Research Article - International Journal of Clinical Rheumatology (2017) Volume 12, Issue 2
25-hydroxyvitamin D3 deficiency and vitamin D receptor polymorphisms in Egyptian patients with BehÃÆçetâÃâ¬Ãâ¢s disease: a pilot study
- *Corresponding Author:
- Zeinab Al-Nahas
Internal Medicine Department
Cairo University, Egypt
E-mail: zeinab.elnahas@gmail.com
Abstract
Background: We investigated serum levels of 25-hydroxyvitamin D3 and the vitamin D receptor (VDR) gene polymorphisms (Fokl, Bsml) in Egyptian patients with Behçet’s disease (BD) and their relationship to disease manifestations and activity. Methods: We studied 45 patients with BD fulfilling the international study group criteria ISG for BD (1999) and 45 healthy, matched controls. We evaluated VDR Fokl, BsmI gene polymorphisms using polymerase chain reaction and restriction enzyme cleavage. Findings: The serum levels of 25-hydroxyvitamin D3 were lower in BD group than control group (P=0.006). When the BD group was compared to the control group, vitamin D3 deficiency (<20 ng/ml) was 6.7% vs. 0%; respectively (P=0.012), and vitamin D3 insufficiency (20- 30 ng/ml) was 77.6% vs. 60%; respectively (P=0.012). Among BD group, Bsml genotype was more associated with BD than FokI genotype. Furthermore, Bsml genotype frequencies were homozygous BB (33.3%) and heterozygous Bb (60%). There was no significant relation between 25-hydroxyvitamin D3 levels and active clinical manifestations of BD. Also, we did not detect any correlation between 25-hydroxyvitamin D3 levels and disease activity, or duration of illness. Bb and Ff genotypes were associated with vitamin D3 deficiency and insufficiency in BD group (P<0.001, 0.001 respectively). Conclusion: lower serum level of 25-hydroxyvitamin D3 might be a modifiable risk factor or consequence of BD. Polymorphisms in the VDR gene also are associated with susceptibility to BD which could be related to the immunomodulatory action of vitamin D. Further larger cohorts for genome wide association studies are required.
Keywords
behcet’s disease, vitamin D deficiency, behcet’s disease activity, vitamin D receptor, gene polymorphisms
Introduction
Behçet’s disease is a chronic multisystem inflammatory disorder of auto-inflammatory/ auto-immune nature. The exact etiology of BD is unknown, genetics, perhaps in conjunction with infectious agent(s), seems to play a critical role in disease susceptibility and development [1]. Vitamin D has long been recognized to be important for bone health and turnover. Vitamin D plays a major role in biologic activities including cellular proliferation and differentiation, immune system modulation and muscle strengthening. It is hypothesized that vitamin D is an environmental factor important in the etiology of T-cell-mediated autoimmune diseases [2]. The biological effect of vitamin D is thought to take place by binding to its receptor (VDR) which belongs to the steroid receptor superfamily. VDR gene polymorphisms lead to functional differences in the immuno-modulatory action of vitamin D. VDR is widely expressed in many cell types including antigen-presenting cells and lymphocytes [3]. The VDR gene is located in the human 12q12-q22 region and contains more than 470 single nucleotide polymorphisms (SNPs), some of which modulate 1,25 dihydroxyvitamin D3 uptake. The most common polymorphisms (SNPs) of the VDR include rs2228570 (FokI) in exon 2 and rs1544410 (BsmI) located in the intron separating exons 8 and 9 [4]. The immunomodulatory effect of 1,25-(OH)2D3 was demonstrated in a human monocyte in vitro model. It works through the down-regulation of TLR2 and TLR4. Do et al. showed that 25 (OH)D levels are inversely correlated with the expressions of TLR2 and TLR4. Furthermore, recent studies showed there is decrease in Vitamin D levels in BD patients [5]. The aim of our study is to investigate serum levels of vitamin D and the most common polymorphisms of the VDR gene in Egyptian patients with BD and to evaluate their relationship to disease manifestations and activity.
