Case Report - International Journal of Clinical Rheumatology (2020) Volume 15, Issue 4
Pregabalin-induced focal myositis: A report of two cases and review of literature
- Corresponding Author:
- Stephen Bell
Florida State University College of Medicine,
Internal Medicine Residency Program at
Sarasota Memorial Health Care System,
Sarasota, FL 34239, USA
E-mail: stephen-bell@smh.com
Abstract
Background: Drug-induced myopathy should be on the differential diagnosis in patients with non-traumatic muscle pain. It is important to consider the diagnosis as symptoms typically abate with removal of the offending agent. Case: Two elderly females presented separately with complaint of lower extremity pain and swelling. There was no elevation in inflammatory markers or muscle enzymes in either case. MRI revealed inflammatory changes on T2-weighted sequences. Both patients experienced rapid improvement of symptoms with discontinuation of pregabalin. Discussion: Medication-induced myositis should be considered in patients presenting with muscle complaints. Due to the overall high prevalence of pregabalin in the management of chronic pain, it is important to consider its role in the pathogenesis of focal myositis.
Abbreviations
ANA: Antineutrophil Antibody; CK: Creatine Kinase; CRP: C-Reactive Protein; ESR: Erythrocyte Sedimentation Rate; HMG-CoA: 3-Hydroxy-3-Methylglutaryl-Coenzyme A; LDH: Lactate Dehydrogenase; MRI: Magnetic Resonance Imaging; RA: Rheumatoid Arthritis
Introduction
There are many causes of acquired muscle disease making the diagnosis challenging. It is imperative during evaluation of such patients to consider medication-induced muscle injury because the condition is potentially reversible with discontinuation of the offending agent. Certain medications are known to cause myopathies due to an adverse drug reaction such as statins. However, other medications have been shown to cause myopathies as a consequence of rare toxic reactions [1]. There is a paucity of case reports of non-statin druginduced myositis, particularly those found to cause a focal myositis. Focal myositis is defined as muscle injury localized to a single skeletal muscle, often presenting in the lower extremities as a mass-like lesion or nodule [2,3].
Jonathon Jones et al. propose three general mechanisms by which medications cause myotoxicity:
• Impairment of energy and protein metabolism due to mitochondrial impairment
• Induction of necrotizing myositis and
• Impairment of autophagy.
Of the three generalized mechanisms, disruption of impaired cellular energy metabolism is the most common [1]. Additionally, certain medications can affect intracellular organelles other than mitochondria including lysosomes and myofibrillary proteins. Alterations of muscle antigens and the myocyte milieu can lead to an immune-mediated response and inflammation. Furthermore, perturbations in electrolytes and other small molecules can lead to dysfunction at the cellular level leading to myotoxicity [4].
Medication-induced myopathy is a diagnosis of exclusion. It is important to rule out other causes such as thyroid disease, infection, metabolic derangements, and malignancy among others. Laboratory studies often used in support of inflammatory myopathies include serum Creatine Kinase (CK), Erythrocyte Sedimentation Rate (ESR), C-Reactive Protein (CRP), aldolase, Lactate Dehydrogenase (LDH), Anti-Neutrophil Antibody (ANA), and anti-synthetase antibodies when clinically appropriate [2]. Magnetic Resonance Imaging (MRI) can reveal hyperintense T2 signal indicating soft tissue edema which suggests localized inflammation [5]. Here we present two cases of drug-induced focal myositis presumed to be related to pregabalin use.
Case 1
An 80-year-old female presented to the emergency department from a rehabilitation facility with right leg pain beginning one week prior to presentation. The pain was described as throbbing and localized to the anterolateral aspect of the distal right lower extremity. The patient denied any generalized weakness, fever, diaphoresis, unintentional weight loss, or other symptoms. There was no history of trauma and no clinical evidence of skin or soft tissue infection. She was recently hospitalized 3 weeks prior to presentation for lower back pain associated with intractable left leg pain and underwent lumbar spinal fusion and decompression surgery. Her past medical history included seropositive Rheumatoid Arthritis (RA), Sjogren’s syndrome, limited cutaneous scleroderma, osteoarthritis, fibromyalgia, lumbar spinal stenosis, and gastro-esophageal reflux disease. Her home medications included methotrexate, folic acid, prednisone, diltiazem, rosuvastatin, zolpidem, tapentadol, and oxycodone. Her methotrexate was discontinued postoperatively by the orthopedic surgery service due to concerns for impaired wound healing, and unfortunately, the patient developed a severe RA flare. She was started on prednisone and pregabalin at the rehabilitation facility one week prior to the current hospitalization. The prednisone was started at 30 mg daily and was tapered to 20 mg daily. Prior to admission pregabalin was started at 50 mg twice daily and titrated up to 175 mg twice daily.
