Case Report - International Journal of Clinical Rheumatology (2021) Volume 16, Issue 6
Patterns of Pulmonary Involvement in an Egyptian Cohort with Autoimmune Diseases: A Descriptive Study
- *Corresponding Author:
- Reem Hamdy A Mohammed
Department of Rheumatology and Rehabilitation, School of Medicine, Cairo University, Egypt
E-mail: rmhamdy@yahoo.com
Abstract
Pulmonary involvement has been reported as a major contributor to significant morbidity and poor disease outcome in a myriad of autoimmune collagen vascular diseases.
Aim of the work: To screen and to describe the different patterns of pulmonary involvement in a cohort of Egyptian patients with autoimmune diseases.
Patients and methods: A cross sectional study conducted on patients attending the outpatient clinic as well as inpatient ward of rheumatology and rehabilitation and chest departments in Kasr Al Ainy teaching hospital- School of Medicine Cairo University in the period from January 2017 to January 2019. Approval and registration of the research by the institutional review board for research ethics was fulfilled prior to initiation of the study. HRCT chest was done to all patients using 16 channels MSCT in Kasr Al Ainy. Reconstructed axial, coronal and sagittal images were done to all patients; complementary mediastinal images were additionally taken. Results: Parenchymal lung disease in the form of interstitial pneumonitis with variable degrees of fibrosis (IPF) were encountered in 48% of the study cohort. Features suggestive of pulmonary hypertension with prominent PA diameter was found in 33% of cases. Mediastinal lymph node enlargement was noted in 34% of cases.
Conclusion: Pulmonary involvement is not uncommon in patients with autoimmune diseases. High resolution CT chest remains the most sensitive technique for early detection of parenchymal lung disease in these patients.
Keywords
collagen vascular diseases • pulmonary affection • parenchymal lung disease • high resolution computerized tomography
Introduction
Pulmonary involvement has been reported as a major contributor to significant morbidity and poor disease outcome in a myriad of autoimmune collagen vascular diseases. The most identified forms in the given study were the ones with rheumatoid arthritis, progressive systemic sclerosis, mixed connective tissue disease, poly-dermatomyositis and systemic lupus erythematosus [1, 2]. High-resolution Computed Tomography (CT) has proved to play an integral role in the detection and characterization of various histo-pathologically confirmed interstitial lung diseases in patients with collagen vascular diseases [3]. Parenchymatous lung involvement might exist in various forms including: Usual Interstitial Pneumonia (UIP), Nonspecific Interstitial Pneumonia (NSIP), cryptogenic organizing pneumonia, diffuse alveolar damage, Lymphocytic Interstitial Pneumonia (LIP), and apical fibrosis [2].
This study aimed to screen and to describe the different patterns of pulmonary involvement in a cohort of Egyptian patients with autoimmune diseases.
Patients and methods
This is a cross sectional study that aimed to screen for patterns of pulmonary involvement in patients with immune mediated collagen vascular diseases using the High- Resolution Computerized Tomography (HRCT) scanning techniques of the chest evaluated by an expert radiologist. The study was conducted on patients attending the outpatient clinic as well as inpatient ward of rheumatology and rehabilitation and chest departments in Kasr Al Ainy teaching hospital- School of Medicine Cairo University in the period from January 2017 to January 2019. Approval and registration of the research by the institutional review board for research ethics was fulfilled prior to initiation of the study.
Inclusion criteria: patients with the established diagnosis/ classification of immune mediated collagen vascular disease according to the American College of Rheumatology (ACR) [4-9]. With clinical features suggestive of pulmonary involvement. Exclusion Criteria: Patient with known associated chest diseases and non-immune mediated pulmonary pathology e.g., tuberculosis. Patients with history of smoking.
All patients were subjected to; thorough clinical examination with history taking, general and chest examination and laboratory investigations including serological tests required to confirm classification of an autoimmune diseases were done. HRCT chest was done to all patients using 16 channels MSCT in Kasr Al Ainy. Reconstructed axial, coronal and sagittal images were done to all patients; complementary mediastinal images were additionally taken.
Statistical analysis was done using the package of statistical analysis used was SPSS version 21. The data was coded, tabulated and analyzed by SPSS. Numerical data was presented by mean and standard deviation. Qualitative data was presented by frequency and percentage. Non-parametric tests as chi-squared test and fisher exact test were used on cells less than 50%.
Results
The research included 100 patients (12 males and 88 females), age range 13 years to 72 years (mean 40.64 ± 13.38 years. They included: 31 patients with the diagnosis of rheumatoid arthritis- RA (31%, 25 females and 6 males), 28 patients with the diagnosis of systemic sclerosis- Ssc (28%, 27 females and 1 male), 24 patients with the diagnosis of Systemic lupus erythematosus- SLE (24%, 22 females and 2 males), 8 patients with the diagnosis of dermatomyositis- DM (8%. 6 females and 2 males), 8 patients with mixed connective tissue disease- MCTD (8%, 7 females and 1 male), and one female patients with the diagnosis of Sjogren’s syndrome. All patients presented with dyspnea and/or dry cough and / or expectoration. The frequency of these manifestations in each disease category were as follows: in RA patients 20(64.5%) had dyspnea as the presenting symptom, 8(25.9%) had dry cough, 3(9.6%) had productive cough, while patients affected by SSc 17(60.7%) had dyspnea, 9(32.3%) had dry cough, 2(7%) had productive cough. In SLE patients 15(62.5%) had dyspnea, 6(25%) had dry cough and 3(12.5%) had productive cough, for patients with DM 7(87.5%) had dyspnea as a presenting symptom, 1(12.5%) had dry cough and none had productive cough. In MCTDs we had 6 patients (75%) having dyspnea as the presenting symptom and 1 patient (12.5%) with dry cough with another patient 1(12.5%) with productive cough. The patient with Sjogren’s syndrome had dyspnea only with no other manifestations at suspicion.
Results of the HRCT in the studied patients revealed
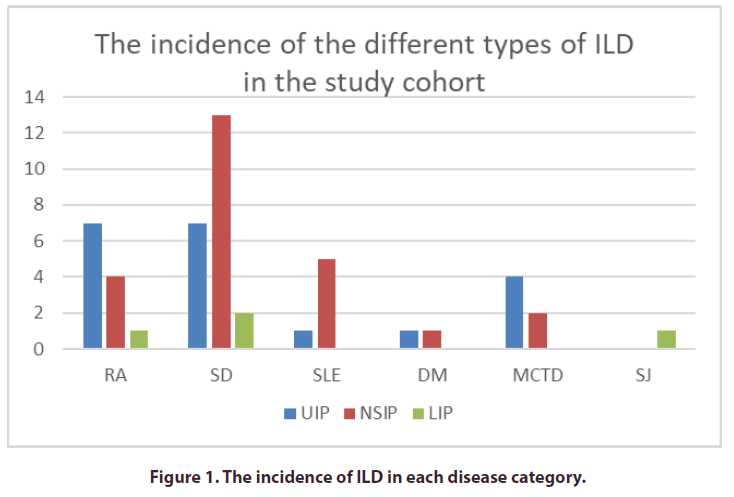
Parenchymal lung disease in the form of interstitial pneumonitis with variable degrees of fibrosis; IPF were encountered in 48% of the cases with bilateral symmetrical predominantly subpleural basal lesions and involvement of the pleural recesses. According to the patterns and distribution of the parenchymal lung disease patients were further classified into usual interstitial pneumonia UIP, non-specific interstitial pneumonia NSIP and lymphocytic interstitial pneumonia LIP. NSIP was the most common type of ILD, found in approximately 24 patients (24% of cases) followed by UIP found in 20 patients (20% of cases) and LIP was the least common type of ILD, found in only 4 patients (4% of cases).
Results of HRCT findings in each disease category
Among patients with RA, UIP was the most common type of ILD, found in approximately 7 of 31(22.5%) cases followed by NSIP found in 4 of 31 (13%) cases and LIP was the least common type of ILD, found in only 1(3%) of cases. In patients with Ssc, NSIP was the most common type of ILD, found in approximately 13 of 28(46%) cases followed by UIP found in 7 of 28(25%) cases and LIP again was the least common type found in only 2(7%) of cases. In patients with the diagnosis of SLE, NSIP was the most common type of ILD found in approximately 4 of 24(16.6%) cases followed by UIP found in 1(4%) of cases, while LIP was not recorded among this disease group. However, in patients with DM both UIP and NSIP had the same incidence found in 1(12.5%) of cases while LIP was not recorded among this disease group. In patients with MCTD, UIP was the most common type of ILD found in 4 of 8 (50%) cases followed by NSIP which was found in 2 of 8(25%) cases while LIP was not recorded among this disease group and finally in the female patient with Sjogren syndrome the HRCT showed features of LIP (Figure 1).
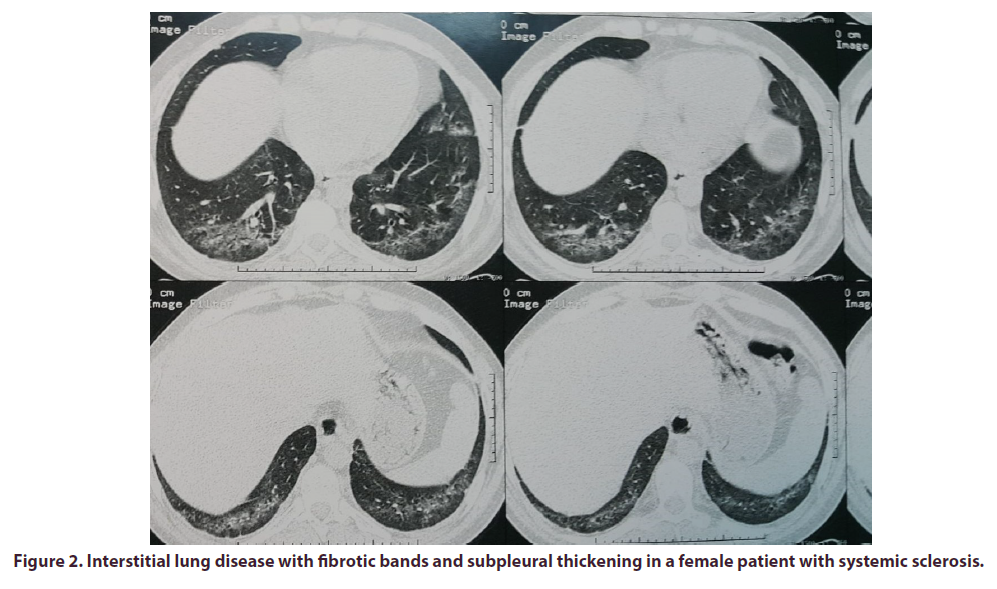
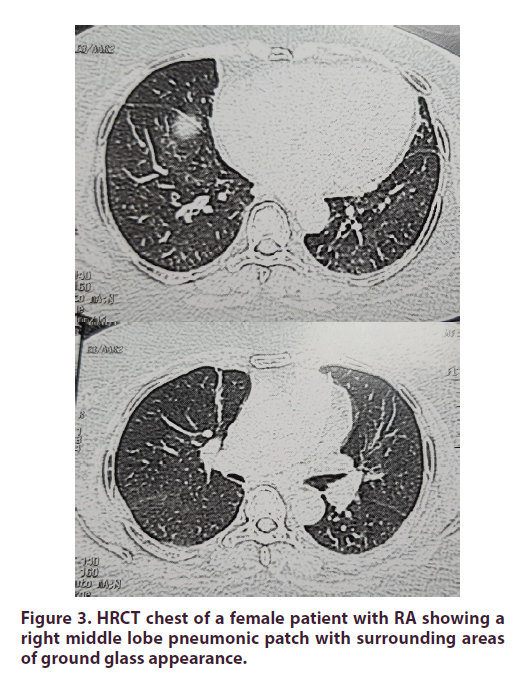
Airway disease was detected in 31 (31%) of the patients. Signs of airways diseases include hyperlucency and bronchial wall thickening. Twenty-four cases showed associated centrilobular nodules reflecting small airway disease of whom 18 cases had a patulous esophagus suggesting aspiration bronchiolitis. The remaining cases thus were considered follicular bronchiolitis by HRCT signs. Mosaic perfusion was noted in 8 cases suggesting bronchiolitis obliterans. Among patients with RA, 4 of 31(13%) cases had airway disease, all of them had bronchial wall thickening and dispersed centrilobular nodules, 3 of them showed hyperlucency and only one case had mosaic pattern of attenuation, 2 of 4 cases had associated patulous esophagus which could suggest aspiration bronchiolitis. In patients with Ssc; 14 of 28(50%) cases had airway disease.12 of 14 cases had bronchial wall thickening, 7 of 14 cases showed hyperlucency, 4 of 14 cases showed mosaic pattern of attenuation and 3 of 14 cases showed dispersed centrilobular nodules. All of cases had associated patulous esophagus and or AF level within esophagus which could suggest aspiration bronchiolitis and 10 of cases had associated IPF. In patients with SLE, 6 of 24(25%) cases had airway disease. 4 of 6 cases had bronchial wall thickening, 2 of 6 cases showed hyperlucency, 2 of 6 cases showed mosaic pattern of attenuation and 3 of 6 cases showed dispersed centrilobular nodules. Patients with DM; 3 of 8(37.5%) cases had airway disease. All of the cases had bronchial wall thickening and hyperlucency, and only one case showed dispersed centrilobular nodules. In MCTD, 4 of 8 (50%) cases had airway disease.4 of 8 cases had bronchial wall thickening, 2 of 8 cases showed mosaic pattern of attenuation. 2 of 4 cases had associated patulous esophagus which could suggest aspiration bronchiolitis and associated IPF. In the female patient with Sjogren syndrome there were no signs of airway disease. Traction bronchiectasis and bronchiolectasis was identified in 42 (42%) of patients with IPF (Figures 1-3).
Figure 2. Interstitial lung disease with fibrotic bands and subpleural thickening in a female patient with systemic sclerosis.
Assessment of the mediastinal images and measurements of the Pulmonary artery diameter
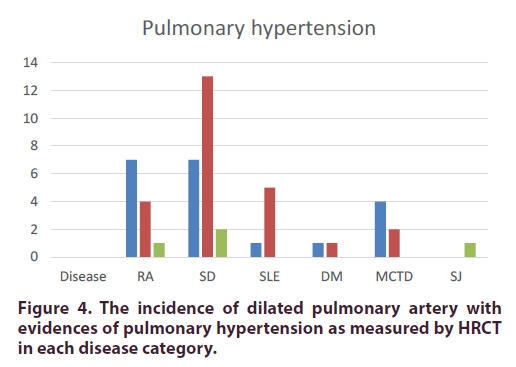
HRCT revealed features suggestive of pulmonary hypertension with prominent PA diameter more than 2.9 cm, exceeding that of the adjacent ascending aorta and associated complications as right sided ventricular dilatation and pericardial effusion in 33% of cases. The range and mean for PA diameters in each disease category are shown in Table 1 and Figure 4.
| Disease | Highest PA dimension | Lowest PA dimension | Median |
|---|---|---|---|
| RA | 3.7 cm | 2.9 cm | 3.2 cm |
| Ssc | 3.5 cm | 2.9 cm | 3.1 cm |
| SLE | 4.5 cm | 3.1 cm | 3.5 cm |
| DM | 3 cm | 2.9 cm | 2.9 cm |
| MCTD | 3.4 cm | 3 cm | 3.1 cm |
| SJ | 3 cm |
Table 1. The range and mean for PA diameters in each disease category.
Figure 4. The incidence of dilated pulmonary artery with evidences of pulmonary hypertension as measured by HRCT in each disease category.
Other features encountered during HRCT exam in the population studied
Thirty-three patients (33%) had pericardial affection in form of effusion or thickening. Pleural affection (effusion or thickening) was recorded in 12 of studied cases (12%). Cardiomegaly was noted in 17 % of cases. Mediastinal lymph node enlargement was noted in 34% of cases. The distribution of mediastinal among patients with RA mediastinal lymphadenopathy was noted in 11 of 31(35%) cases, with perivascular group affected in 5 cases, retrocaval group affected in 5 of cases and subcarinal in one case. The affected node dimension ranges from 1 cm to 2.1 cm (average of 1.58 cm). In Ssc mediastinal lymphadenopathy was noted in 8 of 28(28.5%) cases, with perivascular group affected in 4 cases, retrocaval group affected in 4 of cases. The affected node dimension ranges from 1.1 cm to 2.35 cm (average of 1.52 cm). In MCTD mediastinal lymphadenopathy was noted in 2 of 8 (25%) cases, with perivascular group affected in one case, retrocaval group affected in one case. The affected node dimension ranges from 1.2 cm to 1.5 cm (average of 1.35 cm). Inpatients with SLE, DM and only Sjogren case, no significant mediastinal lymphadenopathy was noted. Esophageal abnormality was recorded in 28% of cases in form of patulous thoracic esophagus and or presence of air fluid level within (Table 2).
| Disease | RA | SSc | SLE | DM | MCTD | SJ |
|---|---|---|---|---|---|---|
| IPF | 39% | 78.50% | 20% | 25% | 75% | 100% |
| Airway disease | 13% | 50% | 25% | 37.50% | 50% | 0% |
| Pulmonary hypertension | 33% | 32% | 8% | 62.50% | 50% | 100% |
| Pericardial affection | 16% | 28.50% | 62.50% | 37.50% | 25% | 0% |
| Pleural affection | 6.40% | 3.50% | 33.30% | 0% | 12.50% | 0% |
| Cardiomegaly | 3% | 25% | 25% | 12.50% | 25% | 0% |
| Mediastinal lymphadenopathy | 35% | 28.50% | 25% | 0% | 0% | 0% |
| Esophageal dysmotility | 9% | 82% | 25% | 0% | 0% | 0% |
Table 2. Collective incidence of each thoracic manifestation among each CVD group.
Discussion
Pulmonary involvement in collagen vascular diseases is a frequently encountered disease related comorbidity particularly in patients with rheumatoid arthritis, progressive systemic sclerosis, systemic lupus erythematosus, polymyositis and dermatomyositis, mixed connective tissue disease, and Sjögren syndrome [1]. Interstitial lung disease has been reported as the most prevalent form of lung involvement in patients with autoimmune disease compared to airway disease [2, 10]. High-resolution Computed Tomography (CT) plays an integral role in the early detection and characterization of the various patterns of interstitial lung affection in these patients considering the limited diagnostic value of traditional plain radiography being less sensitive to early changes [2, 10-13]. The presented study is a cross sectional study that included a sample of 100 patients with the established diagnosis of CVD and displaying clinical manifestations suggestive of pulmonary involvement. HRCT chest was done to eligible cases in Kasr Al Ainy Hospital’s radiology department in the period from January 2017 to January 2019. Authors aimed to report and describe the encountered findings in the population surveyed using the HRCT being a sensitive technique. In the studied population of patients with established collagen vascular diseases interstitial pulmonary fibrosis was noted in 48% of the surveyed cases with NSIP as the most common type of ILD, being reported in approximately 25% of cases followed by UIP found in 20% of cases and LIP was the least common type of ILD, found in only 4% of cases, which agrees with data reported in the literature [14, 15]. The study additionally highlighted other forms of lung involvement apart from the parenchymal disease where pulmonary hypertension was reported in 33% of cases a finding that has been well identified in patients with CVD [16, 17]. Evidence of serositis including pericardial and pleural effusion with or without thickening was found in 33% and 12% of cases respectively another common feature described in patients with CVD form different ethnic groups [18- 23]. Mediastinal lymphadenopathy was noted in 34% of cases, which agrees with Finally in our Egyptian cohort esophageal dilatation occurred in 28% of cases, which agrees with the findings reported by Capobianco et al., 2011 who stated that patients with CVD have a higher risk of esophageal dysmotility [2].
Conclusion
The current study represents a descriptive study on a sample of Egyptian patients with autoimmune diseases who had symptoms suggestive of pulmonary. The study confirmed the presence of different forms of parenchymal lung disease in addition to vascular, serosal and mediastinal findings in the screened cohort of Egyptian patients with collagen vascular diseases. The study has some limitations including the limited financial support which affected the potential to include larger population for HRCT chest. The presence of some relatively uncommon diseases including SS cans Sjogren which might indirectly affect the interpretation of results. The lack of an associated pulmonary function testing to compare the findings to the functional status of the patients assessed.
Conflict of interest
None Declared.
References
- You-Jung Ha, Yun Jong Lee, Eun Ha Kang. Lung Involvements in Rheumatic Diseases: Update on the Epidemiology, Pathogenesis, Clinical Features, and Treatment. Biomed. Res. Int. 2018, 19 (2018).
- Capobianco J, Grimberg A, Thompson B et al. Thoracic Manifestations of Collagen Vascular Diseases. Radiographics. 32(1), 33–50 (2011).
- Pontana F, Billard AS, Duhamel A et al. Effect of iterative reconstruction on the detection of systemic sclerosis-related interstitial lung disease: clinical experience in 55 patients. Radiology. 279(1), 297–305 (2016).