Materials and methods
This is a cross-sectional case control study including forty-five consecutive Egyptian BD patients fulfilling the International Study Group Criteria for BD (ISG 1990) [6]. All patients were recruited from our dedicated Behçet’s disease and Vasculitis outpatient clinic, as well as the Internal Medicine inpatient department, Cairo University Hospitals (Kasr Al Ainy Hospital). Forty-five healthy age and sex matched control individuals were included in this study.
The study was approved by local Ethic Committee of Faculty of Medicine, Cairo University. Informed consent was obtained from all participants.
Patients with other types of illness affecting vitamin D (namely chronic liver, kidney diseases, familial hypercholesterolemia, thyroid and parathyroid diseases, type 1 diabetes mellitus, other autoimmune diseases and malignancy) were excluded from this study. Also patients taking medications known to influence vitamin D metabolism as anticonvulsants; antihypertensive drugs such as diuretics, and calcium channel blockers were also excluded from this study.
All participants were subjected to the following:
• Full medical history and complete physical examination were done with special interest on Behcet’s disease symptoms and ophthalmologic evaluation including slit lamp examination.
• Pathergy Test: It was performed in all patients by intradermal puncture under the forearm skin with 20-gauge needle, 5 mm deep, obliquely under sterile conditions. It is considered positive if a papule or pustule formation on the area was observed after 24-48 h at the needle prick site in the skin [7].
• Assessment of disease activity: Behcet’s disease activity index (BDAI) was performed to all our patients according to the method presented by Bhakta et al. [8].
• Our patients were divided into 2 groups: Active group who had two or more symptoms with worsening of clinical symptoms and lack of wellbeing at time of study and inactive group who had no symptoms regarding BD activity for four weeks or less than 2 symptoms with a healing process and an overall wellbeing status.
• Duplex and colored coated Doppler examination on arterial & venous systems were done when indicated to detect arterial or venous occlusions.
Laboratory investigations
Total serum 25-hydroxyvitamin D (vitamin D)
It was measured in sera of all patients and controls using Enzyme -Linked- Immunosorbent Assay (ELISA). The kit provided by Sunred biocompany (Shanghai, China). This ELISA kit is based on the principle of double antibody sandwich technique to detect human vitamin D.
Vitamin D levels lower than 20 ng/ml were ascribed to “vitamin D deficiency” category. Vitamin D levels higher than 20 ng/ml and lower than 30 ng/ml were ascribed to “vitamin D insufficiency” and higher than 30 ng/ml of vitamin D were considered “Normal”.
VDR Fokl, bsmi gene polymorphisms evaluation
Using polymerase chain reaction and restriction enzyme cleavage, DNA was extracted from whole blood using DNA extraction kit and stored at -80°C in aliquots until required. This was done using Qia-amplification extraction kit (Qiagene, USA). The FokI polymorphism in exon 2 and BsmL polymorphism in intron 8 were determined by using specific primers. Genomic DNA template mixed with forward and reverse of each specific primers and DNA polymerase. Denaturation at 95°C for 3 min followed by PCR reaction was carried out for 35 cycles. Detection of PCR amplification products using gel electrophoresis and ultra-violet light transillumination.
• The 265 bp PCR product of FokI was digested with FokI restriction endonuclease overnight at 37°C. The digested products were separated on 4% agarose gel with ethidium bromide staining and ultraviolet trans illumination. The FF genotype (homozygote of common allele) lacked a FokI restriction site and showed 2 bands of 196 and 69 bp. The heterozygote displayed three fragments of 265, 196 and 69 bp, designated as Ff.
• After amplification of the BsmL gene, the PCR product 850 bp was digested with restriction endonuclease BsmL enzyme after incubation at 37°C overnight and electrophoresed in a 4% agarose gel containing ethidium bromide and then visualized by UV transilluminator. Subjects homozygote for the BSMI restriction site are designated bb and show two fragments at 650 and 200 bp while homozygous for the absence of the site are designated BB and give one band at 850 bp and the heterozygote type gives three bands.
Statistical methods
Quantitative variables were presented in terms of mean ± SD, median and range, or frequencies and percentages when appropriate. Comparison of numerical variables between the study groups was done using Student t test for independent samples in comparing 2 groups when normally distributed and Mann Whitney U test for independent samples when not normally distributed. Comparison of numerical variables between more than two groups was done using Kruskal Wallis test. For comparing categorical data, Chi square (χ2) test was performed. Exact test was used instead when the expected frequency was less than 5. p values less than 0.05 was considered statistically significant. All statistical calculations were done using computer program SPSS (Statistical Package for the Social Science; SPSS Inc., Chicago, IL, USA) release 15 for Microsoft Windows (2006).
