Case Report - Clinical Practice (2020) Volume 17, Issue 1
Successful left gastric artery embolization followed by coronary stenting in a patient with ACS complicated by severe upper gastrointestinal bleeding
- Corresponding Author:
- Marat A. Aripov
Department of Interventional Cardiology
National Research Cardiac
Surgery Centre, Kazakhstan
E-mail: Dr.aripov@gmail.com
Abstract
The presence of severe upper gastrointestinal bleeding significantly limits the use of antiplatelet and anticoagulation therapy in patients with Acute Coronary Syndrome (ACS), because of the risks inherent in performing PCI with anticoagulant and antiplatelet agents. A 72-year-old man was diagnosed with the non-ST-elevation acute coronary syndrome (NSTE-ACS) by ECG and clinical signs. We performed urgent coronagraphy, which revealed multivessel lesions of coronary arteries with critical stenosis of the coronary artery. Cardiac surgery with shunting was planned for the following day, but we subsequently observed melena and the patient began vomiting with blood. Gastroscopy was performed and revealed the presence of stomach cancer on the sub cardinal region reaching the body of the stomach. The dilemma of the current case was the combined risk of further cardiovascular morbidity and the risk of bleeding on dual antiplatelet therapy. Embolization of the left gastric artery was performed with the EmbGold Biosphere 500- 700 µm; concomitant use of clopidogrel and aspirin let us perform stenting using drug-eluting Resolute Integrity and Resolute Onyx stents (Medtronic). This case report suggests that gastric artery embolization is possible in patients with ACS, complicated by acute upper gastrointestinal bleeding requiring stenting and dual antiplatelet therapy.
Keywords
ACS, gastrointestinal bleeding (GIB) stenting, dual antiplatelet therapy, embolization
Background
The presence of severe upper gastrointestinal bleeding significantly limits the use of antiplatelet and anticoagulation therapy in patients with Acute Coronary Syndrome (ACS). This presents significant challenges because of the risks inherent in performing PCI with anticoagulant and antiplatelet agents. The risks of not intervening in this context must also be considered.
Case Report
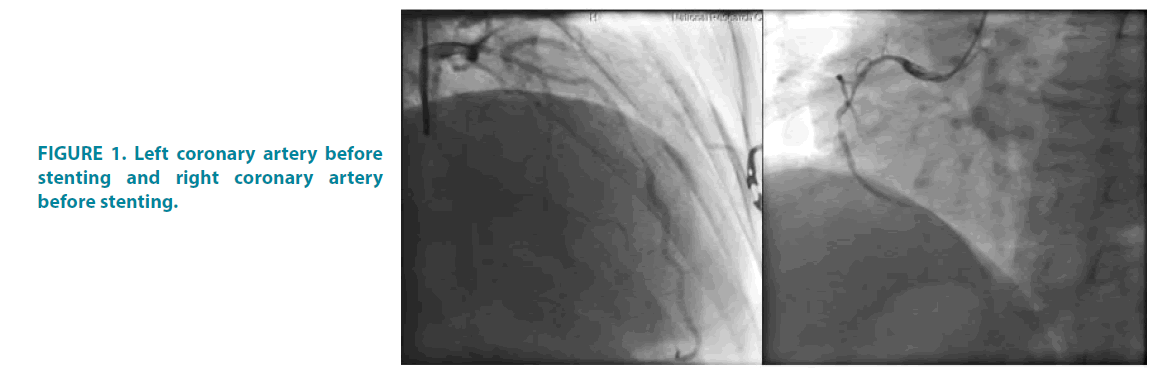
A 72-year-old man was diagnosed at his home with non-ST-elevation acute coronary syndrome (NSTE-ACS) by ECG and clinical signs. The ambulance physicians treated him en route to the hospital with heparin, ticagrelor and aspirin according to our standard protocol. This patient, who was previously unfamiliar to our center, was assessed in the emergency department with a Global Registry of Acute Coronary Events (GRACE) score of 164. We performed urgent coronagraphy, which revealed multivessel lesions of coronary arteries with critical stenosis of coronary artery FIGURE 1.
Figure 1: Left coronary artery before stenting and right coronary artery before stenting.
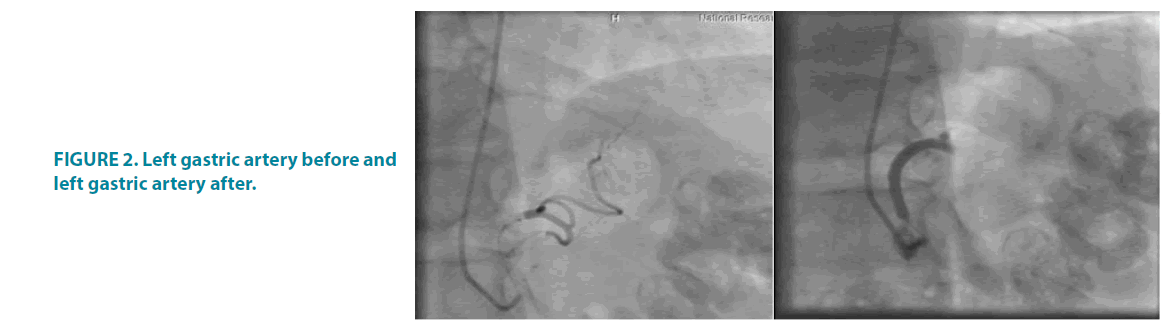
Cardiac surgery with shunting was planned for the following day, but we subsequently observed melena and the patient began vomiting with blood. Gastroscopy was performed and revealed the presence of stomach cancer on the sub cardinal region reaching the body of the stomach FIGURE 2. Pathology showed moderately differentiated stomach adenocarcinoma with necrosis. The hemoglobin level was 52 g/L and the patient was given a blood transfusion and stabilized medically with nitroglycerin for angina pectoris.
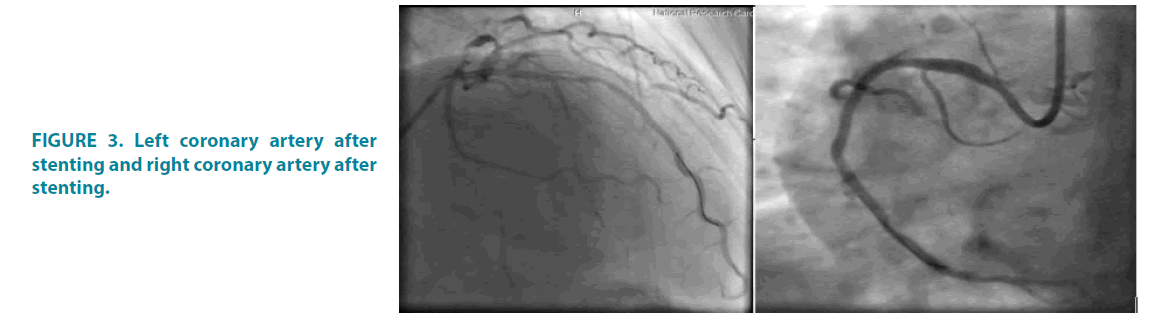
Five days later we performed simultaneous transcatheter embolization of the left gastric artery FIGURE 3 and Left Anterior Descending (LAD) and Right Coronary Artery (RCA) stenting.
Figure 3: Left coronary artery after stenting and right coronary artery after stenting.
The embolization of the left gastric artery was performed with the EmbGold Biosphere 500- 700 μm (Merit Medical) until the blood flow in the artery was stopped. After embolization, clopidogrel and aspirin were given to the patient. We performed stenting using drugeluting Resolute Integrity and Resolute Onyx stents (Medtronic).
The patient had a good recovery following the procedure. During the post-procedure hospital stay of 3 days, he did not complain of chest pain. There was some melena observed but clinical observation suggested the bleeding was minimal, despite ongoing use of clopidogrel and aspirin, and hemoglobin returned to acceptable levels before discharge (Hb 89 g/L).
Discussion
Recent European Society of Cardiology guidelines recommends against treating highrisk patients with dual antiplatelet therapy [1]. However, these patients require immediate revascularization, without which there would be a very poor prognosis in the short and longerterm [2]. Non-variceal Upper Gastrointestinal Bleeding (UGIB) is a relatively common complication in patients receiving antiplatelet therapy and is associated with an increased risk of recurrent ischemic events and mortality [3]. The dilemma of the current case was the combined risk of further cardiovascular morbidity and the risk of bleeding on dual antiplatelet therapy [4]. This patient had severe anemia as a result of gastrointestinal bleeding, which increases mortality to 14% among the common population [5]. At the same time, the cessation of antiplatelet and antithrombotic therapy in patient with ACS are also made prognosis worse [6]. Surgical treatment of UGIB was contraindicated and trans catheter arterial embolization has been established in this context as a favored therapeutic approach [7]. We performed coronary stenting with drugeluting stents immediately following arterial embolization with greater confidence in our application of dual antiplatelet therapy to this patient. Gastric bleeding was reduced to an acceptable level. The proton pump inhibitor therapy was recommended for the reduction of bleeding risk [8]. This case report suggests that gastric artery embolization is possible in patients with ACS complicated by acute upper gastrointestinal bleeding requiring stenting and dual antiplatelet therapy [9].
Conclusion
Dual Antiplatelet Therapy (DAPT) is normally contraindicated in the presence of gastrointestinal bleeding but in this case, transcatheter embolization of the gastric artery was achieved and allowed the immediate use of DAPT followed by coronary stenting. Prospective studies are needed to identify the optimal treatment approach in this complex clinical scenario.
References
- ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. 20, 21 (2015).
- Mohar DS, Seto AH, Kern MJ. Primary percutaneous coronary intervention in patients with st-segment–elevation myocardial infarction and concurrent active gastrointestinal bleeding. Circ Cardiovasc Interv. 8, 003058 (2015).
- Albeiruti R, Chaudhary F, Alqahtani F, et al. Incidence, predictors, and outcomes of gastrointestinal bleeding in patients admitted with st-elevation myocardial infarction. Am J Cardiol. 124, 343-348 (2019).
- Yasuda H, Matsuo Y, Sato Y, et al. Treatment and prevention of gastrointestinal bleeding in patients receiving antiplatelet therapy. World J Crit Care Med. 4, 40-46 (2015).
- Yavorsky RT, Wong RC, Maydonovitch C, et al. Analysis of 3294 cases of upper gastrointestinal bleeding in military medical facilities. Am J Gastroenterol. 90, 568-573 (1995).
- Yap FY, Omene BO, Patel MN, et al. Transcatheter embolotherapy for gastrointestinal bleeding: A single-center review of safety, efficacy, and clinical outcomes. Dig Dis Sci. 58, 1976-1984 (2013).
- Kikkert WJ, Hassell ME, Delewi R, et al. Predictors and prognostic consequence of gastrointestinal bleeding in patients with ST-segment elevation myocardial infarction. Int J Cardiol. 184, 128-134 (2015).
- Barkun AN, Almadi M, Kuipers EJ, et al. Management of nonvariceal upper gastrointestinal bleeding: guideline recommendations from the international consensus group. Ann Intern Med. 171, 805-822 (2019).
- Sehested TSG, Carlson N, Hansen PW, et al. Reduced risk of gastrointestinal bleeding associated with proton pump inhibitor therapy in patients treated with dual antiplatelet therapy after myocardial infarction. Eur Heart J. 40, 1963-1970 (2019).