Case Report - Imaging in Medicine (2017) Volume 9, Issue 5
The radiological features of tracheal rupture following endotracheal intubation
Carina Aguilar, Fidel Rampersad* & Aaron Baldeo SinghRadiology Unit, University of the West Indies (St Augustine), Trinidad & Tobago
- Corresponding Author:
- Fidel
Rampersad
Radiology Unit
University of the West Indies (St Augustine)
Trinidad & Tobago
E-mail: fidelrampersad@gmail.com
Abstract
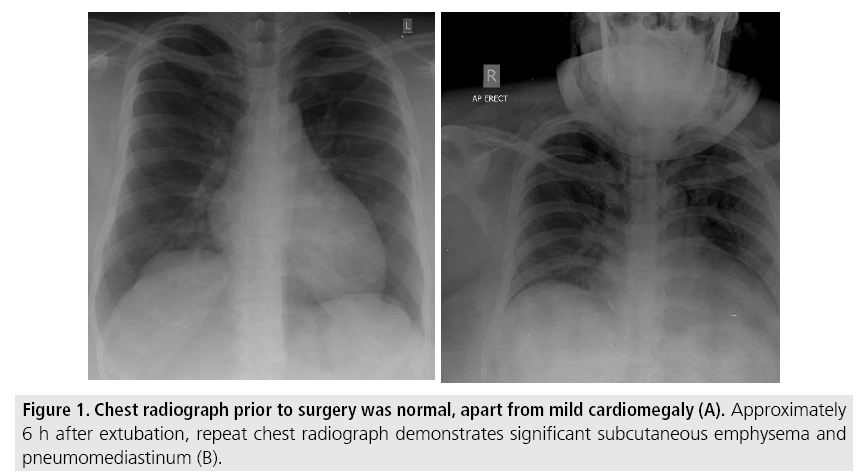
We present a case study of a 30 year old female patient who experienced excessive retching and vomiting. This occurred after receiving oral fluids 5h after receiving general anaesthetic for an elective orthopaedic surgical procedure (open reduction and internal fixation for a right proximal radial fracture). The pre-procedure chest radiograph prior to surgery was normal. A chest radiograph performed 6 hours after extubation showed significant subcutaneous emphysema within the neck and upper chest, as well as pneumomediastinum. There was no evidence of oesophageal rupture on water-soluble contrast swallow. Multislice CT chest confirmed the presence of subcutaneous emphysema in the neck and chest and pneumomediastinum. Tracheal rupture was also demonstrated on CT and confirmed on flexible bronchoscopy. The patient had conservative management. Repeat flexible bronchoscopy approximately two weeks later showed healing of the tracheal tear. Repeat chest radiograph, two weeks later, showed no residual pneumomediastinum and almost complete resolution of the subcutaneous emphysema.
Keywords
tracheal rupture ▪ endotracheal intubation ▪ pneumomediastinum
Abbreviations
CT: Computed Tomography; PITR: Post Intubation Tracheal Rupture; AP: Anterior Posterior; LPO: Left Posterior Oblique
Background
Following the procedure of endotracheal intubation, tracheal rupture is a rare, but serious complication [1]. It usually presents as a linear lesion in the membranous wall of the trachea and is more prevalent in women and patients older than 50 years. The clinical manifestations of tracheal injury include subcutaneous emphysema and respiratory distress.
It is a life threatening complication that can also occur with blunt or penetrating trauma to the neck or chest.
Tracheal rupture can also result from bronchoscopy or other endoscopic interventions [1].
Post intubation tracheal rupture (PITR) can be due to tube tip positioning, cuff overinflation or by repositioning of the endotracheal tube without deflating the cuff [2].
PITR is uncommon, and has a mortality of 22% [3]. Early diagnosis and prompt management is important in view of the associated high morbidity and mortality. Prompt radiological evaluation determines the course of conservative versus surgical management.
■ Case presentation
A 30 year old woman experienced excessive retching and vomiting on the ward, after oral fluids were administered. This was done approximately 5 h after an elective orthopaedic procedure (open reduction and internal fixation surgery for a right proximal radial fracture), done under general anaesthesia, with endotracheal intubation.
