Case Report - International Journal of Clinical Rheumatology (2021) Volume 16, Issue 1
A case of neonatal lupus erythematosus presenting as hypopigmented atrophic scars
- Corresponding Author:
- Hendra Gunawan
Department of Dermatology and Venereology
Faculty of Medicine, Universitas Padjadjaran
Dr. Hasan Sadikin General Hospital, Bandung, Indonesia
E-mail: h.gunawan2016@unpad.ac.id
Abstract
Background: Neonatal Lupus Erythematosus (NLE) is a variant of lupus erythematosus that affects neonates. Cutaneous manifestation is one of the most common clinical manifestations in NLE, including erythematous macules and patches. Hypopigmented atrophic scar is a rare cutaneous manifestation of NLE. Case Report: A case of NLE in a 19-day-old female infant, who was born from asymptomatic first gravida mother was reported. Physical examination showed hypopigmented atrophic scars on the scalp, face, neck, chest, and back. Results of Antinuclear Antibody (ANA) panel from this patient revealed +++ for anti-Ro/SSA, anti-La/SSB, and anti-Ro-S2 recombinant antigens, whereas ANA test from her mother was reactive with a speckled pattern. These findings supported the diagnosis of NLE. Conclusion: Several cutaneous manifestations can present in NLE with hypopigmented atrophic scars as rare presentation. The diagnosis of NLE is an important marker for the asymptomatic mothers, who have a tendency to develop autoimmune diseases.
Keywords
anti-Ro/SSA • anti-La/SSB • atrophic scar • cutaneous manifestation • neonatal lupus erythematosus
Abbreviations
ANA: Antinuclear Antibodies; ENA: Extractable Nuclear Antigen antibodies; MCH: Mean Corpuscular Hemoglobin; MCHC: Mean Corpuscular Hemoglobin Concentration; MCV: Mean Corpuscular Volume; NLE: Neonatal Lupus Erythematosus; RBC: Red Blood Cell count; SLE: Systemic Lupus Erythematosus; TPHA: Treponema Pallidum Hemagglutination Assay; VDRL: Venereal Disease Research Laboratory; WBC: White Blood Cell count
Introduction
Neonatal Lupus Erythematosus (NLE) is a rare autoimmune disease that affects neonates and estimated to occur in 1 in 20.000 live births [1]. The clinical manifestations of NLE are usually characterized by cardiac abnormalities or cutaneous lesions or both. Therefore, the diagnosis of NLE should be suspected in neonates with total heart block or typical cutaneous lesions for NLE, or both, especially if the mother has autoimmune diseases [2]. On the other hand, the diagnosis of NLE is important because it can be a risk indicator for the asymptomatic mothers, who have a tendency to develop autoimmune diseases. Approximately 40-60% of mothers who gave birth to NLE neonates were asymptomatic [3], but half of those mothers would subsequently develop symptoms of autoimmune diseases later on in average of three years’ time [4,5]. Several cutaneous manifestations can present in NLE, such as annular or polycyclic erythematous macules and patches with or without fine scales, petechial hemorrhage, persistent cutis marmorata, and discoid lesion [2]. Telangiectasia and atrophic scars are unusual cutaneous manifestations of NLE [1,6]. Herein, we report a rare case of NLE with hypopigmented atrophic scars as predominant cutaneous manifestation.
Case report
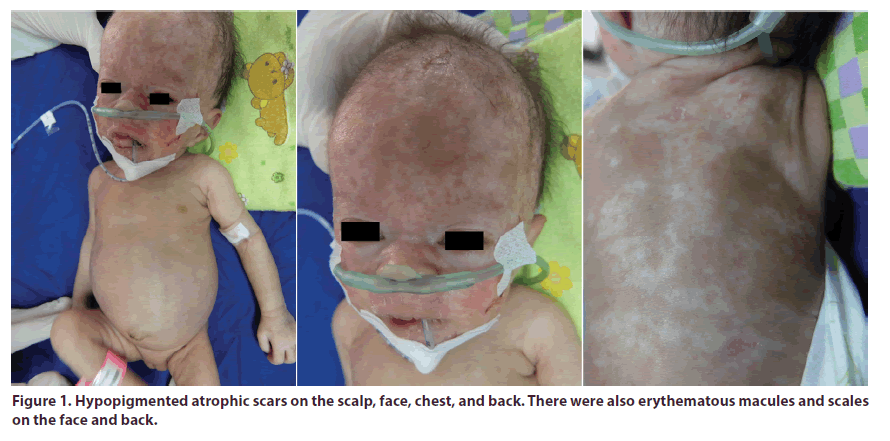
A 19 day-old female infant was consulted to the dermatology and venereology clinic because of the appearance of skin lesions right at birth. The skin lesions progressively increased in size. She was a first child, with birth weight of 1.3 kg, born prematurely at eight months gestational age by spontaneous delivery because of premature rupture of membrane. Physical examination showed predominant irregular hypopigmented atrophic scars on the scalp, face, chest, and back. There were also erythematous macules and scales on the face and back (Figure 1). There were no erosions, bullae, or nail abnormalities.