Results
45 BD patients (38 males and 7 females) with mean age of 34.3 years (range from 21-54 years) and 45 healthy controls (37 males and 8 females) with mean age of 33.6 years (range from 21-54). BDAI with mean of 2.3 ± 1.2 SD (range 0-5). Based on their clinical activity 35 patients had active disease while 10 patients had inactive disease. Their disease duration ranged from 12 to 192 months with median interquartile range (IQR) 52.5 months.7 patients out of 45 BD patients had positive family history (15.6%).
Twelve patients had active ocular manifestations (26.6%); (7 patients had uveitis “5 posterior and 2 anterior”, 3 patients had retinal vascilitis, 2 patients had vitritis). Eight patients had active vascular affection (17.7%); (3 had DVT, 1 had thrombophlebitis, 1 had SVC thrombus, 1 had left atrial thrombosis, 1 had Budd Chiari syndrome and 1 had pulmonary aneurysm). Two patients had acute CNS affection (4.4%) (Table 1).
| Clinical manifestation | BD patients (no=45) | |
|---|---|---|
| Number | (%) | |
| Oral aphthous ulcers# | 23 | 51.1 |
| Genital ulcers | 10 | 22.2 |
| Erythema nodosum | 3 | 6.7 |
| Papulopustular lesions | 10 | 22.2 |
| Ocular lesions | 12 | 26.6 |
| Vascular lesions | 8 | 17.8 |
| Arthralgia/arthritis | 2 | 4.4 |
| CNS lesions | 2 | 4.4 |
| Positive pathergy test | 25 | 55.6 |
Table 1. Clinical manifestations of our BD patients. CNS: Central Nerves System, #Oral ulceration occurred in all patients throughout the course of the disease but some patients had no ulcer at the time of examination.
Twenty eight (62.2%) out of the 45 patients, were on steroids and its dose ranged from 5 to 30 mg per day, 33 patients (73.3%) were on colchicine with a dose that ranged from 1.0 to 1.5 mg per day and 14 patients (31.1%) were on azathioprine and its dose ranged from 100 to 150 mg per day.
Among our BD patients, 3 (6.7%) had vitamin D3 deficiency, 35 (77.8%) had vitamin D3 insufficiency. Meanwhile in control group, 27 (60%) had vitamin D3 insufficiency and none had vitamin D3 deficiency. These findings indicate a prevalence of vitamin D deficiency and insufficiency among BD patients (P<0.012). Average level of vitamin D in BD cases and healthy controls were 26.5 ± 9.1 and 35.7 ± 19.5 ng/ml respectively (P<0.006) (Table 2).
| Total serum Vitamin D3 | Controls Number (45) |
BD patients Number (45) |
|
|---|---|---|---|
| P value | 0.006 | ||
| Controls | Patients | ||
| Vitamin D3 | Sufficient (>30 ng/dl) |
18 (40%) | 7 (15.6%) |
| Insufficient (20-30 ng/dl) |
27 (60%) | 35 (77.8%) | |
| Deficient (<20 ng/dl) |
0 | 3 (6.7%) | |
| P value | 0.012 | ||
Table 2. Comparison between BD patients and controls as regard serum 25-hydroxyvitamin D3 (vitamin D3).
