individuals with diabetes without this complication [17]. Adequate adherence to the multi-faceted demands of self-management depends on good cognitive functioning. Another possible explanation of this discrepancy between better adherence to blood tests and poorer glycemic control may lie in the greater difficulty among DFs, in this study, to adhere to physical activity, which is known to be positively correlated with glycemic control [18,19]. This difficulty may be directly related to the limitations on physical activity imposed by the diabetic foot itself. However, physical activity is a broad and complex concept. Thus, although engaging in physical activities is more challenging for individuals with DF, it is achievable. Additionally, the discrepancy may arise from the method of data collection: whereas adherence to blood tests and medications was assessed by a self-report questionnaire, glycemic control was assessed objectively. More research is needed to explore these contradictory findings.
It is important to note that the higher HbA1c levels found in the DF group in this study ( 8.8) are also higher than consensus recommendations [4,5]. Maintaining appropriate glycemic control is of special importance in the prevention and possibly healing of DF. A reduction of up to 60% in the incidence of clinical neuropathy (a major risk factor for DF) was reported in patients managed with intensive compared to conventional glycemic treatment [20,21]. A graded positive association was found between HbA1c at baseline and during follow-up and the risk of lower extremity amputation (LEA) in individuals with diabetes. Each 1% increase in baseline HbA1c was associated in this study with a 13% (95% CI 1.08–1.17) increased risk of LEA [22]. Interestingly, the higher HbA1c levels in the DF group in this study, were not accompanied by higher BMI or with less selfreported adherence to diet. More research, using additional objective measures of adherence, is needed in order to explore the complex relationships between the different aspects of adherence in this high-risk group.
To conclude, the study’s original question was: Does the presence of diabetic foot complication act as a “wake up call” and translate into better adherence? Unfortunately, the answer is negative. Compared to individuals with diabetes without diabetic foot, DF had the same or lower levels of adherence in all domains, aside for better adherence to blood tests. They also maintained worse glycemic control. Considering the fact that diabetic foot remains one of the most severe yet potentially preventable complications of diabetes [23], we believe it is important to take these findings into consideration. The medical personnel treating individuals with diabetic foot should not automatically assume that the objective severity presented by the ulcer will translate into increased motivation for selfcare. A pro-active approach should probably be implemented, with enhanced therapeutic patient education and support for diabetes selfmanagement.
Some limitations of the study should be pointed out. First, it should be emphasized that the cross sectional design limits the ability to draw definitive conclusions about the causality of adherence patterns. Secondly, some adherence measurements relied on self-report measures prone to bias. In addition, the cohort of individuals with DF was recruited mainly from the orthopedic rehabilitation department, thus probably not representing the average individual with DF rather more likely the more severe cases. Prospective studies are needed in order to fully explore this important topic.
Author contributions
RN: Literature search, study design, neuropsychological evaluation and data extraction, figures, data analysis, data interpretation, writing of manuscript. She had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. IHB: Literature search, figures, study design, data interpretation, writing of manuscript, critical appraisal of manuscript. DM: Study design, data collection, and critical appraisal of manuscript. TCY: Literature search, study design, data collection, data analysis, figures, data interpretation, writing of manuscript, critical appraisal of manuscript. TK: Literature search, study design, figures, data interpretation, writing of manuscript, critical appraisal of manuscript.
Acknowledgment
We thank Dr. Joseph Natovich of Tiuv System Consultants for his assistance in data analysis.
References
- Iversen MM, Grethe S, Tell GS et al. History of foot ulcer increases mortality among individuals with diabetes: Ten year follow up of the Nord Trondelag health study. Diabetes Care. 32(12), 2193–2199 (2009).
- World Health Organization, International Diabetes Federation, Saint Vincent Declaration Working Group. Diabetes Mellitus in Europe: A problem at all ages in all countries: A model for prevention and self-care. Acta. Diabetol. 27(1), 181–183 (1990).
- Neder S, Nadash P. Individualized education can improve foot care for patients with diabetes. Home Healthc. Nurse. 21(12), 837–840 (2003).
- Schaper NC, Van Netten JJ, Apelqvist J et al. Prevention and management of foot problems in diabetes: A summary guidance for daily practice 2015, based on the IWGDF guidance documents. Diabetes Metab Res Rev. 32(Suppl. 1), 7–15 (2016).
- American Diabetes Association. Standards of medical care in diabetes—2015 abridged for primary care providers. Clin Diabetes. 33(2), 97–111 (2015).
- Barlow J, Wright C, Sheasby J et al. Self-management approaches for people with chronic conditions: A review. Pat. Educ. Couns. 48(2), 177–187 (2002).
- Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. J. Diabetes Metab. Disord. 12(1), 14 (2013).
- Chen Y, Sloan FA, Yashkin AP. Adherence to diabetes guidelines for screening, physical activity and medication and onset of complications and death. J. Diabetes Complicat. 29(8), 1228–1233 (2015).
- Viswanathan V, Madhavan S, Rajasekar S et al. Amputation prevention initiative in South India: Positive impact of foot care education. Diabetes Care. 28(5), 1019–1021 (2015).
- Bonner T, Foster M, Spears-Lanoix E. Type 2 diabetes–related foot care knowledge and foot self-care practice interventions in the United States: A systematic review of the literature. Diabetic Foot Ankle. 7(1), 29758 (2016).
- Toobert DJ, Hampson SE, Glasgow AR. The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care. 23(7), 943–950 (2000).
- Rohlfing CL, Wiedmeyer HM, Little RR et al. Defining the relationship between plasma glucose and HbA(1c): Analysis of glucose profiles and HbA(1c) in the Diabetes Control and Complications Trial. Diabetes Care. 25(2), 275–278 (2002).
- Stratton IM, Adler AI, Neil HA et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): Prospective observational study. BMJ. 321(7258), 405-412 (2000).
- Tobias DK, Pan A, Hu FB et al. Body-mass index and mortality among adults with incident type 2 diabetes. N. Engl. J. Med. 370(14), 233–244 (2014).
- Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Ann. 32(9), 509–515 (2002).
- Wang Y, Lopez JM, Bolge SC et al. Depression among people with type 2 diabetes mellitus, US National Health and Nutrition Examination Survey (NHANES), 2005–2012. BMC. Psychiatry. 16(1), 88 (2016).
- Natovich R, Kushnir T, Harman-Boehm I et al. Cognitive dysfunction: Part and parcel of the Diabetic Foot. Diabetes Care. 39(7), 1202–1207 (2016).
- Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: The evidence. CMAJ. 174(6), 801–809 (2006).
- Sigal RJ, Armstrong MJ, Colby P et al. Physical activity and diabetes. Can. J. Diabetes. 37, S40–S44 (2013).
- Bus SA, van Netten JJ. A shift in priority in diabetic foot care and research: 75% of foot ulcers are preventable. Diabetes Metab. Res. Rev. 32, 195–200 (2015).
- Martin CL, Albers JW, Pop-Busui R et al. Neuropathy and related findings in the diabetes control and complications trial/epidemiology of diabetes interventions and complications study. Diabetes Care. 37(1), 31–38 (2014).
- Zhao W, Katzmarzyk PT, Horswell R et al. HbA1c and lower-extremity amputation risk in low-income patients with diabetes. Diabetes Care. 36(11), 3591–3598 (2013).
- Boulton AJ, Vileikyte L, Apelqvist J et al. The global burden of diabetic foot disease. Lancet. 366(9498), 1719–1724 (2005).