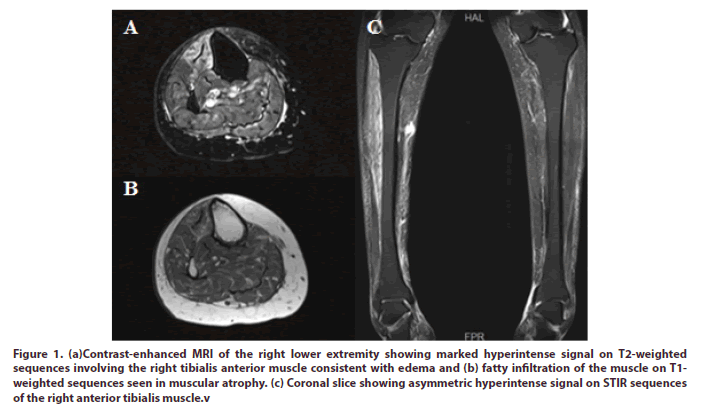
On examination, the patient was afebrile and hemodynamically stable. There was no appreciable swelling of the lower extremities. Homan’s sign was negative. There was no skin erythema or warmth. The patient was neurovascularly intact. There was tenderness to palpation over the right anterior shin. Musculoskeletal exam was remarkable for diffuse synovitis in the shoulders, elbows, wrists, metacarpophalangeal joints, proximal interphalangeal joints 2-5 in the hands bilaterally, knees, subtalar joints, and metatarsophalangeal joints. Muscle strength was 4 out of 5 grossly with the exception of 3 out of 5 strength with right ankle dorsiflexion. Generalized sarcopenia was noted. The rest of the physical examination was unremarkable. Laboratory studies were as shown in Table 1. An x-ray of the right tibia/fibula showed calcaneal enthesophytes, but was negative for soft tissue edema, periosteal lifting, fracture, or dislocation. A non-contrast MRI of the right lower extremity revealed nonspecific intramuscular edema of the tibialis anterior muscle (Figure 1).
Figure 1: (a)Contrast-enhanced MRI of the right lower extremity showing marked hyperintense signal on T2-weighted sequences involving the right tibialis anterior muscle consistent with edema and (b) fatty infiltration of the muscle on T1- weighted sequences seen in muscular atrophy. (c) Coronal slice showing asymmetric hyperintense signal on STIR sequences of the right anterior tibialis muscle.v
The patient was started on methotrexate 20 mg subcutaneous weekly. The prednisone was slowly tapered over the course of several weeks until the patient was maintained on 5 mg daily. Due to suspected medication side effect, the pregabalin was tapered by 50 mg daily over three days starting at 100 mg twice daily until the patient was on 50 mg twice daily, and was subsequently discontinued. The patient was seen in the clinic 3 days after initial presentation at which time she was on prednisone 15 mg daily and almost tapered off pregabalin. She reported marked improvement in the right lower extremity pain, as well as, a modest improvement in her RA flare.
Case 2
A 69-year-old female presented to the clinic for evaluation of left calf pain. The pain was sharp, non-radiating, and associated with progressive swelling in the distal lower extremity. Symptoms improved with elevation and worsened with activity. There was no history of trauma or recent prolonged immobility. The patient’s medical history included mixed connective tissue disease, RA, subacute cutaneous lupus erythematosus, chronic pain syndrome, ulcerative colitis, osteoporosis, and hypothyroidism. Her home medications included mycophenolate, prednisone, denosumab, nortriptyline, diclofenac, and apixaban. She was started on pregabalin 75 mg twice daily for pain management two weeks prior to the current presentation.