On examination, there was neck swelling, with crepitus. The patient complained of difficulty breathing, with no signs of respiratory distress. Normal respiratory rate and oxygen saturation were noted. Chest radiography confirmed extensive subcutaneous emphysema and pneumomediastinum.
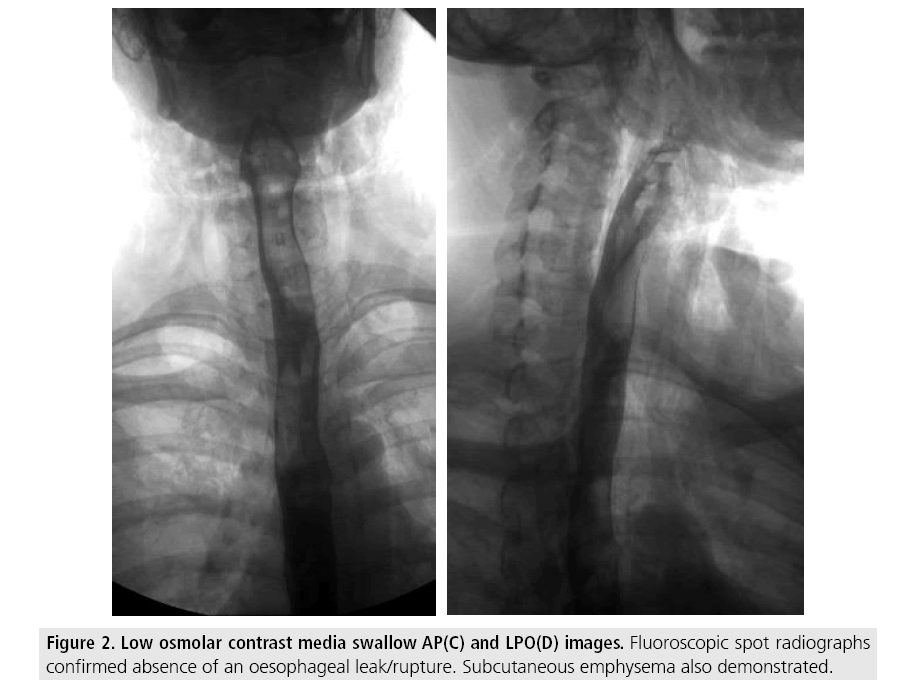
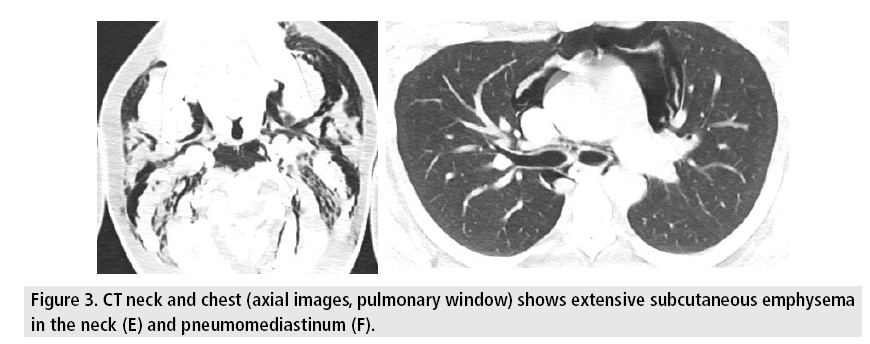
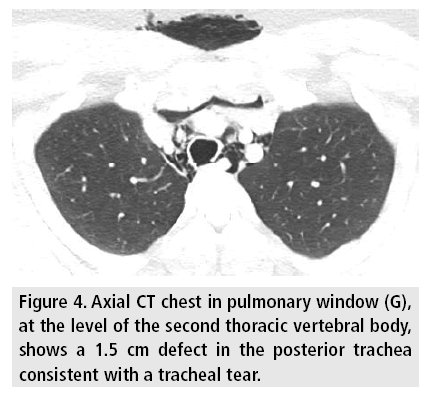
Low osmolar contrast media swallow, done under fluoroscopy, excluded an oesophageal leak/rupture. CT chest confirmed the presence of extensive subcutaneous emphysema of the neck and chest. Extensive pneumomediastinum was also noted. A posterior tracheal rupture was confirmed on CT at the level of the second thoracic vertebral body.