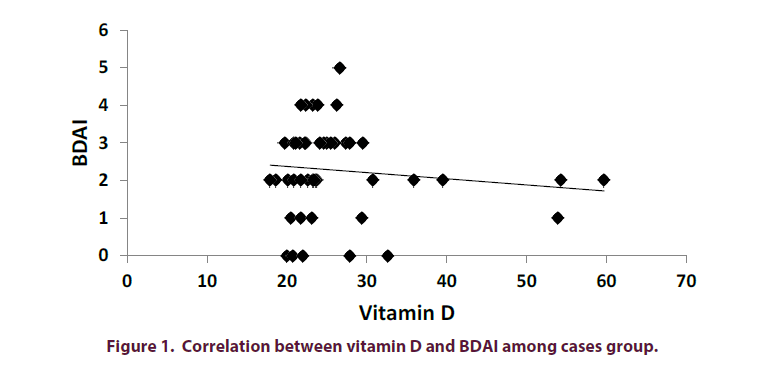
Also among BD patients, males were significantly having lower levels of vitamin D3 than females with a P value of 0.004. There was no statistical significant difference between Vitamin D3 levels and patients with active clinical manifestation (oral, genital ulcers, ocular, vascular, cutaneous lesions and pathergy test). Also no correlation between serum vitamin D3 levels and patients who were on steroids, azathioprine and colchicine. There was no correlation between vitamin D3 levels and disease activity, BDAI, age and duration was present (Figure 1).
On the contrary, there was no contribution of the VDR polymorphisms FokI to BD. FokI genotype frequencies for BD patients and control group were FF:Ff:ff=46.7%:48.9%:4.4% and 37.8%:44.4%:17.8% respectively (P=0.128). Also the frequency of F and f allele in patients and controls was similar at 71.1:28.9% and 60%:40%, respectively.
BsmI genotype frequencies for the BD and control groups were BB:Bb:bb=33.3%:60%:6.7% and 15.6%:44.4%:40%, respectively, (P=0.001). Also, with prevalence of BB and Bb in BD patients. In addition, the frequency of the B and b alleles in our BD patients was 63.3%:36.7%, respectively compared to 37.2%:62.2%, respectively (Table 3).
| Genotype frequency | P-value | Allele frequency | ||||
|---|---|---|---|---|---|---|
| FokI | FF | Ff | ff | F | f | |
| Patients | 46.7% | 48.9% | 4.4% | 0.128 | 71.1% | 28.9% |
| Controls | 37.8% | 44.4% | 17.8% | 60% | 40% | |
| Bsml | BB | Bb | bb | B | b | |
| Patients | 33.3% | 60% | 6.7% | 0.001 | 63.3% | 36.7% |
| Controls | 15.6% | 44.4% | 40% | 37.2% | 62.2% | |
Table 3. Comparison of genotype and allele frequencies for the FokI and Bsml VDR polymorphisms between patients and controls.
We also found a high statistically significant association between vitamin D deficient and insufficient BD patients and specific genotypes Bb and Ff with a P value <0.001, 0.001, respectively. Also no correlation between disease activity and VDR polymorphisms was present (Table 4).
| Vitamin D3 | P-value | ||||
|---|---|---|---|---|---|
| Sufficient | Insufficient | Deficient | |||
| FokI | FF | 71.4% | 45.7% | 0% | 0.001 |
| Ff | 0% | 54.3% | 100% | ||
| ff | 28.6% | 0% | 0% | ||
| Bsml | BB | 57.1% | 28.6% | 33.3% | <0.0001 |
| Bb | 0% | 71.4% | 66.7% | ||
| bb | 42.9% | 0% | 0% | ||
Table 4. Vitamin D3 and the FokI and Bsml, VDR polymorphisms in BD patients.
Discussion
Behçet’s disease (BD) is a chronic autoimmune relapsing disease which involves multiple systems [9]. One of the essential attributes of vitamin D is its immunoregulatory role [5]. Therefore vitamin D deficiencies need to be comprehensively addressed in patients with immunologic disturbances. The optimum serum level of vitamin D which facilitates efficient immune responses is not precisely determined. However it is believed to be lower than its required level in healthy bone metabolism [10].
Hypovitaminosis D was encountered in 33-50% of general population in Sub-Saharan Africa and Middle East. Vitamin D deficiency is considered a global public health concern which affects various age groups [11].
Vitamin D has a key role of in the pathogenesis of autoimmune disorders, and the evidences linking vitamin D status as a potential environmental factor involved in autoimmune disease continue to accumulate.
Vitamin D supplementation has been found to be of therapeutic benefit in animal models of autoimmune disease, including in autoimmune encephalomyelitis, collagen-induced arthritis, type 1 diabetes mellitus, inflammatory bowel disease, autoimmune thyroiditis and systemic lupus erythematosus [12].
