Research Article - Clinical Practice (2021) Volume 18, Issue 8
The adherence to guideline-directed therapy post-surgical revascularisation in coronary artery disease and its effect on postoperative outcomes
- Corresponding Author:
- Eric Yu Wei Lo
Department of Cardiothoracic Surgery
Liverpool Hospital, Australia
E-mail: ericyuweilo@gmail.com
Abstract
Background: The American Heart Association (AHA) in 2015 released a scientific statement with regards to secondary prevention after Coronary Artery Bypass Graft surgery (CABG) [1] where advice around antiplatelet, antihypertensives, beta-blockers, and anti-lipids post CABG for secondary prevention is prescribed. This paper reviewed adherence at a single center after discharge with AHA guidelines for secondary prevention after CABG [1] and the effect this had on outcomes.
Methods: All CABG patients at Liverpool Hospital, NSW, Australia from 2016-2018 were retrospectively analyzed using the cardiac surgery database. Univariate and multivariate analysis to thirty-day mortality was performed (STATA v16.1). Secondary outcomes of morbidity were reviewed.
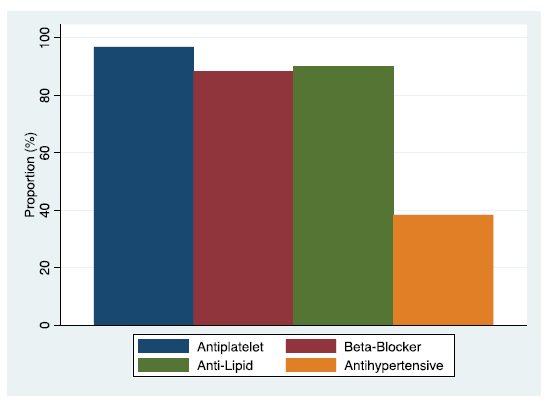
Results: Adherence to AHA Guidelines in nine hundred and sixteen patients who underwent CABG was analyzed. Antiplatelet therapy (96.9%), beta-blocker (88.3%), anti-lipid (90.1%), antihypertensive (38.4%), and total adherence (33.62%). Adherence influenced outcomes of thirty-day mortality and post-operative Myocardial Infarction (MI) but not in post-operative stroke or revascularization rates. Multivariate analysis found that antiplatelet (OR 0.06, 95% CI 0.02-0.25, p<0.001) and anti-lipid therapy (OR 0.26, 95% CI 0.08-0.89, p=0.032) were protective factors against thirty-day mortality, with Peripheral Vascular Disease (PVD) (OR 7.98, 95% CI 2.00-31.80, p=0.003) predicting mortality in this cohort.
Conclusion: Adherence rates to AHA guidelines for secondary prevention post-surgical revascularisation were found to be comparable to that reported in the literature at discharge from the hospital. The independent importance of adherence to antiplatelet therapy and anti-lipid therapy was shown in this cohort in addition to the independent negative effects of PVD on thirty-day mortality. This highlights the importance of adherence to guideline-directed therapies.
Keywords
adherence, secondary prevention, cardiology, cardiac surgery
Introduction
For the conscientious healthcare professional, Guideline Directed Medical Therapy (GDMT) is an important tool to inform clinical practice. In Coronary Artery Bypass Graft Surgery (CABG), adherence to GDMT is low postoperatively [2] and less than that in physician-treated patient populations post Percutaneous Coronary Intervention (PCI) [3,4]. Surgical revascularisation aims to improve prognosis concerning coronary events, the adherence to secondary prevention measures should form an important aspect of clinical care of the post CABG patient. With the promotion of evidence-based medicine as a principle to treat where there exists evidence of benefit [5], guidelines allow expert bodies to help clinicians treat patients with evidence-based standards of care.
The American Heart Association (AHA) in 2015 released a scientific statement with regards to secondary prevention after CABG [1]. In this statement, advice around antiplatelet, antihypertensives, beta-blockers, and anti-lipid agents is detailed specifically about the post CABG patients for secondary prevention.
The AHA examined the evidence wherever possible and based on previous guidelines, contemporaneous trials and large observational studies gave recommendations for medical management post CABG in the domains of antiplatelets, beta-blockers, anti-lipid drugs, and antihypertensives [1].
