Case Report - International Journal of Clinical Rheumatology (2024) Volume 19, Issue 12
Resolution of Psoriatic Arthritis After Breast Implant Removal
Sathvik Saineni1,2*, Ariail Schmitz1,2, Shazia Beg2, Neha Bhanusali2 and Maria Farooq2
1University of Central Florida HCA Florida Healthcare, USA
2Department of Internal Medicine, University of Central Florida College of Medicine, USA
- *Corresponding Author:
- Sathvik Saineni
University of Central Florida HCA Florida Healthcare, USA
E-mail: sathvik.saineni@ucf.edu
Received: 28-Oct-2024, Manuscript No. fmijcr-24-151344; Editor assigned: 29- Oct-2024, Pre-QC No. fmijcr-24-151344 (PQ); Reviewed: 13-Nov-2024, QC No. fmijcr-24-151344; Revised: 26- Nov- 2024, Manuscript No. fmijcr-24-151344 (R); Published: 04-Dec-2024, DOI: 10.37532/1758-4272.2024.19(11).200-203
Abstract
Breast Implant Illness (BII) is a complex condition characterized by various systemic symptoms, often linked to autoimmune responses. This case report presents a unique instance of new-onset psoriatic arthritis (PsA) in a 43-year-old woman with a history of autoimmune disorders, which resolved entirely following the removal of her breast implants. The patient’s PsA symptoms, including joint pain, onycholysis, and fatigue, manifested 3-4 months after undergoing saline breast implantation. Despite the use of multiple disease-modifying antirheumatic drugs (DMARDs), her symptoms persisted until the breast implants were removed, after which she experienced complete resolution, obviating the need for further biologic therapy. The precise mechanisms linking BII to autoimmune disorders are not well understood, but chronic inflammation triggered by breast implants as foreign bodies, silicone and platinum leaching, and the formation of biofilms have been proposed as potential contributors. This case is particularly noteworthy as the first documented instance of new-onset PsA directly associated with breast implants. While previous studies have established connections between breast implants and other autoimmune diseases, such as rheumatoid arthritis and systemic lupus erythematosus, this case broadens the scope of autoimmune manifestations potentially triggered by BII. Given the temporal relationship between implant placement and disease onset, clinicians should consider BII as a differential diagnosis in patients presenting with new-onset or unexplained autoimmune conditions, particularly when traditional therapies fail. The complete resolution of PsA symptoms following implant removal in this case underscores the importance of considering environmental factors in the management of autoimmune diseases. Furthermore, it suggests that breast implant removal may serve as a therapeutic option for select patients with autoimmune conditions linked to BII. This case highlights the need for further research to elucidate the mechanisms underlying the association between breast implants and autoimmune disorders, as well as to identify appropriate therapeutic strategies for affected patients.
Keywords
Breast implant illnessâ Psoriatic arthritisâ Autoimmune diseasesâ Implant removal.
Introduction
Breast Implant Illness (BII) is a complex and often debilitating condition characterized by a wide array of systemic symptoms that patients attribute to their breast implants. These symptoms can encompass fatigue, cognitive dysfunction, joint and muscle pain, hair loss, rashes, and a variety of other complaints that significantly impact quality of life. While the precise mechanisms underlying BII remain poorly understood, a growing body of evidence suggests a potential association between breast implants and the development or exacerbation of autoimmune disorders. Conditions such as rheumatoid arthritis, Sjogren's syndrome, systemic lupus erythematosus, and systemic sclerosis have been reported in some individuals with breast implants, raising concerns about the potential for an autoimmune-mediated response triggered by the implants. This case report presents a unique and compelling observation of a patient who developed new-onset psoriatic arthritis (PsA) following saline breast implantation. Psoriatic arthritis is a chronic inflammatory condition affecting the joints and skin, often associated with psoriasis. The temporal relationship between the onset of PsA symptoms and the presence of breast implants in this patient raises the possibility of a causal link, although further investigation is needed to establish a definitive connection. Notably, the patient's PsA symptoms completely resolved after the removal of her breast implants, further supporting the hypothesis that the implants may have played a role in triggering or exacerbating the autoimmune condition.
Case Presentation
A 43-year-old woman with a complex medical history, including alopecia totalis, Hashimoto's thyroiditis, celiac disease, plaque psoriasis, polycystic ovary syndrome (PCOS), and prior gastric bypass surgery, presented with a new onset of seronegative inflammatory oligoarthritis and onycholysis (nail separation), consistent with a diagnosis of psoriatic arthritis (PsA). Her joint symptoms manifested approximately 3-4 months after undergoing saline breast implantation. Around the same time, she noticed recurrence of her psoriasis which had been inactive for several years.
The patient reported pain in her left wrist, bilateral thumbs, bilateral second metacarpophalangeal (MCP) joints, right fifth MCP joint, right second and third metatarsophalangeal (MTP) joints, and lower back/right hip. She also experienced joint swelling in her hands, morning stiffness lasting a few hours, fatigue, brain fog, and migraines. The patient's past medical history was significant for gastrointestinal bleeding and superior mesenteric vein thrombosis. Her surgical history included gastric bypass, bowel resection, and volvulus reversal. Her family history was notable for a paternal aunt with rheumatoid arthritis and a cousin with alopecia, but no family history of psoriasis or inflammatory bowel disease. She denied alcohol, tobacco, or drug use.
