Editor Note - Interventional Cardiology (2017) Volume 9, Issue 5
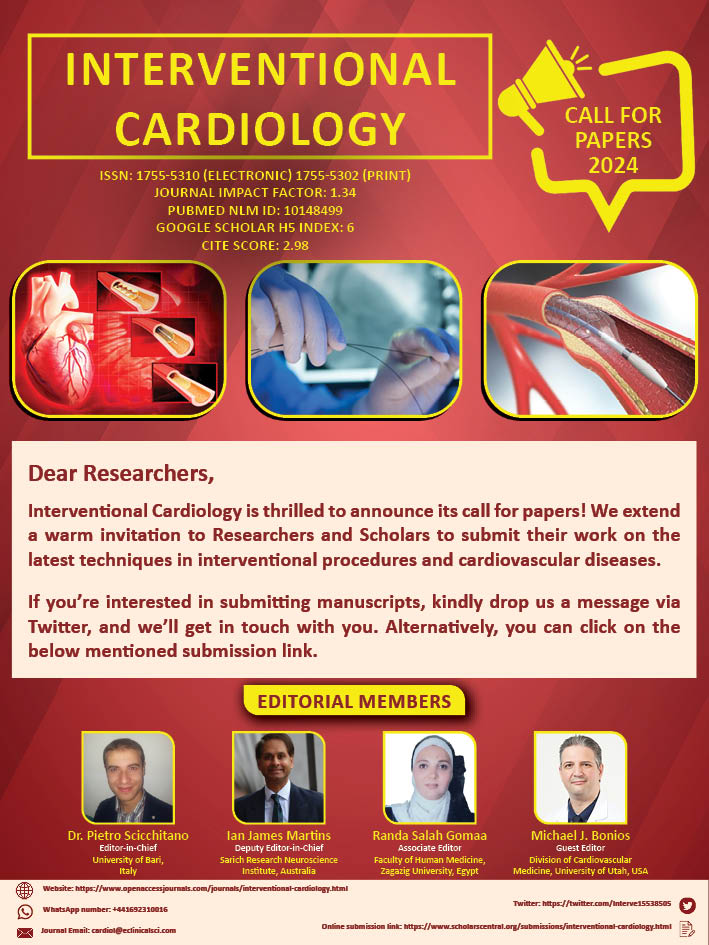
Interventional Cardiology-
- Corresponding Author:
- Ian B. A. Menown
Craigavon Cardiac Centre
Queen’s University, Belfast, UK
E-mail: ian.menown@southerntrust.hscni.net
Submitted: 13 October 2017 Accepted: 16 October 2017 Published online: 19 October 2017
Abstract
Introduction
The current issue of Interventional Cardiology, in keeping with its aim of focusing on state of the art interventional research and practice, showcases several novel studies and case reports. Slavin and Leifsson [1] investigated the relationship between Segmental arterial mediolysis (SAM) and mesangial hyperplasia. Roever et al. [2], investigated the prevalence of atherosclerosis risk factors and Metabolic syndrome (MetS) in urban Brazilian population. Sanoussi et al. [3], presented an extremely rare case of myocardial infraction associated tuberculous pericarditis effusion. Torres and Changlani [4] presented the case of coronary artery ectasia in a 73-year-old male having dyslipidemia, hypertension, and coronary artery disease. Brito and Carvalho [5] investigated the usability of Shared decision-making (SDM) in two scenarios: (1) medication for high cholesterol, and (2) bypass and/or angioplasty for coronary artery disease. Kováčik et al. [6], presented a case of cardiac amyloidosis. Sun and Lei [7] investigated the application of computed tomography pulmonary angiography (CTPA) in cases of suspected pulmonary embolism (PE).
Segmental arterial mediolysis (SAM) is a rare disease of the arteries which causes massive bleeding and/or ischemic symptoms. SAM is initiated as a result of the release of norepinephrine from the peripheral sympathetic nerves which innervate the arteries targeted in SAM. In addition to humans, SAM is also prevalent in dogs and pigs; in these animals, SAM is accompanied by mesangial cell hyperplasia. Slavin and Leifsson [1] investigated the relationship between SAM and mesangial hyperplasia. The authors found that the various stimuli at the root of SAM may also induce focal mesangial cell hyperplasia and contraction; thus, it can be inferred that SAM and mesangial cell hyperplasia have a shared pathogenesis.
Metabolic syndrome (MetS), an umbrella term encompassing risk factors such as high blood pressure, insulin resistance, high triglycerides, and pro-thrombotic tendency, is associated with an increased risk of stroke and cardiovascular disease. Metabolic syndrome is increasingly becoming more common globally, due to increasing obesity rates in adults. The high prevalence of MetS and associated risk factors in atherosclerosis may be associated with enhanced accumulation of perirenal and visceral fat deposits. Roever et al. [2], investigated the atherosclerosis risk factors and MetS in urban Brazilian population.
Pericardial effusion, one of the complications of myocardial infarction, is characterized by accumulation of fluid may present with congestive hepatomegaly, low volume pulse, raised jugular venous pressure, ascites and peripheral oedema. Sanoussi et al. [3], presented an case of tuberculous pericarditis effusion in the setting of acute myocardial infarction. The authors suggest that tuberculosis should be considered while making a differential diagnosis of myocardial infarction associated pericardial effusion in countries endemic for TB.
Aneurysmal coronary artery disease or coronary artery ectasia is defined as the dilation of a section of a coronary vessel more than 1.5 times the diameter of the adjacent arterial/vascular segments; and can be either discrete or continuous. Coronary artery ectasia is usually accompanied by coronary atherosclerosis;. The aneurysmal segments are known to cause turbulent or sluggish blood flow, and increase the incidence of ischemia. Torres and Changlani [4] presented the case of a 73- year-old male having dyslipidemia, hypertension, and coronary artery disease who had suffered from myocardial infarction 20 years ago. Heart catheterization revealed a fusiform aneurysm (14 mm) involving the entire left main (LM) coronary artery and many small aneurysms on the right coronary artery (RCA).
When considering treatment options for coronary artery disease (CAD), patients have to make a wide range of decisions in coordination with the primary care physicians. On their part, primary care physicians have to brief the patients about the risks, benefits, and alternative approaches of treatment, so that the patient can make an informed decision, keeping in mind the cost-to-benefit ratio. Shared decision-making (SDM) and enhancing patient involvement in the decision making process has gained a lot of interest in recent years. Brito and Carvalho [5] compared SDM in case of two disparate conditions: (1) medication for high cholesterol, and (2) bypass and/or angioplasty for coronary artery disease. The authors found that as compared with the cardiac procedures group, more individuals in the cholesterol medication group believed that the therapeutic decision was prominently theirs. Thus, the nature of a medical intervention significantly impacts the decision making patterns and preferences.
Amyloidosis is a systemic disease characterized by the excess production of amyloid, which are then deposited in the extracellular spaces of multiple tissues; amyloids can get accumulated in practically any organ of the body. The underlying reason behind amyloid formation and deposition has not yet been fully elucidated. The worldwide incidence of new amyloidosis cases is estimated at 8 to 10 cases per million per year. Amyloidosis may be (1) primary (AL), (2) secondary (AA), (3) familial, (4) senile, or (5) dialysis related. The prognosis of AL amyloidosis is dependent on the identity and number of affected organs and the severity of amyloid accumulation. The worst prognosis for amyloidosis is associated with cardiac involvement, which has a median survival, in untreated patients, of ~6 months from the initiation of congestive heart failure. Kováčik et al. [6], presented a case report of amyloid accumulation in the cardiac tissue.
Sun and Lei [7] investigated the application of computed tomography pulmonary angiography (CTPA) in cases of suspected pulmonary embolism (PE). Medical records of 450 patients with suspected PE who had undergone CTPA over a period of 6 months were reviewed. The study suggested that CTPA can diagnose PE with a high accuracy whereas triple rule-out computed tomography had a lower diagnostic yield.
References
- Slavin RE, Leifsson PS. Segmental arterial mediolysis with mesangial cell hyperplasia; A review with supplementary comments concerning its pathogenesis. Interv. Cardiol. 9(5): 181-190 (2017).
- Roever L, Resende ES, Diniz ALD, et al. Major risk factors for atherosclerosis and metabolic syndrome: The UHS. Interv. Cardiol. 9(5): 199-203 (2017).
- Sanoussi H, Kourireche N, Lakhal Z, et al. Tuberculous pericarditis: An exceptional STEMI association: Case report. Interv. Cardiol. 9(5): 205-208 (2017).
- Torres RJ, Changlani M. Coronary artery aneurysms in the elderly: Case report. Interv. Cardiol. 9(5): 211-214 (2017).
- Brito ATAB, Carvalho G. Does the type of treatment affect who makes the decision? Secondary data analysis of patients undergoing angioplasty vs. medical treatment for high cholesterol levels. Interv. Cardiol. 9(5): 215-221 (2017).
- Kovacik F, Taborsky M, Hutyra M, et al. Cardiac amyloidosis: case report. Interv. Cardiol. 9(5): 223-225 (2017).
- Sun Z, Lei J. Diagnostic yield of CT pulmonary angiography in the diagnosis of pulmonary embolism: A single center experience. Interv. Cardiol. 9(5): 191-198 (2017).