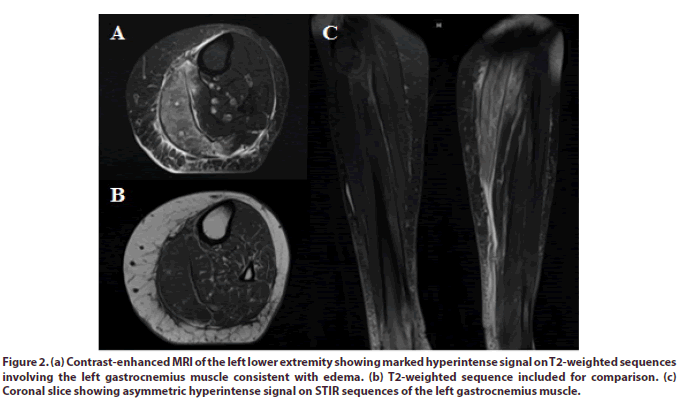
On examination, she was in noticeable discomfort. She was afebrile and hemodynamically stable. There was mild erythema and swelling over the medial aspect of the plantar surface of the left foot. There was marked tenderness over the posterior aspect of the left calf. Homan’s sign was negative. There was no appreciable synovitis in the upper or lower extremities. Muscle strength was 4 out of 5 in all muscle groups except for 3 out of 5 strength with plantarflexion of the left ankle. Laboratory studies were as shown in Table 1. An MRI of the left lower extremity revealed nonspecific edema of the left gastrocnemius muscle and surrounding subcutaneous tissues (Figure 2).
Figure 2: (a) Contrast-enhanced MRI of the left lower extremity showing marked hyperintense signal on T2-weighted sequences involving the left gastrocnemius muscle consistent with edema. (b) T2-weighted sequence included for comparison. (c) Coronal slice showing asymmetric hyperintense signal on STIR sequences of the left gastrocnemius muscle.
Table 1. Laboratory values.
| Lab test | Results | Reference range | |
|---|---|---|---|
| Case 1 | Case 2 | ||
| white blood cell | 14.8 | 4.6 | 4.5-11.0 x 103/µL |
| hemoglobin | 10 | 11 | 11.6-16.1 g/dL |
| Platelets | 444 | 255 | 150-450 x 103/µL |
| Sodium | 137 | 138 | 131-145 mmol/L |
| potassium | 4.2 | 4.2 | 3.5-5.1 mmol/L |
| blood urea nitrogen | 18 | 19 | 8-23 mg/dL |
| creatinine | 0.64 | 0.76 | 0.55-1.02 mg/dL |
| Glucose | 171 | 84 | 70-100 mg/dL |
| AST | 14 | 31 | 15-37 U/L |
| ALT | 26 | 36 | 13-56 U/L |
| ALP | 143 | 47 | 33-149 U/L |
| total bilirubin | 0.1 | 0.4 | 0.2-1.3 mg/dL |
| Albumin | 2.6 | 4.1 | 3.2-4.8 g/dL |
| ESR | 25 | 11 | 0-30 mm/hr |
| CRP | 1.5 | < 8.0 mg/L | |
| Aldolase | 7.1 | 4.4 | ≤ 8.1 U/L |
| lactate dehydrogenase | 257 | 84-246 U/L | |
| creatine kinase | 63 | < 10 | 26-192 U/L |
| ANA | positive | Negative | |
| ANA titer | 0.486111111 | < 1:40 | |
| ANA-H2S | positive | Negative | |
AST: Aspartate Transaminase; ALT: Alanine Transaminase; ALP: Alkaline Phosphatase; ESR: Erythrocyte Sedimentation Rate; CRP: C-Reactive Protein; ANA: Anti-Neutrophil Antibody; H2S: Hep-2 Substrate
There was a suspected adverse drug reaction to pregabalin as in the previous case. As such, the pregabalin was discontinued. The patient experience rapid improvement in the pain and swelling within one week. She was seen in the rheumatology clinic 2 weeks later with minimal residual pain and no swelling. We are happy to report by 4 weeks all symptoms resolved.
Discussion
Drug-induced myopathy is a heterogenous group of disordered with variable presentations. Symptoms typically include muscle pain, weakness, or swelling, and may be accompanied by elevations in CK or aldolase. Many drug-related myopathies are potentially reversible at early stage and heightened suspicion is required to make the diagnosis. Prompt identification and cessation can prevent irreversible damage and improve outcomes. The most widely recognized medication class to cause myalgias are the 3-hydroxy-3methylglutaryl-coenzyme A (HMG-CoA) reductase inhibitors known as statins. Statins are more likely to cause a syndrome of oligo- or polymyalgia which is not what was observed in these cases. There are 4 clinically recognized phenotypes:
• Rhabdomyolysis
• Myalgia and/or mild elevation in CK
• Self-limited toxic myopathy and
• Immune-mediated necrotizing myopathy and anti- HMGCoA reductase antibodies [6].