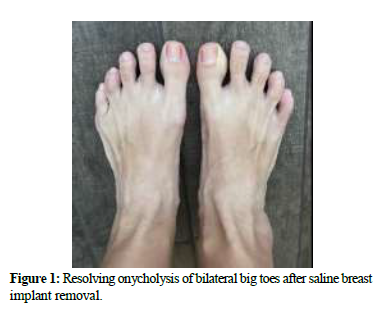
Physical examination revealed multiple clusters of healing psoriatic plaques on the patient's arms, legs, and abdomen, accompanied by onycholysis of both great toes. Notably, there was tenderness upon palpation of the proximal interphalangeal (PIP) joints in both hands and joints of the feet, with swelling specifically observed in the left second PIP joint.
Laboratory results were normal for Complete blood count, complete metabolic panel, Erythrocyte sedimentation rate, C-reactive protein, vitamin D, and thyroid stimulating hormone. Negative results were obtained for Rheumatoid factor, Cyclic citrullinated peptide antibody, HLA-B27, Anti-nuclear antibody, glucose-6-phosphate-dehydrogenase, Babesia, Anaplasma, Epstein Barr virus, QuantiFERON-TB Gold, Hepatitis panel, Lupus anticoagulant, Cardiolipin AB, and Beta-2 glycoprotein.
Radiographic imaging of the hands, wrists, ankles, and feet identified a left plantar calcaneal enthesophyte (bone spur), hardware in the right foot from previous surgery, and additional enthesophytes at the plantar fascia and Achilles tendon insertion sites. Apart from these findings, the imaging studies were unremarkable. A dual-energy X-ray absorptiometry (DEXA) scan revealed osteopenia (low bone density) in the left femoral neck.
The patient had a long history of unsuccessful treatment with various disease-modifying antirheumatic drugs (DMARDs), including hydroxychloroquine, methotrexate, tofacitinib, upadacitinib, adalimumab, and etanercept, due to primary failure, intolerance, or paradoxical reactions. Although secukinumab provided adequate joint response and was well-tolerated, it was discontinued before the removal of breast implants.
Following surgical removal of her breast implants, the patient experienced complete resolution of her joint pain, onycholysis (Figure 1), and fatigue, obviating the need for further biologic therapy.
Discussion
While the precise mechanisms underlying BII and its association with autoimmune disorders remain elusive, several hypotheses have emerged. A prominent theory suggests that breast implants, regardless of filler type, may act as a trigger for an immune response due to their nature as foreign bodies. This response, characterized by chronic inflammation, could potentially manifest as the systemic symptoms observed in BII patients [1]. Moreover, this chronic inflammation might exacerbate pre-existing autoimmune conditions or even trigger new-onset autoimmune diseases, as observed in the unique case presented in this report [2].
Silicone, a component of both saline and silicone gel implants, and platinum, a catalyst used in the manufacturing process, have been identified as potential culprits in BII. Studies have shown that these substances can leach from the implants and potentially act as triggers for autoimmune reactions [3]. Furthermore, the formation of biofilms on the surface of implants has been suggested as an additional contributing factor [4]. These biofilms, complex communities of microorganisms, may not only cause local complications but also contribute to systemic inflammation, potentially exacerbating autoimmune responses.
The case report presented here is particularly noteworthy as it details the first documented instance of new-onset psoriatic arthritis (PsA) directly attributed to breast implants. While previous studies have established links between breast implants and other autoimmune diseases such as rheumatoid arthritis and systemic lupus erythematosus [5], this case broadens the understanding of the potential autoimmune manifestations associated with BII. It highlights the need for clinicians to consider BII as a potential differential diagnosis in patients presenting with new-onset or unexplained autoimmune conditions, especially those with a history of breast implantation.
The complete resolution of PsA symptoms following implant removal in this case further supports considering environmental triggers in the management of autoimmune diseases. It also emphasizes the potential therapeutic benefit of implant removal in select patients experiencing autoimmune conditions associated with BII. This case report serves as a compelling reminder of the intricate interplay between environmental factors and autoimmune diseases, while also highlighting the potential risks associated with breast implants.
Conclusion
This case report emphasizes the need for heightened awareness of BII as a potential trigger or exacerbating factor in autoimmune diseases. While further research is needed to elucidate the exact mechanisms underlying this association, clinicians should consider breast implant removal as a potential therapeutic option for patients with autoimmune conditions who have failed conventional therapies and have a temporal relationship between implant placement and disease onset or exacerbation.
References
- Suh LJ, Khan I, Kelley-Patteson C, et al. Breast Implant-Associated Immunological Disorders. J Immunol Res. 8536149 (2022).
- Cohen Tervaert JW, Colaris MJ, van der Hulst RR. Silicone breast implants and autoimmune rheumatic diseases: myth or reality. Curr Opin Rheumatol. 29(4), 348-354 (2017).
- Coriddi M, Burke EA, Myers P, et al. Autoimmune Disease and Breast Implants: Systematic Review of Outcomes. Ann Plast Surg. 90(4), 385-388 (2023).
- Shons AR, Schubert W. Silicone breast implants and immune disease. Ann Plast Surg. 28(5), 491-501. (1992).
- Brown SL, Langone JJ, Brinton LA. Silicone breast implants and autoimmune disease. J Am Med Womens Assoc. 53(1), 21-24 (1998).
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref