Case Report - Imaging in Medicine (2017) Volume 9, Issue 4
A rare case of chronic calcific pancreatitis with intrahepatic and splenic pseudocysts
Sanjib Kumar Das*, Ipsita Acharya, Jayashree Mohanty, Sasmita Parida & Basanta Manjari SwainSCB Medical College, Cuttack, India
- Corresponding Author:
- Sanjib Kumar Das
SCB Medical College, Cuttack, India
E-mail: sanjib1988@gmail.com
Abstract
Pancreatic pseudocyst is a well-defined collection of fluid rich in pancreatic enzymes which occurs as a complication of pancreatitis. They are mostly located in the head and body of the pancreas while few are found in extra-pancreatic locations like mediastinum, liver, pelvis, pleura and spleen. However intrahepatic pseudocyst is a rare complication of pancreatitis with only 34 such cases being reported in English literature till the year 2009. Around 1 in 100 cases of pancreatic pseudocyst show extension into spleen.
Keywords
chronic calcific pancreatitis • intrahepatic • splenic pseudocyst
Introduction
A 41 year old Indian alcoholic male with a history of cholelithiasis presented with dull aching epigastric pain and mild abdominal distension. On physical examination, patient was found to have right upper quadrant and epigastric tenderness with hepatosplenomegaly. Laboratory investigations showed normal liver function with increased serum lipase.
We present a known case of gallstone disease with dull aching epigastric pain and abdominal distension, who on evaluation showed chronic calcific pancreatitis with intrahepatic and splenic pseudocyst.
Case
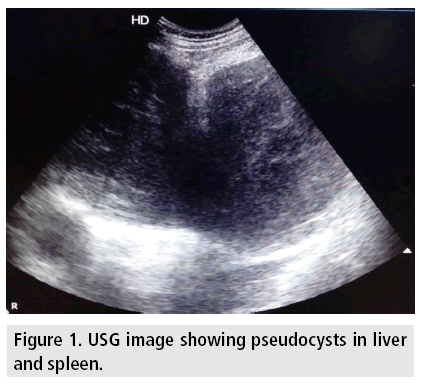
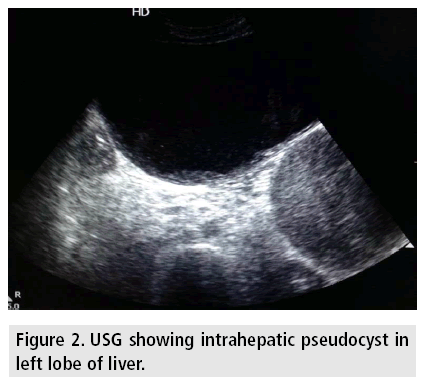
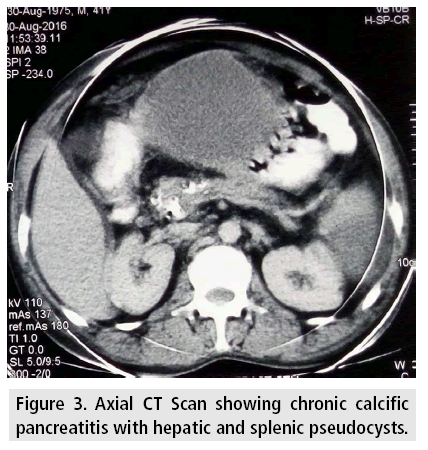
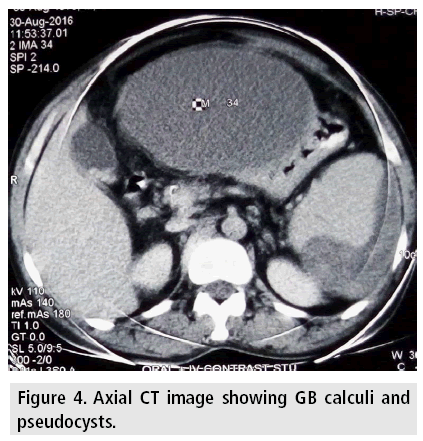
On USG, two large cystic lesions were noted in the liver and spleen. Thinned out pancreatic parenchyma with dilated MPD containing multiple calculi were also visualized suggesting chronic calcific pancreatitis. Multiple gallbladder calculi were also seen.
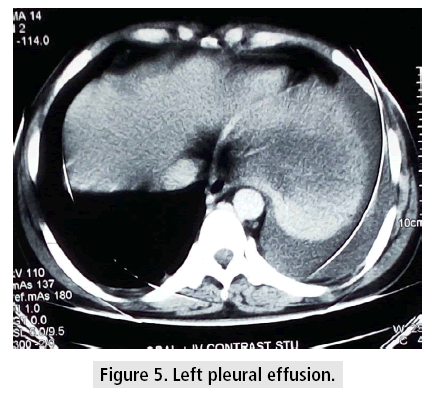
Further evaluation on CT showed similar findings of chronic calcific pancreatitis with intrahepatic and splenic pseudocysts (FIGURES 1-5).