The laboratory examinations revealed thrombocytopenia without anemia (Table 1). The Antinuclear Antibody (ANA) panel examinations showed anti-Ro/SSA +++, anti-La/SSB +++, and anti-Ro-S2 recombinant +++. The Venereal Disease Research Laboratory (VDRL) and Treponema Pallidum Hemagglutination Assay (TPHA) tests were non-reactive.
Table 1. Complete blood count.
| Lab | Result | Reference Value |
|---|---|---|
| WBC | 6.3 | 5 - 20 thou/mcL |
| RBC | 5.15 | 3.90 - 5.50 thou/mcL |
| Hemoglobin | 16.6 | 13.5 - 19.5 g/dL |
| Hematocrit | 49 | 42% - 60% |
| MCV | 110.2 | 98 - 118 fL |
| MCH | 37 | 31 - 37 pg |
| MCHC | 34 | 30% - 36% |
| Platelet | 11 | 150 - 450 thou/mcL |
WBC: White Blood Cell count; RBC: Red Blood Cell count; MCV: Mean Corpuscular Volume; MCH: Mean Corpuscular Hemoglobin; MCHC: Mean Corpuscular Hemoglobin Concentration
The results of electrocardiography and head ultrasonography were within normal limit. A skin biopsy was not feasible due to the parent’s refusal. The mother had no other signs or symptoms of SLE but she had a positive ANA test with a speckled pattern. Based on those findings, the diagnosis of NLE was established. Treatment with moisturizer was prescribed to this patient.
Discussion
Neonatal lupus erythematosus is caused by the passage of maternal ANA and Extractable Nuclear Antigen antibodies (ENA) through placenta [3,4]. The important ENA in the pathogenesis of disease are anti-Ro/SSA, anti-La/SSB, and less frequently anti-U1 Ribonucleoprotein (RNP). These antibodies cross the placenta and damage the fetal tissue that caused manifestations in the neonates. Beside maternal antibodies, environmental factors and fetal genetics components may contribute to the pathogenesis of NLE [2]. Anti-La/SSB antibodies influence the development of cutaneous NLE; while anti-Ro/SSA antibodies are involved in the development of NLE with complete heart block. Several reports from the Research Registry for Neonatal Lupus/US indicate that the ratio between girls and boys is 2:1 with cutaneous NLE [3].
Cutaneous manifestation in NLE is about 40% [5], which may present at birth (20%) or in the first three months of life [1,2]. The mean duration of the rash is 15- 17 weeks. The rash of NLE tends to be photosensitive, but it can occur in non-sun exposed areas [4]. Periocular erythema or “raccoon eyes” is a characteristic of cutaneous manifestation in NLE [1,5]. Wisuthsarewong et al. [2] reported in their study that cutaneous manifestation in NLE were erythematous patches (91,7%), subacute cutaneous lupus erythematosus (50%), petechial hemorrhage (41,7%), persistent cutis marmorata (16,7%), and discoid lesions (8,3%). Perez et al. [1] stated that the purplish, atrophic telangiectasia and erythema multiforme-like lesions were rare cutaneous manifestations in NLE. To the best of our knowledge, there are only a few reports that described atrophic scars, especially hypopigmented atrophic scars in NLE [6-10]. The presence of atrophic scars at birth is thought to be the result of inflammatory insult in utero, but the pathogenesis of this phenomenon remain unknown [11].