With antiplatelets, the AHA guidelines recommend that aspirin should be given postoperatively within six hours and continued indefinitely (Class 1 recommendation, Level of Evidence A) [1]. After off-pump CABG it is recommended by the AHA that Dual Antiplatelet Therapy (DAPT) should be continued for a year post-operatively with the use of clopidogrel (75 mg) in addition to aspirin to reduce graft occlusion (Class 1 recommendation, Level of Evidence A) [1].
Beta-blockers are recommended by the AHA Guidelines for the prevention of post-operative Atrial Fibrillation (AF) and in patients who have a previous Myocardial Infarction (MI) (Class 1 recommendation, Level of Evidence A) [1]. The type of beta-blocker is prescribed by the AHA in the situation when there is left ventricular dysfunction; where the guidelines recommend a long-acting beta-blocker (bisoprolol, metoprolol XL or carvedilol) (Class 1 recommendation, Level of Evidence B) [1].
Anti-lipid therapy with statin therapy is recommended for all CABG patients in the AHA guidelines for secondary prevention post CABG (Class 1 recommendation, Level of Evidence A) [1]. Satin dosage is discussed by age, with highintensity statin therapy for CABG patients <75 and moderate intensity for those >75 (Class 1 Recommendation, Level of Evidence A) [1].
Hypertension management recommendations in the AHA guidelines begin with beta-blocker use post-operatively (Class 1 recommendation, Level of Evidence A) [1]. Angiotensinconverting enzyme inhibitor (ACE-I) treatment is recommended for patients with recent MI, left ventricular dysfunction, diabetes mellitus, and chronic kidney disease (Class 1 recommendation, Level of Evidence A) [1]. The AHA goes further to recommend ACE-I or Angiotensin II Receptor Blocker (ARB) therapy if ACE-I is not tolerated for whatever reason, should be instituted for all CABG patients who have an ejection fraction (EF) <40% or previous MI (Class 1 recommendation, Level of Evidence B) [1].
Current practice at Liverpool Hospital, NSW, Australia regarding secondary prevention post-CABG is anecdotally in keeping with established guidelines, however, this has never been scrutinized. Implementation of secondary prevention for post CABG patients is surgeon dependant. For instance, DAPT post CABG versus aspirin alone in the elective, post-acute coronary syndrome, and post-off-pump surgery varies amongst surgeons. This individualized practice inspired scrutiny to ensure best practices were being implemented by international guidelines. Moreover, while it is assumed that adherence to GDMT improves outcomes for patients; examining the effect of adherence on outcomes in a real-world population can reinforce the benefits of implementation of GDMT in patients of all clinicians.
■ Adherence
Guidelines do not necessarily translate to therapy that is given to patients. In 2014 researchers examined the adherence rates of secondary prevention in a randomly selected cohort of CABG patients at admission and one year postoperatively [2]. Composite Adherence to all four agents was under 50% at both time points examined, however, this was largely due to the non-Adherence of ACE-i/ARB [2]. In 2019, researchers in Taiwan examined guideline adherence with AHA guidelines with specific attention to antiplatelet, beta-blockers, statins, and ACE-I/ARB and found in the Taiwanese CABG population adherence was around 40% for each of the individual classes of medications [4]. Further, a Finnish research group reported a lower achievement of secondary prevention in a rural population that had lower socioeconomic status and therefore lower access to standard care compared to a regional cohort [6].
A large multicentre observational study to look at the effect of cardiac rehab on compliance with medications [7]. They found that the cardiac rehabilitation program improved rates of adherence at one year [7]. Regarding the adherence at discharge, the authors found around 90% GDMT adherence [7].
■ Outcomes
The adherence to GDMT should yield better outcomes for patients as the guidelines are informed by available evidence. Taiwanese researchers found that the rate of death and or post-operative MI was higher in the patients who were not taking these drugs at discharge for the various GDMT [4]. All medications had mortality and morbidity benefit: with antiplatelet 20.4% vs. 15.5%, ACE-i/ARB 18.1% vs. 14.6%, statins had 19 versus 12.0%, beta-blocker 18.2% vs.13.6% mortality and or MI; although no statistical analysis was described [4].
This article examines practices with a retrospective observational cohort study; reviewing over three years of CABG patients at a single center to ascertain adherence at discharge with AHA guidelines for secondary prevention after CABG [1] and the effect adherence has on postoperative outcomes.
Materials and Methods
In this retrospective observational study, participants included all patients who underwent CABG over three years (2017-2019) at Liverpool Hospital NSW, Australia. This methodology was chosen to examine the current practice at the institution about adherence to Class 1 recommendations from AHA Guidelines [1] and the resultant effect on outcomes of mortality and morbidity; specifically, thirty-day mortality and secondary outcomes of postoperative MI, stroke, and redo revascularisation. The adherent and non-adherent groups were compared with the hypothesis being that guideline-directed secondary prevention therapy improves outcomes post CABG.
Statistical analyses
Group characteristics were compared using t-test, chi-squared, and Mann-Whitney U tests for parametric, categorical, and non-parametric variables respectively. The primary outcomes of interest were adherence to secondary prevention guidelines at discharge and their effect on mortality and morbidity. Potential confounding factors beyond the exposure of adherence to AHA secondary prevention guidelines were accounted for through univariate and multivariate analysis of the socio-demographic, risk factors, clinical differences, and adherence with regards to morbidity and mortality. This was performed via a stepwise univariate and multivariate logistic regression including the adherence variables and significant variables with a significance level set at p ≤ 0.05. For univariate and multivariate analysis of these outcomes, penalized maximum likelihood logistic regression (Firth method) was used to overcome the issues of rare events and separation [8].
Results
■ Adherence to AHA Guidelines
From the single-center experience at Liverpool Hospital, NSW, Australia over the three years from 2016-2018, data from 916 patients who underwent CABG. Their adherence to AHA Guidelines [1], with regards to antiplatelet, beta-blockers, anti-lipid, and antihypertensive medications at discharge was reviewed. Adherence to antiplatelet therapy (96.9%), beta-blocker (88.3%), anti-lipid (90.1%), and antihypertensive (38.4%) is detailed in (FIGURE 1 and TABLE 1) .Total adherence with the four aspects as per AHA Guidelines [1] was 33.62% (TABLE 1).
| Adherence (%) | |
|---|---|
| Antiplatelet | 96.94 |
| Beta-Blocker | 88.32 |
| Anti-Lipid | 90.07 |
| Anti HTN | 38.43 |
| Total | 33.63 |
TABLE 1. Adherence to AHA Guidelines.
Demographic data for those adherent to the four aspects of the AHA Guidelines [1] versus not is outlined in Table 2 for each aspect and composite adherence. With regards to antiplatelet adherence (TABLE 2), significant differences between the groups was found in female gender (39.3% vs. 19.6%, p=0.01); weight (70.6 kg versus 83.6 kg, p<0.001); smoking history (28.6% vs. 55.7%, p<0.01); hypercholesterolaemia (67.9% vs. 84.5%, p=0.02); respiratory disease (28.6% vs. 8.6%, p<0.001); and preoperative shock (3.6% vs. 0.5%; p=0.03) (TABLE 2).
| Antiplatelets | |||
| Non- Adherence | Adherence | p value | |
| Age (Mean) | 67.11 | 66.12 | 0.6 |
| Female (%) | 39.29 | 19.59 | 0.011 |
| Weight (kg) | 70.57 | 83.58 | 0.0005 |
| Smoking (%) | 28.57 | 55.74 | 0.0044 |
| CVD (%) | 10.71 | 7.55 | 0.53 |
| PVD (%) | 3.57 | 7.66 | 0.42 |
| AF (%) | 10.71 | 5.52 | 0.24 |
| DM (%) | 42.86 | 48.42 | 0.56 |
| HCHOL (%) | 67.86 | 84.46 | 0.018 |
| Elective (%) | 28.57 | 27.7 | 0.92 |
| Resp Disease (%) | 28.57 | 8.56 | 0.0003 |
| Previous MI (%) | 50 | 53.04 | 0.75 |
| SHOCK (%) | 3.57 | 0.45 | 0.027 |
| Beta-Blockers | |||
| Non- Adherence | Adherence | p value | |
| Age (Mean) | 65.92 | 66.18 | 0.8 |
| Female (%) | 20.56 | 20.15 | 0.92 |
| Weight (kg) | 86.2 | 82.79 | 0.089 |
| Smoking (%) | 57.94 | 54.51 | 0.5 |
| CVD (%) | 11.21 | 7.17 | 0.14 |
| PVD (%) | 8.41 | 7.42 | 0.71 |
| AF (%) | 15.89 | 4.33 | <0.000001 |
| DM (%) | 52.34 | 47.71 | 0.37 |
| HCHOL (%) | 83.18 | 84.05 | 0.82 |
| Elective (%) | 17.76 | 29.05 | 0.014 |
| Resp Disease (%) | 7.48 | 9.39 | 0.52 |
| Previous MI (%) | 47.66 | 53.65 | 0.24 |
| SHOCK (%) | 0.93 | 0.49 | 0.56 |
| Anti-lipids | |||
| Non- Adherence | Adherence | p value | |
| Age (Mean) | 66.15 | 66.14 | 0.99 |
| Female (%) | 23.08 | 19.88 | 0.47 |
| Weight (kg) | 78.34 | 83.72 | 0.012 |
| Smoking (%) | 53.85 | 55.03 | 0.83 |
| CVD (%) | 8.79 | 7.52 | 0.66 |
| PVD (%) | 5.49 | 7.76 | 0.44 |
| AF (%) | 12.09 | 4.97 | 0.0054 |
| DM (%) | 57.14 | 47.27 | 0.074 |
| HCHOL (%) | 70.33 | 85.45 | 0.0002 |
| Elective (%) | 12.09 | 29.45 | 0.0005 |
| Resp Disease (%) | 12.09 | 8.85 | 0.31 |
| Previous MI (%) | 48.35 | 53.45 | 0.35 |
| SHOCK (%) | 1.1 | 0.48 | 0.45 |
| Antihypertensives | |||
| Non- Adherence | Adherence | p value | |
| Age (Mean) | 65.4 | 67.34 | 0.004 |
| Female (%) | 19.15 | 21.88 | 0.32 |
| Weight (kg) | 83.74 | 82.3 | 0.27 |
| Smoking (%) | 55.67 | 53.69 | 0.56 |
| CVD (%) | 8.51 | 6.25 | 0.21 |
| PVD (%) | 8.87 | 5.4 | 0.053 |
| AF (%) | 6.38 | 4.55 | 0.24 |
| DM (%) | 49.47 | 46.31 | 0.35 |
| HCHOL (%) | 85.11 | 82.1 | 0.23 |
| Elective (%) | 24.47 | 32.95 | 0.0053 |
| Resp Disease (%) | 8.87 | 9.66 | 0.69 |
| Previous MI (%) | 85.99 | 0 | <0.000001 |
| SHOCK (%) | 0.89 | 0 | 0.077 |
| Total Adherence | |||
| Non- Adherence | Adherence | p value | |
| Age (Mean) | 65.69 | 67.04 | 0.053 |
| Female (%) | 20.07 | 20.45 | 0.89 |
| Weight (kg) | 83.16 | 83.23 | 0.96 |
| Smoking (%) | 55.26 | 54.22 | 0.76 |
| CVD (%) | 8.39 | 6.17 | 0.23 |
| PVD (%) | 8.39 | 5.84 | 0.17 |
| AF (%) | 6.58 | 3.9 | 0.097 |
| DM (%) | 49.84 | 45.13 | 0.18 |
| HCHOL (%) | 84.05 | 83.77 | 0.91 |
| Elective (%) | 23.52 | 36.04 | <0.0001 |
| Resp Disease (%) | 9.05 | 9.42 | 0.85 |
| Previous MI (%) | 79.77 | 0 | <0.000001 |
| SHOCK (%) | 0.83 | 0 | 0.11 |
TABLE 2. Patient Factors comparison by Adherence.
With beta-blocker adherence, significant differences between the groups were found in existing AF (15.9% vs 4.3%; p<0.0001); and elective cases (17.8% vs 29.05%, p=0.01) (TABLE 2).
With anti-lipids adherence, significant differences between the groups were found in existing weight (78.3% vs. 83.7%, p=0.01); AF (12.1% vs 5.0%; p=0.005); hypercholesterolaemia (70.3% vs. 85.5%, p<0.001); and elective cases (12.1% vs. 29.5%, p<0.001) (TABLE 2) .
With antihypertensives adherence, significant differences between the groups were found in age (65.4 vs. 67.3; p<0.01); elective cases (24.5% vs. 33.0 %, p=0.005); and previous MI (86% vs. 0%, p<0.0001) (TABLE 2) .
With total adherence, significant differences between the groups were found in elective cases (23.5% vs. 36.0%, p<0.0001); and previous MI (79.8% vs. 0.0%, p<0.0001) (TABLE 2) .