For confirmation, aspirate was obtained from the cystic lesions which showed very high levels of pancreatic enzymes.
Discussion
Pancreatic pseudocyst is a well-known complication of acute and chronic pancreatitis where there occurs a collection of inflammatory exudates surrounded by a wall of fibrous or granulation tissue.
About 80% of the cases are located in the head and body of the pancreas while around 20% are found in extrapancreatic locations like mediastinum, liver, pelvis, pleura and spleen. However intrahepatic pseudocyst is a rare complication of pancreatitis with only 34 such cases being reported in English literature till the year 2009 [1,2]. Around 1 in 100 cases of pancreatic pseudocyst show extension into spleen [3].
Intrahepatic psudocysts have been postulated to occur by two basic pathophysiologic mechanisms. The first mechanism leading to development of subcapsular pseudocyst in left lobe of liver occurs due to accumulation of the pancreatic juice in the lesser sac, which then tracks along lesser omentum or gastrosplenic ligament into the liver. The second mechanism is associated with tracking of collection from the head of the pancreas along the hepatoduodenal ligament into the porta hepatis resulting in an intraparenchymal collection [1,4].
Several mechanisms have also been proposed underlying the formation of splenic pseudocyst. One of which involves tracking of pancreatic enzymes along the splenic hilar vessels. Other mechanisms include direct erosion of splenic capsule with isolated pseudocyst formation and due to pancreatitis of ectopic pancreatic tissue located in splenic parenchyma [3].
Clinically patient usually presents with abdominal pain, palpable abdominal lump, jaundice, fever and leucocytosis.
On Ultrasonography, features of acute or chronic pancreatitis can be detected along with a hypoechoic or anechoic collection with low level internal echoes which represents the pseudocyst.
On contrast-enhanced CT scan, pseudocyst appears as a well-defined round to oval hypodense collection with homogenous low internal attenuation surrounded by a welldefined enhancing wall. On evaluation with MR imaging, well-circumscribed unilocular lesion showing hypointensity on T1 weighted imaging and hyperintensity on T2 weighted imaging is detected. In addition MRI can better detect the vascular complications like pseudoaneurysm and venous thrombosis [3].
For confirmation of pancreatic origin, detection of elevated amylase and lipase levels in aspirated fluid is most useful [5,6].
Most of the pancreatic pseudocysts resolve spontaneously without any specific treatment. However, drainage may be required when symptoms appear due to compression of adjacent organs appear or when complications like rupture, infection or bleeding arise [6,7].
Conclusion
No definite guidelines have been formulated for the treatment of intrahepatic pseudocysts. They can be drained surgically, percutaneously or by endoscopy [8]. Small splenic cysts are managed conservatively and larger ones by endoscopic drainage, percutaneous catheter drainage or splenectomy [3].
References
- Noor T, Sandeep G, Arup B. A rare case report of hepatic sub capsular pseudocyst of pancreas. J. Clin. Diagn. Res. 10, PD18-PD19 (2016).
- Guesmi F, Zoghlami A, Saidi Y et al. Pancreatic pseudocysts located in the liver: A systematic review of the literature. Tunis. Med. 87, 801-804 (2009).
- Sunder G, Snigdha G, Mohinder G et al. Pseudopancreatic cyst invasion into spleen: Case report and review. Journal. of. Mahatma. Gandhi. Institute. of. Medical. Sciences. 19, 2 (2014).
- Folco S, Stuart M. Intrahepatic pseudocyst complicating acute pancreatitis: Imaging findings. AJR. Am. J. Roentgenol. 165, 873-874 (1995).
- Lyngdoh M, Prasant B, Pranjal P et al. Intrahepatic pseudocyst complicating acute pancreatitis: A rare case report. Int. J. Biomed. Adv. Res. 7, 300-301 (2016).
- Mayank D, Santosh S, Shipra S. A rare case of pancreatic pseudocyst involving liver and spleen. Inter. J. Med. Sci. Res. Pract. 2, 150-152 (2015).
- Cheruvu CV, Clarke MG, Prentice M et al. Conservative treatment as an option in the management of pancreatic pseudocyst. Ann. R. Coll. Surg. Engl. 85, 313-316 (2003).
- Parveen H, Sagar T, Prasant S et al. Rare case of intrahepatic pancreatic pseudocyst misdiagnosed as hepatic abscess. Int. J. Adv. Integr. Med. Sci. 1, 191-193 (2016).