In our work, we carried out a comparative study between BD patients and control group as regard the total serum 25-hydroxyvitamin D (vitamin D). It showed a statistical significant difference between both groups in prevalence of vitamin D deficiency and insufficiency within BD patients (p=0.012).
Several studies are in agreement with our results regarding the different levels of vitamin D between BD patients and controls as Karatay et al. [13] who investigated 31 patients with BD, vitamin D levels were significantly lower in the patient group than in the control group (p=0.001), Ganeb et al. [14] who investigated 42 patients with BD, where there was a statistically significant decrease in serum vitamin D levels (p=0.02) and Khabbazi et al. [15] who investigated 48 patients with BD, and demonstrated a statistically significant lower serum vitamin D levels (p=0.0001) ) in patients compared to controls.
Faezi et al. [16] who investigated 112 patients with BD, showed disagreement with our study results as they found that vitamin D deficiency was significantly more common in controls than cases group (P<0.001). This controversy may be explained by the fact that they excluded BD cases with severe activity in their study and also patients and controls were gathered at different time frames.
Also in our study, BD male patients had lower levels of total serum 25-hydroxyvitamin D than female patients (p=0.004) which was in agreement with Faezi et al. who also found lower levels in males than females (p= 0.039). Contrary to our findings Khabbazi et al. [15] and Hamzaoui et al. [17] found no significant difference in vitamin D levels between the male and female BD patients.
Also in our study, there was no relationship between 25(OH) D levels and disease activity and active clinical manifestations in BD patients. The same results were shown by Khabbazi et al. [15] and Faezi et al. [16]. Contrary to our findings Ganeb et al., [14] found a statistically significant decrease of vitamin D serum levels in BD patients with vascular lesions (p= 0.001). Hamzaoui et al. [17] also who reported lower levels of vitamin D in BD active patients compared to patients with inactive disease; those who had no symptoms related to BD in a fourweek period, or less than two symptoms with a healing process and an overall well-being status (p=0.024).
In our study, there was no difference between serum vitamin D levels in patients who were on steroids, azathioprine or colchicine and those who did not receive these medications. These results agree with Ganeb et al. [14].
Although recognized as an autoimmune disease, BD is classified among the inflammatory diseases. Its etiopathogenesis involves the T cells; the immune cells capable of producing the VDR protein. Any alteration in the VDR protein may directly influence T-cell proliferation, inducing a Th1/Th2 imbalance, thereby triggering an excessive and uncontrolled immune response responsible for inflammation [18].
The BsmI and FokI polymorphisms have an important role in the function of the VDR receptor. The FokI polymorphism located in exon 2 is linked to a second methionine start site, leading to the formation of a shorter protein receptor that has greater transcriptional activity than the wild type receptor. The BsmI polymorphism can be linked to a variablelength polyadenylate sequence within the 3′-untranslated region. The level of VDR mRNA was significantly decreased in patients with the VDR B allele versus those not bearing the B allele [19].
Bsml genotype frequencies for the BD and control groups had a highly statistically significant difference with a P value 0.001. The BB and Bb genotypes were significantly associated with BD. In addition, the B allele frequency of 63.3% was present in BD patients compared to 37.2% of controls. To the contrary, there was no contribution of the VDR polymorphism FokI to BD with a P value of 0.128.
In contrast to our results, Khodadadi et al. [20] who studied VDR polymorphisms in 50 BD patients from Iranian Azari, found that the ff genotype was significantly associated with BD (P=0.04) and the f allele frequency of 26% was present in BD patients. Also Karraya et al. [21] who studied VDR polymorphisms in 135 BD patients from Tunisia, found that The FF genotype was significantly associated with BD (p= 0.002) and the F allele was found in 68.8% of BD patients.
Similarly, several studies done in an Egyptian population to investigate VDR polymorphisms with other autoimmune diseases were in agreement with our result. Hussien et al. [22] (Zagazig) investigated rheumatoid arthritis patients with and without osteoporosis, they found that bone mineral density (BMD) was lower in individuals with the BB genotype in RA patients with osteoporosis (P=0.0001) suggesting an association of the B allele with increased osteoclastic activity in RA patients.