Flexible bronchoscopy confirmed a 3 cm left posterolateral partial thickness tear of the trachea, located approximately 5 cm from the carina (FIGURES 1-4).
Figure 1: Chest radiograph prior to surgery was normal, apart from mild cardiomegaly (A). Approximately 6 h after extubation, repeat chest radiograph demonstrates significant subcutaneous emphysema and pneumomediastinum (B).
Figure 2: Low osmolar contrast media swallow AP(C) and LPO(D) images. Fluoroscopic spot radiographs confirmed absence of an oesophageal leak/rupture. Subcutaneous emphysema also demonstrated.
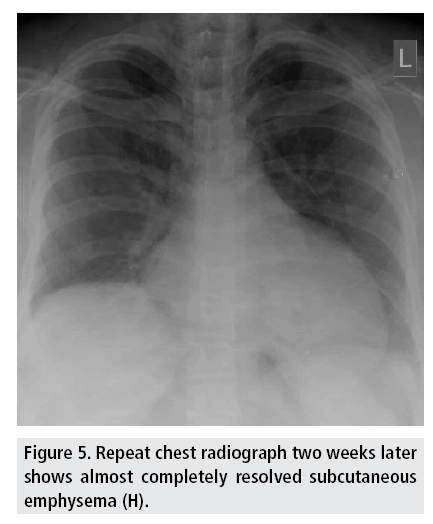
The conservative course of management was taken, with close monitoring by the anaesthetic and thoracic surgical team. Repeat flexible bronchoscopy done approximately two weeks later showed healing of the tracheal tear. There was almost complete resolution of the subcutaneous emphysema and complete resolution of the pneumomediastinum, on a follow up chest radiograph done after 2 weeks (FIGURE 5).
Discussion
The trachea commences at the level of the cricoid (at the level of the sixth cervical vertebral body) and bifurcates at the carina (at the level of the fifth thoracic vertebral body) and contains incomplete cartilaginous rings [4]. The posterior trachea is a fibrous membranous wall, known as the pars membranacea. PITR typically causes longitudinal lacerations of the pars membranacea, rarely extending into the main bronchi.
The presenting features of PITR are subcutaneous emphysema, pneumomediastinum, and pneumothorax [1].
Multi detector CT with thin slices, viewed in pulmonary (lung) window allows detailed assessment of the trachea and enables localization of the injury. Diagnosis can then be confirmed by bronchoscopy, allowing precise demarcation of location, extent, and depth of the PITR [5].
Surgical management is the mainstay of treatment. However, conservative management is considered in patients with rupture less than 2 cm and in selected stable patients with nonprogressive symptoms and with no air leakage on spontaneous breathing [1,5].
Clinical suspicion and early imaging (especially with CT) and bronchoscopy, is beneficial in patients with PITR. Avoidance of endotracheal cuff over-inflation is advised. Conservative management, rather than surgical repair, is advised in patients with a small tracheal defect and with favourable clinical presentation [1].
Acknowledgement
We would like to acknowledge the Patient, Nursing Staff, Anaesthetic Team and the Thoracic Surgical Team for their support in putting together this case study.
Consent
Patient consent was obtained but they choose to remain anonymous.
Funding
No funding was required for this case study.
Competing and conflicting interests
There was no competing and conflicting interest.
References
- Marty-Ane C, Picard E. Membranous tracheal rupture after endotracheal intubation. Ann. Thorac. Surg. 60, 1367-1371 (1995).
- Miñambres E, Burón J, Ballesteros MA et al. Tracheal rupture after endotracheal intubation: A literature systematic review. Eur. J. Cardiothorac. Surg. 35 (2009).
- Lim H, Kim JH, Kim D et al. Tracheal rupture after endotracheal intubation-A report of three cases. Korean. J. Anesthesiol. 62, 277-280 (2012)
- Gamsu G, Webb W. Computed tomography of the trachea: Normal and abnormal. Am. J. Roentgenol. 139, 321-326 (1982).
- Prunet B, Lacroix G, Asencio Y et al. Iatrogenic post-intubation tracheal rupture treated conservatively without intubation: A case report. Cases. J. 1, 259 (2008).