A study by Berent at al. showed 96.5% of 1,111 study participants complaining of myalgia has normal CK levels. The pectoral muscle was most commonly involved, followed by quadriceps femoris, biceps brachii, and deltoid muscles [7].
These two cases are thought to represent unique adverse drug reactions. There have been no similarly described cases in the literature with pregabalin-mediated myositis. However, there are reports of rhabdomyolysis associated with Lyrica® and asymptomatic elevations in CK (1.5% compared to 0.7% placebo) in premarketing clinical trials although the clinical significance of these findings remains unclear [8]. Both cases share similar presentations and responses to discontinuation of pregabalin which supports the diagnosis. Our index of suspicion for an inflammatory myositis remained low due to normal inflammatory markers and muscle enzymes. It is important to consider glucocorticoidmediated myopathy in the first case due to the recent increase in the patient’s home prednisone dosage. Glucocorticoid-induced myopathy can present in an acute form or chronic form. In contrast to these cases, acute glucocorticoid-induced myopathy typically presents in the critical care setting with diffuse polymyopathy with progressive weakness in the setting of high dosages of steroids [9].
Focal myositis is a rare disorder usually isolated to one skeletal muscle or muscle group. In addition to medications it has been attributed to rheumatic disease, trauma, and neoplasia. In such cases, it is unclear whether it is a separate disease entity or part of a syndrome [3]. Frequently patients are often mistreated as a case of cellulitis or suspected of having a deep venous thrombosis [10]. Musculoskeletal ultrasound may be used to help with the diagnosis and may show hypoechoic enlargement of the muscle with preservation of the muscle fiber orientation [11].
Pregabalin has become ubiquitous in the management of chronic pain syndromes. Although, it has been shown to cause asymptomatic myopathy in premarketing trials, it is not a known agent of cause myositis. More investigation is needed to determine its potential role in this pathogenesis. Both of these patients had generalized sarcopenia which we suspect may have put them at higher risk, but this needs to be investigated in further studies.
Acknowledgments
Not applicable
Funding
Not applicable
Competing and conflicting interests
The authors declare that they have no competing interests.
References
- Jones JD, Kirsch HL, Wortmann RL et al. The causes of drug-induced muscle toxicity. Curr. Opin. Rheumatol. 26(6), 697–703 (2014).
- Devic P, Gallay L, Streichenberger N et al. Focal myositis: A review. Neuromusculo. Disord. 26(11), 725–733 (2016).
- Gallay L, Hot A, Petiot P et al. Focal myositis: New insights on diagnosis and pathology. Neurology. 90(12), e1013–e1020 (2018).
- Valiyil R, Christopher-Stine L. Drug-related myopathies of which the clinician should be aware. Curr. Rheumatol. Rep. 12(3), 213–220 (2010).
- Coupal TM, Chang DR, Pennycooke K et al. Radiologic findings in gabapentin-induced myositis. J. Radiol. Case. Rep. 11(4), 30–37 (2017).
- Selva-O’Callaghan A, Alvarado-Cardenas M, Pinal-Fernández I et al. Statin-induced myalgia and myositis: An update on pathogenesis and clinical recommendations. Expert. Rev. Clin. Immunol. 14(3), 215–224 (2018).
- Berent T, Berent R, Steiner S et al. Statin-induced muscular side effects at reset and exercise – An anatomical mapping. Atheroscler. Suppl. 40, 73–78 (2019).
- https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/021446s026,022488s005lbl.pdf
- Pereira RMR, de Carvalho JF. Glucocorticoid-induced myopathy. Joint. Bone. Spine. 78(1), 41–44 (2011).
- Aslam F, Fox M, Chang-Miller A. Ultrasound for the rheumatologist – Focal myositis. Acta. Rheumatol. Port. 42(4), 336–338 (2017).
- Laurent PE, Larribe M, Guenoun D et al. Focal myositis: Sonographic findings. Muscle. Nerve. 52(2), 306–307 (2015).