Case Report - International Journal of Clinical Rheumatology (2022) Volume 17, Issue 2
The prevalence of difficult airway indices in systemic sclerosis patients and their correlation with the modified Rodnan skin score
Reza Atef Yekta1*, Hoda Kavosi2, Ali Ghasemi3, Mahsa Najafi Kandovan3, Azin Etemadimanesh3, Zahra Tamartash2, Ali Javinani2, Seyedeh Zahra Fotook Kiaei4, Alireza Emamzade2, Amirmohammad Mohammadadegan2
1Department of Anaesthesiology at Tehran University of Medical Sciences, Tehran, Iran
2Rheumatology Research Center, Tehran University of Medical Sciences, Tehran, Iran
3Faculty of Medicine, Tehran University of Medical Science, Tehran, Iran
4Advanced Thoracic Research Centre, Tehran University of Medical Science, Tehran, Iran
- *Corresponding Author:
- Reza Atef Yekta
Department of Anaesthesiology at Tehran University of Medical Sciences, Tehran, Iran
E-mail: atefyekta@tums.ac.ir
Received: 02-Feb-2022, Manuscript No. fmijcr-22-53202; Editor assigned: 07-Feb-2022, PreQC No. fmijcr-22-53202(PQ); Reviewed: 20-Feb-2022, QC No. fmijcr-22-53202; Revised: 24-Feb-2022, Manuscript No. fmijcr-22-53202(R); Published: 28-Feb-2022, DOI: 10.37532/1758-4272.2022.17(2).039-045
Abstract
Introduction: Systemic sclerosis (SSc) is a chronic multisystem autoimmune disease characterized by skin stiffness with pulmonary and cardiovascular involvements, responsible for mortality in SSC patients. Preoperative management in SSc patients is critical to have a better operation result. Owing to possible complications of SSc, prediction of a difficult airway in these patients is fateful for proper airway management. The score of skin stiffness is evaluated by modified Rodnan skin score (MRSS). MRSS measures skin stiffness and has been widely utilized to assess the progression and severity of the disease. In this study, we aimed to investigate the prevalence of the difficult airway indices (DAIs) in SSc patients and evaluate the correlation between the DAIs and the MRSS.
Material and method: A total of 139 patients with a definite diagnosis of SSc based on the ACR/EULAR 2013 criteria were enrolled in this cross-sectional study. The DAIs included the modified Mallampati classification (MMC), 3-3-2 rule, mouth opening (MO), thyromental distance, finger to palm (FTP), upper lip bite test (ULBT), and prayer sign was measured in addition to MRSS.
Results: The median MRSS was 14. The most frequent DAIs among the patients was MMC (37.5%) and prayer sign (35.2%). The MRSS was significantly correlated with the 3-3-2 rule, MO, FTP, ULBT, and prayer sign. No significant correlation was seen between the disease duration and the recorded variables. Conclusion: In this study, we found that the MRSS is associated with DAIs making it a valuable asset in the preoperative evaluations of SSc patients.
Keywords: systemic scleroderma • intubation • airway management
Introduction
Systemic sclerosis is a chronic immunemediated multisystem disease characterized by fibrosis, vasculopathy and visceral manifestations. Systemic sclerosis patients experience several complications in their appearance and internal organs functions. Systemic sclerosis involves about 17 per 100,000 persons globally [1]. There is no treatment available to reverse or suppress disease complications and treatment goals are focused on symptoms control and improving organ functions [2].
