Case Report - International Journal of Clinical Rheumatology (2021) Volume 16, Issue 6
A case of neurofibramatosis presenting with jaccoud arthropathy
- *Corresponding Author:
- Muhammet Limon
Division of Rheumatology, Selcuk University School of Medicine, Selcuklu, Konya, Turkey
E-mail: dr_mlimon@hotmail.com
Abstract
Jaccoud artropathy is a syndrome that is characterized by progressive, painless and reversible deformities involving especially the hands. Jaccoud artropathy may occur idiopathicallly as well as being associated with rheumatological diseases, lung malignancy, infections and Parkinson’s disease. Neurofibromatosis is a genetic chilhhood disease which presents with skin, eye, neurological and musculokeletal system manifestations. So far, no case of coexistence of neurofibromatosis and Jaccoud artropathy has been reported. This case is presented due to establishment of Jaccoud arthropathy in a patient with the diagnosis of neurofibromatosis.
Keywords
jaccoud arthropathy • hand deformity • neurofibromatosis
Introduction
Jaccoud Arthropathy (JA) was originally described with acute rheumatismal fever and subsequently associated with other rheumatological diseases. In JA, hyperextension develops in proximal interphalangial joints, and hyperflexion in distal interphalangial joints. JA may occur idiopathically as well as being associated with rheumatological diseases,lung malignancy, infections (HIV) and Parkinson’s disease. Neurofibromatosis is a genetic disease of chilhdhood presenting with dermatological, neurological, ophtamological and musculo skeletal system findings.
Neurofibromatosis type-1 (NF1, von Recklinghausen disease) is a congenital neurocutaneous syndrome that can involve nervous system, bone, endocrine glands and other organs. NF type 1, occurs once every 2500 to 3000 births and defect at 17q11.2 gene has been incriminated for this disease. Its cardinal findings are ; neurofibromas, ‘cafe au lait' spots, axillary -inguinal freckles and iris hamartomas (Lisch nodules). 30% to50% of neurofiromatosis type 1 cases develops due to spontaneous mutation. The rest are autosomal dominant. Patients are diagnosed in chilhdhood espeicallly with cafe au lait spots on skin and neurofibromas, which are the earliest signs. Diagnosis is made when at least two of diagnostic criteria developed in 1988 and updated in 1997 by NIH consensus concference are met. In NF1,skeletal system abnormalities such as osteopenia, scoliosis, sphneoid dysplasia, congenital tibia dysplasia and pseudoarthrosis may occur. Cafe au lait spots are the earliest and most consistent symptoms. Neurofibromas commonly emerge on the body after the age of 10. In NF1, Lisch nodules occur at the rates of 10%, 50% and 100% respectively around the ages of 6, 30 and 60. One of the clinical characteristics of Neurofibromatosis type 1 is that the rate of benign and malignanat tumors increase. To our knowledge, so far no case of coexistence of neurofibromatosis with Jaccoud arthropathy has been reported. This case is presented due to the establishment of JA in a patient with the diagnosis of neurofibromatosis.
Case
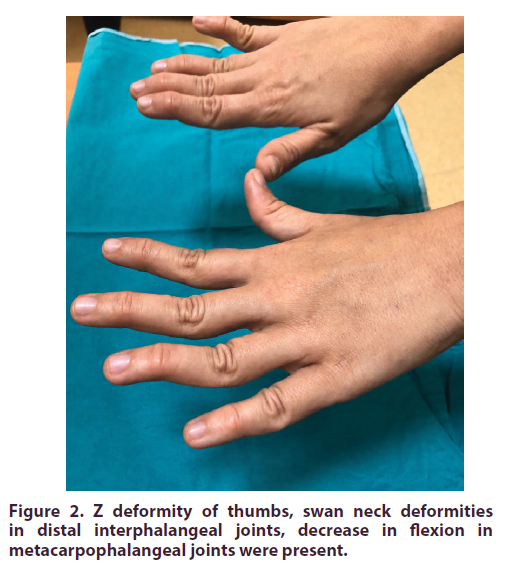
A 24-year-old female patient with known Neurofibromatosis type-1(NF1) diagnosis, presented to rheumatology outpatient clinic with complaints of deformity in her fingers. It was learned that finger deformity started two years ago and progressed in time. It was not accompanied by pain and stiffness. In family history, her father had a diagnosis of NF1. In physical examination, no pathology was found in vital findings and systemic examination but ‘cafe au lait' spots were observed in axillary region and trunk and neurofiboma was detected behind the ear (Figure 1). There was no arthritis in musculo-skeletal system examination. Z deformity of thumbs, swan neck deformities in distal interphalangeal joints, decrease in flexion in metacarpophalangeal joints were present, suggesting JA (Figure 2). Bilateral hand graphy corroborated non erosive diseae. In addition, patient had scoliosis as well. In eye examination, Lish nodules were detected. Laboratory examination results were as follows: Leucocyte:7200 K/Ul,neutrophil: 4200 K/Ul, hemoglobin: 13.1 gr/dl,thrombocyte: 247.000 K/Ul, creatinine: 0,4 mg/dl, CRP: 1mg/L (N:0-8), sedimentation: 2 mm/h. Among autoimmune markers, ANA, RF and anti –CCP were found to be negative. Anti-HIV was negative. In bilateral hand graphy, no erosion was detected and with thoraco-lumbar graphies, scoliosis was confirmed. Orthopedic surgery was planned due to scoliosis. Patient was kept under clinical follow up.
Discussion
JA, is a clinical condition characterized by reversible joint deformities such as swan neck, thumb subluxation, ulnar deviation, 'boutonniere' and hallux valgus along with lack of joint erosions in plain graphy. It was first defined by François-Sigismond Jaccoud in 1869 in a young patient with rheumatismal fever and chronic joints deformities. JA has been described to ocur in association with some other disorders, especially Systemic Lupus Erythematosus (SLE). Although less commonly, it has also been associated with scleroderma, Sjögren’s syndrome, vasculitis, psoriatic arthritis, reactive arthritis, ankylosing spondylitis, calcium pyrophosphate deposition disease among rehumatological diseases and was detected even in normal individuals. JA may also be associated with lung malignancy, inflammatory bowel disease, infections (HIV), and Parkinson’s disease [1-5]. In a study carried out in Brazil in 2006, JA incidence was found to be 2.8% in SLE [6]. In a different case series, the incidence of Jaccoud arthropathy was found to be % 3.47 in SLE patients [7]. JA is marked by a deforming arthropathy which can mimic clinical presentataion of RA: Although JA may involve all joints, it mostly presents with ulnar deviation, swan neck and boutonniere deformities, and Z-deformity of thumb, more than one non erosive subluxation along with serious deformations in hands. Subluxation in all MKP joint and ulnar deviation is usually the first sign and swan neck and boutonniere and Z-deformities may arise at later stages. In general, JA is not characterized by erosion or bone destruction in plain radography, unlike rheumatoid arthritis. However, novel imaging modalities usch as magnetic resonance and high performance ultrasonography revealed the presence of small erosions in the joints of a few patients with JA. Pathophysiology of JA still remains unknown. Deformities in JA are secondary to soft tissue abnormalities and include joints laxity, capsule fibrosis, synovitis tenosynovitis and muscular imbalance. Whether joint hypermobility contributes to development of JA is debatable. At present, JA treatment is conservative and is based on the use of non steroid anti inflammatory drugs, low dose corticosteroids, methotraxate, and antimalarial drugs. Surgery may play role in treatment by realignment of soft tissue around joint or by more agressive procedures such as arthrodesis, silastic implant and arthroplasty. In cases with hallux valgus, osteotomy or resection can be carried out at metarsal head. In patients with metacarpophalangial joint fusion, joint functions may be improved with implant placement.
To date, coexistence of neurofibromatosis and Jaccoud arthropathy has not been reported. As mentioned before, this is the first reported case of association of Neurofibromatosis with JA. As other similar cases emerge, this issue will be elucidated further.
References
- Bittl JA, Perloff JK. Chronic post-rheumatic fever arthropathy of Jaccoud. Am. Heart. J. 105(3), 515–517 (1983).
- Van Vugt R, Derksen R, Kater L et al. Deforming arthropathy or lupus and rhupus hands in systemic lupus erythematosus. Ann. Rheum. Dis. 57(9), 540–544 (1998).
- Johnson J, Leonard-Segal A, Nashel D. Jaccoud's-type arthropathy: an association with malignancy. J. Rheumatol. 16(9), 1278–1280 (1989).
- Bradley J, Pinals R. Jaccoud's arthropathy in scleroderma. Clin. Exp. Rheumatol. 2(4), 337–340 (1984).
- Maher J, Strosberg J, Rowley R et al. Jaccoud's arthropathy and inflammatory bowel disease. J. Rheumatol. 19(10), 1637–1639 (1992).
- Caznoch C, Esmanhotto L, Silva M, Skare T. Pattern of joint involvement in patients with systemic lupus erythematosus and its association with rheumatoid factor and hypermobility. Rev. Bras. Reumatol. 46(4), 261–265 (2006).
- Santiago MB, Galvao V. Jaccoud arthropathy in systemic lupus erythematosus: analysis of clinical characteristics and review of the literature. Medicine. 87(1), 37–44 (2008).