■ Outcomes with regards to adherence to AHA Guidelines
Thirty-day mortality post CABG was compared in rates of adherence to the aspects of the AHA guidelines [1]. Survivors were more adherent with antiplatelets (97.5% vs. 64.3%, p<0.001); beta-blockers (88.8% vs. 57.1%, p=0.0003); anti-lipids (90.5% vs. 64.3%, p=0.001); antihypertensives (39.0% vs. 0.0%; p=0.003) and in total (34.1% vs. 0.0%, p=0.007) (TABLE 3).
| Survival | Death | p value | |
|---|---|---|---|
| Antiplatelet (%) | 97.45 | 64.29 | <0.000001 |
| Beta-Blocker (%) | 88.8 | 57.14 | 0.0003 |
| Anti-Lipid (%) | 90.47 | 64.23 | 0.0012 |
| Anti HTN (%) | 39.02 | 0 | 0.0029 |
| Total (%) | 34.15 | 0 | 0.0073 |
TABLE 3. Outcome (Mortality) compared by Adherence.
The secondary outcome of post-operative MI was also examined with regards to rates of adherence. Significant differences in rates of adherence in freedom from post-operative MI as compared to those who had the complication was seen in antiplatelet adherence (97.0% vs. 80.0%, p=0.03); beta-blockers (88.5% vs. 60.0%, p=0.05); and anti-lipids (90.2% vs. 60.0%, p=0.02 (TABLE 4). The differences seen in antihypertensives (38.5% vs. 20.0%; p=0.4); and in total (33.7% vs. 20.0%, p=0.5) were not statistically significant (TABLE 4).
| No MI | MI | p value | |
|---|---|---|---|
| Antiplatelet (%) | 97.04 | 80 | 0.027 |
| Beta-Blocker (%) | 88.47 | 60 | 0.048 |
| Anti-Lipid (%) | 90.23 | 60 | 0.024 |
| Anti HTN (%) | 38.53 | 20 | 0.4 |
| Total (%) | 33.7 | 20 | 0.52 |
TABLE 4. Outcome (Post-Operative MI) compared by Adherence.
The secondary outcome of stroke was examined with rates of adherence. No significant differences in rates of adherence in freedom from post-operative stroke as compared to those who had the complication with differences in antiplatelet adherence (97.0% vs. 95.5%, p=0.7); beta-blockers (88.4% vs. 86.4%; p=0.8); anti-lipids (90.2% vs. 81.8%, p=0.2); antihypertensives (38.8% vs. 22.8%, p=0.1); and in total (33.9% vs. 22.7%, p=0.3) were all not statistically significant (TABLE 5).
| No CVA | CVA | p value | |
|---|---|---|---|
| Antiplatelet (%) | 96.98 | 95.45 | 0.68 |
| Beta-Blocker (%) | 88.37 | 86.36 | 0.77 |
| Anti-Lipid (%) | 90.276 | 81.82 | 0.19 |
| Anti HTN (%) | 38.81 | 22.73 | 0.13 |
| Total (%) | 33.89 | 22.73 | 0.27 |
TABLE 5. Outcome (Stroke) compared by Adherence.
The secondary outcome of revascularisation post CABG was examined with rates of adherence. And again. no significant differences in rates of adherence in those who did not require revascularisation and those who did. In antiplatelet adherence (97.0% vs. 100.0%, p=0.6); beta-blockers (88.2% vs. 100.0%; p=0.3); anti-lipids (90.2% vs. 77.7%, p=0.2); antihypertensives (38.4% vs. 44.4%, p=0.7); and in total (33.6% vs. 33.3%, p=1.0) were all not statistically significant (TABLE 6).
| No Revascularisation | Revascularisation | p value | |
|---|---|---|---|
| Antiplatelet (%) | 96.91 | 100 | 0.59 |
| Beta-Blocker (%) | 88.2 | 100 | 0.27 |
| Anti-Lipid (%) | 90.19 | 77.78 | 0.22 |
| Anti HTN (%) | 38.37 | 44.44 | 0.71 |
| Total (%) | 33.63 | 33.33 | 0.99 |
TABLE 6. Outcome (Revascularisation) compared by Adherence.
■ Univariate Analysis
Patient factors and adherence to AHA Guidelines [1] were analysed via univariate analysis of factors in relation to mortality by logistic regression (TABLE 7). Cerebrovascular disease (OR 5.39, 95% CI 1.78-16.73, p=0.004), peripheral vascular disease (OR 7.53, 95% CI 2.56-22.17, p=0.0003), preoperative AF (OR 5.25, 95% CI 1.53-17.96, p=0.008), and adherence to the four aspects of the AHA Guidelines [1] individually and composite adherence (Antiplatelet (OR 0.05, 95% CI 0.02-0.14, p<0.001), beta-blocker (OR 0.17, 95% CI 0.06-0.47, p<0.001), anti-Lipid (OR 0.18, 95% CI 0.06-0.54, p=0.002), antihypertensives (OR 0.054, 95% CI 0.003-0.91, p=0.04), and total adherence (OR 0.07, 95% CI 0.004-1.12, p=0.56) all were found to statistically significant factors of mortality.
| Odds Ratio | 95% Confidence interval | p value | |
|---|---|---|---|
| Patient Factors | |||
| Age | 1.04 | 0.99-1.10 | 0.16 |
| Female | 2.32 | 0.80-6.71 | 0.12 |
| Weight | 1 | 0.97-1.03 | 0.95 |
| Smoking Hx | 0.62 | 0.22-1.75 | 0.37 |
| Cerebrovascular Disease | 5.39 | 1.74-16.73 | 0.004* |
| Peripheral Vascular Disease | 7.53 | 2.56-22.17 | 0.0003* |
| Preoperative AF | 5.25 | 1.53-17.96 | 0.008* |
| Diabetes Mellitus | 1.41 | 0.50-3.95 | 0.51 |
| Hypercholesterolaemia | 0.63 | 0.19-2.10 | 0.45 |
| Elective | 0.79 | 0.24-2.63 | 0.7 |
| Respiratory Disease | 1.99 | 0.50-7.88 | 0.33 |
| Adherence | |||
| Antiplatelet | 0.05 | 0.02-0.14 | <0.001* |
| Beta-blocker | 0.17 | 0.06-0.47 | <0.001* |
| Anti-Lipid | 0.18 | 0.06-0.54 | 0.002* |
| Antihypertensive | 0.05 | 0.003-0.91 | 0.04* |
| Total Compliance | 0.07 | 0.004-1.12 | 0.56* |
| *Significant Value | |||
TABLE 7. Univariate logistic regression examining the effect of patient factors and management factors on mortality.
■ Multivariate Analysis
Taking into consideration the statistically significant factors (at a significance level of p<=0.05) and inclusive of adherence rates, multivariate logistic regression was performed (Table 8). The independent factors of mortality that were found via multivariate analysis included peripheral vascular disease (OR 7.98, 95% CI 2.00-31.80, p=0.003), antiplatelet (OR 0.06, 95% CI 0.02-0.25, p<0.001), anti-lipid (OR 0.26, 95% CI 0.08-0.89, p=0.032).
| Odds Ratio | 95% Confidence interval | p value | |
|---|---|---|---|
| Cerebrovascular Disease | 2.03 | 0.46-9.00 | 0.35 |
| Peripheral Vascular Disease | 7.98 | 2.00-31.80 | 0.003* |
| Preoperative AF | 2.79 | 0.62-12.55 | 0.18 |
| Antiplatelet | 0.06 | 0.02-0.25 | <0.001* |
| Beta-blocker | 0.58 | 0.17-1.99 | 0.38 |
| Anti-Lipid | 0.26 | 0.07-0.89 | 0.032* |
| Antihypertensive | 0.22 | 0.01-3.98 | 0.31 |
| Total Adherence | 0.71 | 0.01-39.39 | 0.87 |
| *Significant Value | |||
TABLE 8. Multivariate logistic regression examining the effect of patient factors and management factors on mortality.
Discussion
In this retrospective observational cohort study, the aim was to ascertain the adherence rates to AHA Guidelines for secondary prevention post-surgical revascularisation [1] and its relationship to outcomes of mortality and morbidity. Overall compliance to the AHA guidelines for secondary prevention post CABG was found to be low (complete adherence at 33.6%). This was comparable to findings from 2014 by Barry et al., which reported the utilization rate for patients receiving all four classes of secondary prevention cardiovascular medication was 35% at discharge [2]. Deficiencies were found in anti-hypertensive use, which individually demonstrated the lowest adherence (38.4%). Similarly, Barry et al in 2014 found that adherence rates to ACE-I/ARBs were the lowest of the four aspects studied (42%, the other three aspects ranging from 94-96% adherence at discharge) [2].
Possibly the timepoint of adherence examined explains this. Barry et al., (2014), found an increase in adherence at a later follow update (42% at discharge to 65% at one-year follow-up) [2]. Possibly the nature of post-operative patients’ blood pressures at discharge compared to later in their convalescence may contribute to the low adherence with antihypertensives. These patients tend to have lower blood pressures close to the operation precluding them from antihypertensives as compared to when they recover and can tolerate therapy. This is an observed phenomenon in clinical practice.
With thirty-day mortality, composite adherence to the AHA guidelines were found to be a statistically significant factor. Individually, each aspect showed higher rates of adherence in the survival group. This intuitively makes sense as the principles of evidence-based medicine are that adherence to GDMT, which has evidence of benefit as the foundation for the recommendations, should have better outcomes for the individual patient.
The variation in the cohorts at baseline with regards to composite adherence included elective cases which were in higher proportion in adherent patients (TABLE 2) (36.04% vs. 23.52%, p<0.0001) and previous MI which were seen in lower numbers of adherent patients (TABLE 2) (0.00% vs. 79.77%, p<0.000001). Elective cases by nature would be expected to be a more controlled endeavor with the outcomes being less morbid than the alternative. As a result, the cohort that is both adherent and more elective may be showing lower mortality because of the elective status rather than the adherence. Similarly, patients who have had a previous MI have already had an insult to their myocardium and as a result, may lead to a worse outcome. This worse foundation may be the reason the higher incidence of thirty-day mortally is seen in this cohort despite the adherence.
To account for the variation in the cohorts a stepwise univariate to multivariate logistic regression analysis was undertaken. Unsurprisingly the four aspects of adherence were found to be statically significant protective factors against thirty-day mortality. However, cerebrovascular disease, peripheral vascular disease, and preoperative AF were as well found to be statistically significant factors in thirty-day mortality via univariate analysis (TABLE 7). Taking into consideration these factors including the adherence factors, multivariate logistic regression was performed. Considering other factors, adherence to the four aspects individually and as composite adherence were not all found to be factors contributing to thirty-day mortality. Antiplatelet and anti-lipid adherence were found to be statistically significant protective factors for mortality. Peripheral vascular disease as well was found to be a statistically significant factor of thirty-day mortality. These findings emphasize the importance of antithrombotic effects and anti-lipid effects on this cardiovascular morbid group of patients. Similarly, the full-body effect seen in patients with known peripheral vascular disease heralds the outcome of all-cause thirty-day mortality in this group of people despite adherence to GDMT.
In the secondary outcomes analyzed, only post-operative MI was found to have a statistically significant difference in adherence between those who experienced the complication and those who did not (Table 4). The implications of these findings for clinical practice emphasize the importance of these secondary prevention measures concerning outcomes. Antiplatelet and anti-lipid aspects of the AHA GDMT for secondary prevention post CABG were found to be statistically significant protective factors in thirty-day mortality. The adherence found in antiplatelet and anti-lipid therapy was >90% in this cohort but encourages the persistence with this clinical practice of prescribing these medications to prevent thirty-day mortality. This study found that adherence with antiplatelet recommendations at discharge conferred a reduction in odds of thirty-day mortality of 94% and with adherence of antiplatelet therapy and with anti-lipid recommendations a reduction in odds of thirty-day mortality of 74% via multivariate analysis (TABLE 8). With anti-lipid management, these findings are consistent with what is seen in the literature, with researchers specifically examining statin therapy found in its secondary outcomes that anti-lipid therapy conferred a reduction in major adverse cardiovascular events [9]. Further, in another study examining multiple secondary prevention strategies, anti-lipid therapies (statins) were found to be protective [4]. Regarding anti-platelet therapy, the majority of findings in the literature endorse the use of antiplatelet therapy long-term post CABG, with some contention with regards to dual antiplatelet therapy and its duration postoperatively [10]. These AHA guidelines for secondary prevention post CABG had statistically significant protective properties in two of the four recommendations regarding thirty-day mortality. These all serve to encourage the consistent prescription of secondary prevention measures in a real-world cohort.