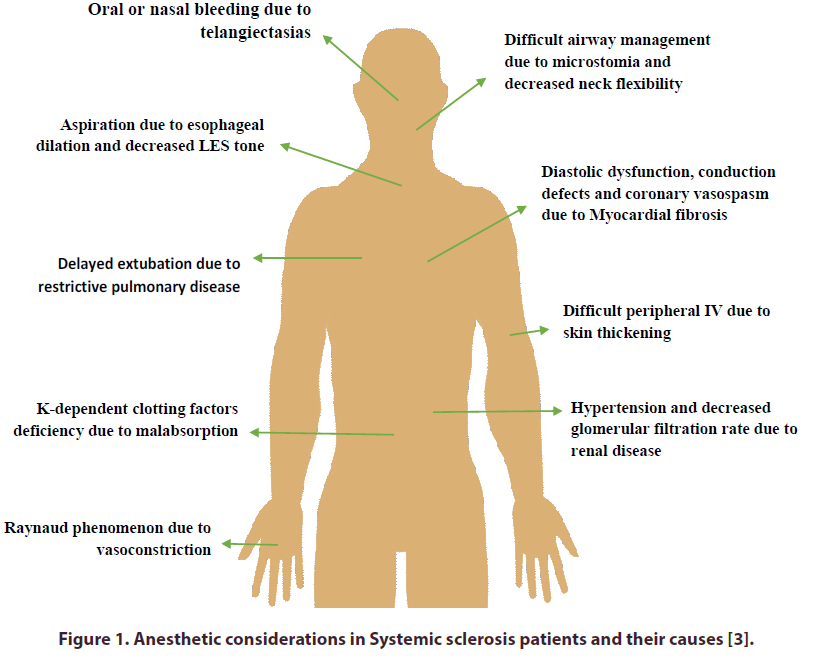
Anesthetic management of systemic sclerosis patients is a challenging subject due to their multiorgan involvements (Figure 1).
Some clinicians recommend regional anesthesia in these patients if applicable. But in case of need for general anesthesia and intubation, anesthesiologist may face with difficult airway and be enforced to use fiber optic, blind nasal or retrograde intubation techniques. Perioperative airway assessment is critical in systemic sclerosis patients due to microstomia -limited ability to open mouth-and cardiopulmonary involvement which makes direct laryngoscopy and ventilation more challenging [3-6]. There is limited evidence-based guidance for optimal preoperative assessment and intubation in these patients.
Different airway indices (DAIs) have been proposed for preoperative difficult airway evaluation, including: Modified Mallampati test (MMT), Prayer sign, Neck range of motion, Standard finger-to-palm (FTP) test, Thyromental distance (TMD), Mouth opening, Upper lip bite test (ULBT), and 3-3-2 rule [7- 10]. All of these indices are related to skin tightness and musculoskeletal wellbeing of patients and used as valid predictors for difficult airway incidence.
Extent of skin stiffness is commonly assessed with the modified Rodnan skin score (MRSS), an index that represents severity and activity of systemic sclerosis. MRSS is a semi-quantitative standard measure to score skin stiffness in 17 different body parts including fingers, hands, forearms, arms, face, upper and lower trunk, feet, legs, and thighs on a scale from 0 to 3 [11]. A higher MRSS score has a direct correlation with various internal organ involvements, particularly pulmonary complications [12]. Relationship between MRSS and difficult airway has not been addressed in previous studies.
Several papers have highlighted difficult airway management in systemic sclerosis patients [13-15]; nonetheless, there are no comprehensive studies on the frequency of DAIs and their relationship with other predictive indices in these patients. Bridging between systemic sclerosis severity indices and DAIs can guide us to a better understanding of difficult airway in these patients.
In the present work, we aimed to investigate the frequency of DAIs in systemic sclerosis patients and their relationship with disease severity and skin stiffness measured via MRSS.
Material and Methods
In this cross-sectional study, patients selected through a simple random sampling approach from the systemic sclerosis registry of the Rheumatology Research Center (RRC) at Shariati Hospital, Tehran, Iran.
All participants were previously diagnosed with systemic sclerosis by an experienced rheumatologist based on the 2013 classification criteria for systemic sclerosis: an American College of Rheumatology/ European League against Rheumatism (ACR/EULAR) collaborative initiative [16]. The patients were excluded from the study if they had prior head or neck trauma, localized scleroderma, overlap syndrome, BMI over 30 untrimmed facial hair or lacking natural teeth.
Written and verbal consent was obtained from all participants and patients were informed about details of study. Study protocol was approved by the Ethics Committee of Tehran University of Medical Sciences (code: IR.TUMS.MEDICINE.REC.1398.082).
Aim of the study was to describe prevalence of DAIs among systemic sclerosis patients and its probable relationship with skin stiffness caused by progression of the disease. Patients’ Demographic data and medical history were extracted from aforementioned data registry of patients, including age, gender, disease duration from the first non-Raynaud phenomenon, history of endotracheal intubation or sleep apnea. There were no data available about the incidence of difficult airway management for patients with previous intubation.
At first patients were examined by a rheumatologist for verification of the diagnosis and skin stiffness examination. Modified Rodnan skin score was recorded for each patient with an acceptable reliability coefficient over time (ICC=0.88) [17].
DAIs of all the patients were independently measured and recorded by an anesthesiologist at the same day. Evaluated DAIs included classification tests like modified Mallampati classification (MMC) and Upper lip bite test (ULBT), dichotomous tests like neck range of motion (RoM), prayer sign and 3-3-2 rule, and also mouth opening, thyromental distance and standard finger-to-palm were measured for all participants.
The MMC was evaluated by observability of faucial pillars, uvula, and soft palate without phonation, while the patient was in a sitting position with open mouth and protruded tongue. It classifies as followed and class III or IV were considered as positive DAIs:
• Class I: Soft palate, uvula, fauces, and pillars are visible.
• Class II: Soft palate, the major part of uvula, and fauces are visible.
• Class III: Soft palate and base of uvula are visible. • Class IV: Only the hard palate is visible [18].
The ULBT is the ability to bite the upper lip using lower teeth. It defines in three classes:
• Class 1: The patient can easily bite the upper lip.
• Class 2: The lower incisors barely touch the upper lip.
• Class 3: The lower teeth cannot reach the upper lip [19].
The neck RoM was assessed and recorded as either normal or limited range of motion. In the prayer sign test, the patient squeezed palms of both hands together. If the fingers were able to fully extend and the palms do not meet in the phalangeal joints, the test was considered positive. The 3-3-2 rule technique predicts the difficult intubation based on the following scales: 3, three fingers could easily pass between inter-incisor distances (IID); 3, the distance between the mentum and hyoid bone is equal to the width of three fingers; 2, the distance between hyoid-thyroid cartilages (HTD) is equal to the width of two fingers [20]. Limitation in any of them was considered as a positive DAI.
Mouth opening, thyromental distance - and standard finger to palm were measured in centimeter (cm) by a ruler.
Thyroid mental distance (TMD) is the distance from the mentum to the top of the thyroid cartilage cleft while the head is fully extended. TMD equal to 6.5 cm or more with no other anatomical abnormalities predicts easy intubation [21]. Standard Finger-To-Palm (FTP) measures the distance between the tip of the third finger and the distal palmar crease while all the fingers are fully flexed [22].
At the end, demographic data and prevalence of DAIs among patients described in detail. We also compared each of DAIs with patients’ MRSS, disease duration and history of intubation or sleep apnea to suggest the probable causes of positive DAIs among systemic sclerosis patients.
Statistical analysis
The continuous variables were tested for normal distribution with the Shapiro–Wilk test and presented as mean ± standard deviation or median and interquartile range. Consequently, the χ2 test was applied for the comparison of the categorical variables. To evaluate the correlation between the categorical and continuous variables, the Spearman rank correlation was performed. Ultimately, the P-values were adjusted via the Benjamini– Hochberg method for the false discovery rate, and the values below 0.05 were considered to be significant. All the statistical analyses were performed with the SPSS software for Windows version 25.0 (Armonk, NY: IBM Corp).