Our findings were similar to results of studies done in other autoimmune diseases in different populations where they found association of BsmI VDR polymorphism in autoimmune thyroid diseases in China, MS in northwest Greece and BsmI polymorphism with lupus and MS in Iran, lupus in Thailand, type 1 diabetes mellitus in Portugal. However, In Taiwanese and Chinese populations, the B allele of the BsmI VDR polymorphism was significantly associated with lupus. In contrast to the BsmI VDR polymorphism, the FokI polymorphism was associated with type 1 diabetes mellitus in Italy and with autoimmune Addison’s disease in Germany [20].
Also, it seems that environmental factors which influence levels of active vitamin D are complex and a significant difference exists between vitamin D functions and VDR polymorphisms. The association between VDR polymorphisms and autoimmune diseases may vary across different ethnic populations [20].
Bsml and Apal restriction site polymorphisms occur in the intron separating exons VIII and IX. A T/C nucleotide substitution (ATT to ATC) leading to a synonymous change at codon 352 (isoleucine) in exon IX and is detected by the restriction enzyme Taql. More attention is focused on the possible role of these variants in the development of auto inflammatory and other diseases related to the immune system. Diseases associated with these polymorphisms may therefore be better explained by linkage disequilibrium with other functional variation within the VDR gene or with another closely linked gene or genes [23].
We also found a high statistically significant association between vitamin D deficient and insufficient BD patients and specific genotypes Bb and Ff with a P value <0.001, 0.001, respectively.
The FokI polymorphism of the VDR gene has two variants differing from each other by three amino acids: the f/ M1 variant has 427 amino acids and the F/M4 variant 424 amino acids. The shorter (F/M4) receptor includes about 65 percent of VDR gene alleles in human subjects, accordingly, the FokI variant remains a candidate functional polymorphism; the f allele isoform interacts with the basal transcription factor less efficiently than does the F allele isoform, providing a possible mechanism for the reduced trans-activation associated (connected) with this allele [18].
Also, Colin et al. [24] confirming the higher activity of the 424 aa short VDR variant, found that phytohemoglutinin stimulated the growth of peripheral blood monocytes differs according to Fokl polymorphism. They found that the one-half maximal concentration for 1α,25 (OH)2 vitamin D inhibition of phytohemoglutinin-stimulated growth was noticeably higher for cells containing the full-length VDR isoform (i.e., Ff and ff genotypes) than for those with the shorter isoform (FF genotype).
Conclusion
This study demonstrated that serum levels of vitamin D were significantly lower in BD patients. Bsml genotype frequencies are significantly associated with BD in Egypt. Our findings suggest that vitamin D may contribute to the pathogenesis of BD through its role as immunomodulatory or might be a consequence of BD.
To the best of our knowledge, this is the first study that investigates VDR polymorphisms in BD patients in Egypt. However, our study has the unavoidable limitation of number since it was conducted on a small number of Egyptian patients with BD from Cairo University Hospitals as a pilot study. For future studies we recommend enrolling a larger number of Egyptian BD patients from different geographic locations as a multi-centre national study. Also, international studies of BD patients from different countries are required. This will provide data on genetic relationships with VDR polymorphisms and statistically empowered results on such a relationship.
Conflict of interest
All the authors declare that they have no conflict of interest.
References
- Carapito R, Shahram F, Michel S et al. On the genetics of the Silk Route: association analysis of HLA, IL10, and IL23R-IL12RB2 regions with Behçet’s disease in an Iranian population. Immunogenetics. 67, 289–293 (2015).
- Haroon M, Bond U, Quillinan N et al. The prevalence of vitamin D deficiency in consecutive new patients seen over a 6-month period in general rheumatology clinics. Clin. Rheumatol. 30, 789–794 (2011).
- Morgan JW, Kouttab N, Ford D et al. Vitamin D mediated gene regulation in phenotypically defined B cell subpopulation. Endocrinology. 141, 3225–3234 (2000).
- Mostowska A, Lianeri M, Wudarski M et al. Vitamin D receptor gene BsmI, FokI, ApaI and TaqI polymorphisms and the risk of systemic lupus erythematosus. Mol. Biol. Rep. 40, 803–810 (2013).
- Do JE, Kwon SY, Park S et al. Effects of vitamin D on expression of Toll-like receptors of monocytes from patients with Behcet's disease. Rheumatology. 47, 840–848 (2008).