Limitations in the study largely surround the timing of follow-up. Class 1 recommendations by the AHA guidelines for secondary prevention post-surgical revascularisation state that antiplatelet therapy should be instituted by six hours post-operation [1]. This study, like many others in the literature report on GDMT using the metric of prescriptions at discharge or in the community. This fails to capture if the antiplatelet therapy is being instituted at a time that is in line with Class 1 recommendations. As this time point has not been reviewed in the compliance literature, it is difficult to comment on if this would be an important factor in short-term to long-term outcomes of morbidity and mortality.
Furthermore, longer-term follow-up of these patients would give more information as to the long-term effect of adherence to secondary prevention guidelines. The effects of long-term use of GDMT were questioned in previous studies where researchers found that the treatment effect was greatest in the first year of therapy rather than the subsequent years concerning beta-blockers [11]. Further follow-up may give a timeframe to how therapy should be instituted long-term in other agents as well.
To improve adherence to GDMT, firstly dissemination of current practices and their effect on patient outcomes should be realized following the recommended audit cycle [12]. This would promote the importance of GDMT in this cohort of post CABG patients to reduce adverse outcomes; particularly because of the positive nature of the findings of the study.
Conclusion
Guideline-directed therapy for secondary prevention is an important way to standardize care for patients who undergo surgical revascularisation in an evidence-based fashion. adherence rates to AHA guidelines for secondary prevention post-surgical revascularisation were found to be comparable to that reported in the literature at discharge from the hospital. The effect on outcomes in this study was found concerning thirty-day mortality and postoperative MI, but not in other complications of post-operative stroke and revascularization rates. Through a stepwise univariate and multivariate analysis, the independent importance of adherence with antiplatelet therapy and antilipid therapy was shown in this cohort in addition to the independent negative effects of peripheral vascular disease on thirty-day mortality.
These findings will inform practice and strategies for quality improvements in this postsurgical revascularisation setting. Future studies into earlier and later follow-up timepoints may further elucidate the importance of early adherence in the post-operative patient and adherence effect beyond the short and intermediate-term outcomes examined in this study.
References
- Kulik A, Ruel M, Jneid H, et al. Secondary prevention after coronary artery bypass graft surgery: a scientific statement from the American Heart Association. Circulation. 131, 927-964 (2015).
- Barry AR, Koshman SL, Norris CM, et al. Evaluation of preventive cardiovascular pharmacotherapy after coronary artery bypass graft surgery. Pharmacotherapy. 34, 464-472 (2014).
- Riley RF, Don CW, Aldea GS, et al. Recent trends in adherence to secondary prevention guidelines for patients undergoing coronary revascularization in Washington state: an analysis of the Clinical Outcomes Assessment Program (COAP) Registry. J Am Heart Assoc. 1, e002733 (2012).
- Feng WH, Chu CY, Hsu PC, et al. The effects of secondary prevention after coronary revascularization in Taiwan. PloS one. 14, e0215811 (2019).
- Belsey J. What is evidence-based medicine? (2009). [Available at: http://www.bandolier.org.uk/painres/download/whatis/ebm.pdf].
- Repo T, Tykkylainen M, Mustonen J, et al. Outcomes of secondary prevention among coronary heart disease patients in a high-risk region in Finland. Int J Environ Res Public Health. 15, 724 (2018).
- Gao XQ, Li Y, Jiang ZL. Comparison of secondary prevention status between percutaneous coronary intervention and coronary artery bypass patients. Arq Bras Cardiol. 109, 466-474 (2017).
- Wang X. Firth logistic regression for rare variant association tests. Front Genet. 5, 187 (2014).
- Poorhosseini H, Tavolinejad H, Aminorroaya A, et al. The association of statins for secondary prevention with progression to diabetes in patients with the prediabetic state after coronary artery bypass graft surgery: A retrospective cohort study. J Diabetes Complications. 34, 107713 (2020).
- Liu M, Zhuang X, Chen X, et al. Antiplatelet strategy in primary and secondary prevention of cardiovascular disease in patients with type 2 diabetes mellitus: A perspective from the guideline appraisal. J Diabetes Investig. 12, 99-108 (2020).
- Park J, Lee SH, Jeong DS, et al. Association between β-Blocker and outcome of coronary artery bypass graft: before and after 1 year. Ann Thorac Surg. 111, 69-75 (2020).
- Benjamin A. Audit: how to do it in practice. BMJ. 336, 1241-1245 (2008).