Results
At the end of study 139 systemic sclerosis patients were enrolled. The mean age of patients was 49 years old. Median disease duration was 7 years. History of sleep apnea and intubation was positive in 10 (7.2%) and 33 (23.74%) patients, respectively. Experience of difficult airway management during previous intubations was unclear. Median of patients’ MRSS during rheumatologic examination was 14 with an IQR25–75 of 10 to 20 (min-max: 0-48).
Between evaluated positive DAIs, modified Mallampati classes of III and IV were the most prevalent among a total of 52 (37.5%) patients; followed by prayer sign (35.2%) and 3-3-2 rule (17.3%). Table 1 depicts detailed results of all measured DAIs.
| Tests with classification | Class1 | Class2 | Class3 | Class4 | |
|---|---|---|---|---|---|
| Midified Mallampati (N) | 57 (41%) | 30 (21.5%) | 24 (17.3%) | 28 (20.2%) | |
| Upper lip bite test (N) | 90 (64.7%) | 36 (25.9%) | 13 (9.4%) | N/A | |
| Tests with dichotomous outcomes | Normal | Abnormal or Limited | |||
| Neck range of motion (N) | 133 (95.7%) | 6 (4.3%) | |||
| Prayer sign (N) | 90 (64.8%) | 49 (35.2%) | |||
| 3-3-2 rule (N) | 115 (82.7%) | 24 (17.3%) | |||
| Tests with continuous values | Median (IQR25–75) | ||||
| Mouth opening (cm) | 3.50 (3.5-4.0) | ||||
| Thyromental distance (cm) | 9.00 (8.0-9.5) | ||||
| Finger-To-Palm (cm) | 1.00 (0.0-2.0) | ||||
Table 1. Description of the difficult airway indices among 139 systemic sclerosis patients.
In the comprehensive analysis there was a significant correlation between MRSS and some DAIs including: ULBT (P=0.01), mouth opening (P-value:0.04), 3-3- 2 rule (P-value:0.007), standard FTP (P-value:0.002), and prayer sign (P-value:0.001). We could not find any correlation between patients MRSS and Modified mallampati classification, neck RoM and thyromental distance. Also, there was not any relationship between MRSS and previous history if sleep apnea and intubation.
Subsequently, correlation between the disease duration and DAIs was examined and could not find any correlation between the disease duration and DAIs (P-value >0.05) (Table 2).
| Index | Correlation with the disease duration | Correlation with the MRSS | ||||
|---|---|---|---|---|---|---|
| p-value | Spearman’s rho | adjusted p-value | p-value | Spearman’s rho | adjusted p-value | |
| Modified Mallampati (Classes III and IV) | 0.288 | -0.091 | 0.504 | 0.727 | 0.030 | 0.898 |
| Neck range of motion | 0.926 | 0.008 | 1 | 0.377 | 0.076 | 0.609 |
| Upper lip bite test (Class 3) | 0.035 | 0.179 | 0.122 | 0.002 | 0.256 | 0.010 |
| Mouth opening | 0.184 | -0.113 | 0.429 | 0.010 | -0.219 | 0.042 |
| 3-3-2 rule | 0.625 | 0.042 | 0.820 | 0.001 | 0.289 | 0.007 |
| Thyromental distance | 0.988 | -0.001 | 0.988 | 0.158 | -0.120 | 0.414 |
| Standard Finger-To-Palm | 0.200 | 0.109 | 0.420 | <0.001 | 0.380 | 0.002 |
| Prayer sign | 0.797 | 0.022 | 0.929 | <0.001 | 0.469 | 0.001 |
| History of intubation | 0.438 | -0.066 | 0.613 | 0.931 | -0.007 | 0.977 |
| History of sleep apnea | 0.382 | 0.075 | 0.573 | 0.209 | -0.107 | 0.399 |
| Modified Rodnan Skin score | 0.088 | -0.145 | 0.264 | N/A | N/A | N/A |
Table 2. Correlation between study parameters and the disease duration or MRSS with correction for multiple comparisons.