- International Study Group for Behcets disease. Criteria for diagnosis of Behcets disease. Lancet. 335, 1078–1080 (1990).
- Sequeira FF, Daryani D (2011) The oral and skin pathergy test. Indian. J. Dermatol. Venereol. Leprol. 77, 526–530 (2011).
- Bhakta BB, Brennan P, James TE et al. Behcet’s disease: evaluation of a new instrument to measure clinical activity. Rheumatology. 38, 728–733 (1999).
- Pineton de Chambrun M, Wechsler B, Geri G, Cacoub P, Saadoun D. New insights into the pathogenesis of Behçet's disease. Autoimmun. Rev. 11, 687–698 (2012).
- Kamen DL, Cooper GS, Bouali H et al. Vitamin D deficiency in systemic lupus erythematosus. Autoimmun. Rev. 5, 114–117 (2006).
- Arabi A, El Rassi R, El-Hajj FG. Hypovitaminosis D in developing countries-prevalence, risk factors and outcomes. Nat. Rev. Endocrinol. 6, 550–561 (2010).
- Booth DR, Ding N, Parnell GP et al. Cistromic and genetic evidence that the vitamin D receptor mediates susceptibility to latitude-dependent autoimmune diseases. Genes. Immun. 17, 213–219 (2016).
- Karatay S, Yildirim k, Karakuzu A et al. Vitamin D status in patients with Behcet’s Disease. Clinics. 66, 721–723 (2011).
- Ganeb S, Sabry H, Alassal M et al. (2013) Vitamin D levels in patients with Behcet’s disease: Significance and impact on disease measures. The Egyptian Rheumatologist 35, 151–157 (2013).
- Khabbazi A, Rashtchizadeh N, Ghorbanihahjo A et al. The status of serum vitamin D in patients with active Behcet’s disease compared with controls. Int. J. Rheum. Dis. 17, 430–434 (2014).
- Faezi ST, Ansari N, Paragomi P et al. (2014) Vitamin D deficiency in patients with Behcet's disease. J. Diabetes. Metab. Disord. 13, 18 (2014).
- Hamzaoui K, Dhifallah IB, Karray E, Sassi FH, Hamzaoui A. Vitamin D modulates peripheral immunity in patients with Behcet’s disease. Clin. Exp. Rheumatol. 28(4 Suppl 60), S50–S57 (2010).
- Jurutka PW, Remus LS, Whitfield GK et al. The polymorphic N terminus in human Vitamin D receptor isoforms influences transcriptional activity by modulating interaction with transcription factor IIB. Mol. Endocrinol. 14, 401–420 (2000).
- Monticielo OA, Brenol JC, Chies JA et al. The role of BsmI and FokI vitamin D receptor gene polymorphisms and serum 25-hydroxyvitamin D in Brazilian patients with systemic lupus erythematosus. Lupus. 21, 43–52 (2012).
- Khodadadi H, Khabazi A, Ghaderian S et al. Molecular analysis of vitamin D receptor gene polymorphisms rs2228570 (FokI) and rs1544410 (BsmI) in patients with Behcet’s Disease. Life. Sci. J. 10(4) (2014).
- Karraya EF, Dhifallaha IB, Abdelghanib KB et al. Associations of vitamin D receptor gene polymorphisms FokI and BsmI with susceptibility to rheumatoid arthritis and Behcet’s disease in Tunisians. Joint. Bone. Spine. 79, 144–148 (2012).
- Hussien YM, Shehata S, Karam RA et al. Polymorphism in vitamin D receptor and osteoprotegerin genes in Egyptian rheumatoid arthritis patients with and without osteoporosis. Mol. Biol. Rep. 40, 3675–3680 (2013).
- McCullough ML, Bostick RM, Mayo TL. Vitamin D gene pathway polymorphisms and risk of colorectal, breast and prostate cancer. Ann. Rev. Nutr. 29, 111–132 (2009).
- Colin EM, Asmawidjaja PS, van Hamburg JP et al. 1,25-Dihydroxyvitamin D3 modulates Th17 polarization and interleukin-22 expression by memory T cells from patients with early rheumatoid arthritis. Arthritis. Rheum. 62, 132–142 (2010).