- Aletaha D, Neogi T, Silman AJ et al. 2010 Rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis. Rheum. 62, 2569–2581 (2010).
- Avouac J, Fransen J, Walker U et al. Preliminary criteria for the very early diagnosis of systemic sclerosis: results of a Delphi Consensus Study from EULAR Scleroderma Trials and Research Group. Ann. Rheum. Dis. 70(3), 476–481 (2011).
- Lundberg IE, Tjärnlund A, Bottai M et al. 2017 European League Against Rheumatism/American College of Rheumatology Classification Criteria for Adult and Juvenile Idiopathic Inflammatory Myopathies and Their Major Subgroups. Arthritis. Rheumatol. 69(12), 2271–2282 (2017).
- Tanaka Y, Kuwana M, Fujii T et al. 2019 Diagnostic criteria for mixed connective tissue disease (MCTD): From the Japan research committee of the ministry of health, labor, and welfare for systemic autoimmune diseases. Mod. Rheumatol. 31(1), 29–33 (2021).
- Shiboski CH, Shiboski SC, Seror R et al. 2016 American College of Rheumatology/European League Against Rheumatism Classification Criteria for Primary Sjögren's Syndrome: A Consensus and Data-Driven Methodology Involving Three International Patient Cohorts. Arthritis. Rheumatol. 69(1), 35–45 (2017).
- Aringer M, Costenbader K, Daikh D et al. 2019 European League Against Rheumatism/American College of Rheumatology Classification Criteria for Systemic Lupus Erythematosus. Arthritis. Rheumatol. 71(9), 1400–1412 (2019).
- Ruano CA, Lucas RN, Leal CI et al. Thoracic manifestations of connective tissue diseases. Curr. Probl. Diagn. Radiol 44(1), 47–59 (2015).
- Mirfeizi Z, Farrokh D, Javanbakht A et al. Chest high resolution computed tomography findings in connective tissue diseases. Tanaffos. 12(3), 49–52 (2013).
- Salaffi F, Carotti M, Di Carlo M et al. High-resolution computed tomography of the lung in patients with rheumatoid arthritis: Prevalence of interstitial lung disease involvement and determinants of abnormalities. Medicine. 98(38), e17088 (2019).
- Goldin JG, Lynch DA, Strollo DC et al. High-resolution CT scan findings in patients with symptomatic scleroderma-related interstitial lung disease. Chest. 134(2), 358–367 (2008).
- Castelino FV, Varga J. Interstitial lung disease in connective tissue diseases: evolving concepts of pathogenesis and management. Arthritis. Res. Ther. 12(4), 213 (2010).
- Fischer A, Lee JS, Cottin V. Interstitial Lung Disease Evaluation: Detecting Connective Tissue Disease. Respiration. 90, 177–184 (2015).
- Ratanawatkul P, Oh A, Caleb Richards J et al. Performance of pulmonary artery dimensions measured on high-resolution computed tomography scan for identifying pulmonary hypertension. ERJ. Open. Research. 6, 00232–2019 (2020).
- Niklas Karolina, Niklas Arkadiusz, Mularek-Kubzdela Tatiana et al. Prevalence of pulmonary hypertension in patients with systemic sclerosis and mixed connective tissue disease. Medicine. 97(28), e11437 (2018).
- Cojocaru M, Cojocaru IM, Silosi I et al. Pulmonary manifestations of systemic autoimmune diseases. Maedica. 6(3), 224–229 (2011).
- Fischer A, Distler J. Progressive fibrosing interstitial lung disease associated with systemic autoimmune diseases. Clin. Rheumatol. 38, 2673–2681 (2019).
- Fischer A, du Bois R. Interstitial lung disease in connective tissue disorders. Lancet. 380, 689–698 (2012).
- Kobak S, Kalkan S, Kirilmaz B et al. Pulmonary Arterial Hypertension in Patients with Primary Sjögren's Syndrome. Autoimmune Dis. 2014, (2014).
- Mayberry JP, Primack SL, Müller NL. Thoracic manifestations of systemic autoimmune diseases: radiographic and high-resolution CT findings. RadioGraphics. 20(6), 1623–1635 (2013).
- Yuko Okabe, Takatoshi Aoki, Takashi Terasawa et al. Mediastinal and axillar lymphadenopathy in patients with rheumatoid arthritis: prevalence and clinical significance. Clinical. Imaging. 55, 140-143 (2019).