Discussion
Preoperative assessment of systemic sclerosis patients is essential to prevent failure of airway management due to their probable skin stiffness, microstomia and musculoskeletal complications. A better understanding of the difficult airway indices in systemic sclerosis patients with different disease severity can help anesthesiologists to be prepared and assemble the setting for the optimal management of difficult airway and predict the risk of airway management failure.
In the present study, we described the prevalence and distribution of DAIs among systemic sclerosis patients. Modified Mallampati classes of III and IV (37.5%), prayer sign (35.2%) and the 3-3-2 rule (17.3%) were the most prevalent DAIs in the study population, respectively; and the median TMD was 9 cm. Till now there are no comprehensive studies about the DAIs and their causes in systemic sclerosis patients; however, some studies reported the incidence rate of 17-19% classes of III or IV MMC among rheumatoid arthritis (RA) patients, and the mean TMD of 8.19 cm [23,24]. Two different studies among the normal population, reported the incidence rates of classes of III or IV MMC as 16.1% and 25.6% and average TMDs of 6.5 cm and 7.1 cm [25,26]. Based on the results of our study, Prevalence of MMC in systemic sclerosis patients is higher than the normal population and RA patients. Understanding the pattern of positive DAIs and their underlying causes can clarify the reasons behind these complications.
Despite the present lack of data about the prevalence of DAIs and their relationship with occurrence of difficult airway incidences in systemic sclerosis patients, some of these indices have been reported alongside difficult airway management in these patients, namely microstomia [4,13,26] and limited neck RoM [14,27]. A case report described a patient with difficult airway that was subsequently found to be an undiagnosed case of systemic sclerosis [14]. Further studies are needed to evaluate predictive value of each DAIs for difficult airways in systemic sclerosis patients.
The modified Rodnan skin score is a test that evaluates the skin stiffness and correlates with the severity of systemic sclerosis. It has been widely implemented for primary or secondary outcome measures for systemic sclerosis patients [11,28,29]. Accordingly, it has been shown that the skin sclerosis measured with MRSS is associated with more internal organ involvement, particularly interstitial lung disease and gastrointestinal dysmotility [30]. Similarly, a significant correlation has been reported between MRSS and musculoskeletal involvement in systemic sclerosis patients. Researchers reported a progressively rising mortality correlated with increased MRSS [31]. Investigating the relationships between MRSS and DAIs, can elucidate the role of systemic sclerosis severity and skin stiffness in causing difficult airway among these patients.
In our study, the median MRSS of the patients was 14.0. MRSS was significantly correlated with positive ULBT, mouth opening, 3-3-2 rule, standard FTP, and prayer sign. These results suggest that the upper airway deterioration coincides with the increase in skin stiffness and systemic sclerosis severity. It also highlights the importance of skin fibrosis in difficult airway assessment. Consequently, it seems that the MRSS can also be correlated with the severity of the upper airway and orofacial involvement among systemic sclerosis patients.
Our results revealed no significant correlations between the disease duration and the incidence of DAIs. It has been shown in previous studies that the MRSS not only does not increase over time but also fairly declines in patients receiving proper medical treatment [32]. The atrophic changes of the skin in the prolonged systemic sclerosis can be responsible for this discrepancy. It has been reported that 3 to 5 years after the disease onset, the skin stiffness incrementally improves [33,34]. There were no significant correlations between MRSS and the disease duration in the current study, as well; signifying that the younger patients with shorter disease duration or newly diagnosed systemic sclerosis patients should not be overlooked for the difficult airway assessments.
Preoperative management in systemic sclerosis patients should encompass thorough multi-system investigations. Considering the progressive internal organs involvement in systemic sclerosis patients, including cardiopulmonary and renovascular systems, preoperative and anesthetic management of these patients is already a challenging subject. Additionally, the involvement of skin and orofacial soft tissue renders intubation and airway management even more challenging and should be taken into account for better risk stratification. Therefore, rheumatologists and anesthesiologists should be more vigilant about the probable difficult airway in systemic sclerosis patients and arrange the proper requirements. The results of the present study simply showed that DAIs incidence is more frequent among systemic sclerosis patients compared to normal population and the more the skin stiffness and systemic sclerosis severity, the greater the chance of having a difficult airway. Anesthesiologists who prepare systemic sclerosis patients for operations under general anesthesia should focus on the skin stiffness and DAIs more precisely.