The typical cardiac involvement of NLE is congenital Complete (third-degree) Heart Block (CHB) [1,5]. Hematologic abnormality occurs in 27% NLE patients [4] and thrombocytopenia has been the most frequently noted hematologic abnormality and may occur in about 10% of cases [1]. Neurologic manifestations also can occur in NLE, such as macrocephaly with or without associated hydrocephalus [2,5]. There was no abnormality in electrocardiography and head ultrasonography examination on this patient, which indicated that there were no cardiac and neurological involvements. Nevertheless, there was thrombocytopenia in this patient that indicated a hematological involvement. The cutaneous manifestation may resolve spontaneously by 6-12 months of age with the disappearance of maternal antibodies [4]. NLE patients presenting with cutaneous manifestation should avoid exposure to direct sunlight. In some cases, topical steroids are needed to reduce the evolution to atrophy, but systemic steroids are not indicated in NLE [3]. Therefore, we did not provide any therapy other than moisturizer to this patient because the skin lesions were already atrophy. The prognosis of NLE is determined by the presence of cardiac involvement, because most of the other manifestations are self-resolving [1,5]. Cardiac abnormalities are usually irreversible and the mortality rate is 20% [1,2,4].
The risk for mothers who have already had one neonates with NLE having an affected baby in subsequent pregnancy are 36%. A mother with a previous neonate with cutaneous NLE can have a subsequent neonate with congenital heart block and vice versa. Hence, weekly to every other week fetal echocardiograms between 16 and 26 weeks gestational age are recommended for those mothers [4].
Conclusion
Neonatal lupus erythematosus has several cutaneous manifestations, but predominant hypopigmented atrophic scar is a rare clinical presentation. The diagnosis of NLE is an important marker for the asymptomatic mothers, who have a tendency to develop autoimmune diseases.
Acknowledgments
All authors would like to thank to all Department of Dermatology and Venereology Faculty of Medicine, Universitas Padjadjaran-Dr. Hasan Sadikin General Hospital, Bandung, Indonesia staffs.
Funding
None.
Competing and conflict of interests
The author reports no conflicts of interest in this work.
Ethical statement
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
References
- Perez MF, Bujan MM, Cervini AB et al. Neonatal lupus erythematosus: a report of four cases. An. Bras. Dermatol. 86(2), 347-351 (2011).
- Wisuthsarewong W, Soongswang J, Chantorn R. Neonatal lupus eruthematosus clinial character, investigation, and outcome. Pediatr. Dermatol. 28(2), 115-121 (2011).
- Savino F, Viola S, Tarasco V et al. Neonatal lupus erythematosus: A cutaneous cases based update. Ital. J. Pediatr. 42, 1 (2016).
- Paller AS, Mancini AJ. Collagen Vascular Disorders. Hurwitz clinical pedatric dermatology: A textbook of skin disorder of childhood and adolescence. 5th Edn. Edinburgh: Elsevier. Pp, 505-507 (2016).
- Vanoni F, Lava SAG, Fossali EF et al. Neonatal systemic lupus erythematosus syndrome: A comprehensive review. Clinic. Rev. Allerg. Immunol. 53(3), 469-476 (2017).
- Khurana A, Maria A, Sardana K et al. Congenital scars: a rare presentation of neonatal lupus. Arch. Dis. Child. Fetal. Neonatal. Ed. 104(6), F630 (2019).
- Salman A, Sarıçam MH, Yücelten AD et al. Neonatal lupus erythematosus: Report of a case with cutaneous, hematological and hepatobiliary findings. Turk. J. Pediatr. 58(1), 106–108 (2016).
- Bhatt TA, Fatani HA, Mimesh S. Congenital lupus erythematosus. Indian. J. Dermatol. 56(6), 734–736 (2011).
- Crowley E, Frieden IJ. Neonatal lupus erythematosus: an unusual congenital presentation with cutaneous atrophy, erosions, alopecia, and pancytopenia. Pediatr. Dermatol. 15(1), 38–42 (1998).
- Saoji V, Deopujari S. Neonatal lupus erythematosus-three different presentations. Indian. J. Pediatric. Dermatol. 15(3), 110-113 (2014).
- Levy R, Briggs L, Silverman E et al. Cutaneous Sequelae in Neonatal Lupus: A Retrospective Cohort Study. J. Am. Acad. Dermatol. 83(2), 440-446 (2019).