Our study had certain limitations, including the small sample size and no follow-ups in case the patients undergo general anesthesia. We suggest performing studies with long term follow-ups to evaluate the real incidence of difficult airway and its’ relative causes among systemic sclerosis patients to reach the best preoperative screening tools for these patients.
In conclusion, the findings obtained herein implied that the prevalence of DAIs in systemic sclerosis patients is higher than normal population and there may be a correlation between some DAIs and skin stiffness.
References
- Bairkdar M, Rossides M, Westerlind H et al. Incidence and prevalence of systemic sclerosis globally: a comprehensive systematic review and meta-analysis. Rheumatol. (2021).
- Kowal-Bielecka O, Fransen J, Avouac J et al. Update of EULAR recommendations for the treatment of systemic sclerosis. Annals of the rheumatic diseases. 76(8),1327-1339 (2017).
- Roberts JG, Sabar R, Gianoli JA et al. Progressive systemic sclerosis: clinical manifestations and anesthetic considerations. J Clin Anesth. 14(6),474-477 (2002).
- Shionoya Y, Kamiga H, Tsujimoto G et al. Anesthetic management of a patient with systemic sclerosis and microstomia. Anesth Prog. 67(1),28-34 (2020).
- Braun-Falco O, Plewig G, Wolff HH et al. Dermatology. Springer Science & Business Media. (2009).
- Crincoli V, Fatone L, Fanelli M et al. Orofacial manifestations and temporomandibular disorders of systemic scleroderma: an observational study. Int J Mol Sci.17(7),1189 (2016).
- Johnson C. A Comparison of the Upper Lip Bite Test (a Simple New Technique) with Modified Mallampati Classification in Predicting Difficulty in Endotracheal Intubation: A Prospective Blinded Study. Survey Anesth. 48(1),59 (2004).
- Khan ZH, Mohammadi M, Rasouli MR et al. The diagnostic value of the upper lip bite test combined with sternomental distance, thyromental distance, and interincisor distance for prediction of easy laryngoscopy and intubation: a prospective study. Anesth Analg. 109(3),822-824 (2009).
- Knudsen K, Högman M, Larsson A et al. The best method to predict easy intubation: a quasi-experimental pilot study. J Perianest Nurs. 29(4),292-297 (2014).
- Yu T, Wang B, Jin XJ et al. Predicting difficult airways: 3-3-2 rule or 3-3 rule? Irish Journal of Medical Science. 184(3),677-683 (2015).
- Khanna D, Furst DE, Clements PJ et al. Standardization of the modified Rodnan skin score for use in clinical trials of systemic sclerosis. J Scleroderma Relat Disord. 2(1),11-18 (2017).
- Ooi G, Mok MY, Tsang KWT et al. Interstitial lung disease in systemic sclerosis: An HRCT-clinical correlative study. Acta Radiologica. 44(3),258-264 (2003).
- Thompson J, Conklin KA. Anesthetic management of a pregnant patient with scleroderma. Obstetric Anesthesia Digest. 3(4),129 (1983).
- Kanter GJ, Barash PG. Undiagnosed scleroderma in a patient with a difficult airway. Yale J Biol Med. 71(1),31 (1998).
- D'Angelo R, Miller R. Pregnancy complicated by severe preeclampsia and thrombocytopenia in a patient with scleroderma. Anesth Analg. 85(4),839-841 (1997).
- Van den Hoogen F, Khanna D, Fransen J et al. Classification criteria for systemic sclerosis: an American College of 2013.
- Javinani A, Nejad ZJ, Gharibdoost F et al. Bundle Branch Blocks and Fragmented QRS Complex in Iranian Patients with Systemic Sclerosis. J Tehran Heart Cent. 14(1),6 (2019).
- Ambesh SP, Singh N, Rao PB et al. A combination of the modified Mallampati score, thyromental distance, anatomical abnormality, and cervical mobility (M-TAC) predicts difficult laryngoscopy better than Mallampati classification. Acta Anaesthesiol Taiwan. 51(2),58-62 (2013).
- Myneni N, O'Leary AM, Sandison M et al. Evaluation of the upper lip bite test in predicting difficult laryngoscopy. J Clin Anesth. 22(3),174-178 (2010).
- Sharma S, Patel R, Hashmi MF et al. 3-3-2 Rule. (2018).
- Tripathi M, Pandey M. Short thyromental distance: a predictor of difficult intubation or an indicator for small blade selection? J American Society Anesthesiol. 104(6),1131-1136 (2006).
- Torok KS, Baker NA, Lucas M et al. Reliability and validity of the delta finger-to-palm (FTP), a new measure of finger range of motion in systemic sclerosis. Clin Exp Rheumatol. 28(2 Suppl 58),S28 (2010).
- Lopez-Olivo MA, Andrabi TR, Palla SL et al. Cervical spine radiographs in patients with rheumatoid arthritis undergoing anesthesia. J Clin Rheumatol. 18(2),61-66 (2012).
- Akkurt BCO, Guler H, Inanoglu K et al. Disease activity in rheumatoid arthritis as a predictor of difficult intubation? Eu J Anaesthesiol. 25(10),800-804 (2008).
- Prakash S, Kumar A, Bhandari S et al. Difficult laryngoscopy and intubation in the Indian population: An assessment of anatomical and clinical risk factors. Indian J Anaesth. 57(6),569 (2013).
- El-Radaideh KK, Dheeb E, Shbool H et al. Evaluation of different airway tests to determine difficult intubation in apparently normal adult patients undergoing surgical procedures. Patient Saf Surg. 14(1),1-8 (2020).
- Moaveni D, Cohn J, Brodt J et al. Scleroderma and pulmonary hypertension complicating two pregnancies: use of neuraxial anesthesia, general anesthesia, epoprostenol and a multidisciplinary approach for cesarean delivery. Int J Obstet Anesth. 24(4),375-382 (2015).
- Czirjak L, Foeldvari I, Müller-Ladner U. Skin involvement in systemic sclerosis. Rheumatology. 47(suppl_5),v44-v45 (2008).
- Kumánovics G, Péntek M, Bae S et al. Assessment of skin involvement in systemic sclerosis. Rheumatology. 56(suppl_5),v53-v66 (2017).
- Wannarong T, Muangchan C. High burden of skin sclerosis is associated with severe organ involvement in patients with systemic sclerosis and systemic sclerosis overlap syndrome. Rheumatology Int 38(12),2279-2288 (2018).
- Ledoult E, Launay D, Béhal H et al. Early trajectories of skin thickening are associated with severity and mortality in systemic sclerosis. Arthritis Res Ther. 22(1),1-12 (2020).
- Shand L, Lunt M, Nihtyanova S et al. Relationship between change in skin score and disease outcome in diffuse cutaneous systemic sclerosis: application of a latent linear trajectory model. Arthritis Rheum. 56(7),2422-2431 (2007).
- Merkel PA, Silliman NP, Clements PJ et al. Patterns and predictors of change in outcome measures in clinical trials in scleroderma: an individual patient meta-analysis of 629 subjects with diffuse cutaneous systemic sclerosis. Arthritis Rheum. 64(10),3420-3429 (2012).
- Nevskaya T, Zheng B, Baxter CA et al. Skin improvement is a surrogate for favourable changes in other organ systems in early diffuse cutaneous systemic sclerosis. Rheumatol. 59(7),1715-1724 (2020).
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref