Research Article - Interventional Cardiology (2022) Volume 14, Issue 5
Outcomes on CLTI management with directional atherectomy with antirestenotic therapy on a single Latin-American center
- Corresponding Author:
- Patricio Huerta
Vascular Surgery Hospital Barros Luco Trudeau,
Department of Surgery,
Faculty of Medicine University of Chile,
Santiago,
Chile,
E-mail: patricio.huerta@clinicasantamaria.cl
Received date: 30-Aug-2022, Manuscript No. FMIC-22-67447; Editor assigned: 01-Sep-2022, PreQC No. FMIC-22-67447 (PQ); Reviewed date: 15-Sep-2022, QC No. FMIC-22-67447;Revised date: 22-Sep-2022, Manuscript No. FMIC-22-67447 (R);Published date: 29-Sep-2022, DOI: 10.37532/1755-5310.2022.14(5).559
Abstract
Introduction: The treatment of calcified femoropopliteal lesions is complex. Plaque debulking devices may improve results in such cases. Results have been reported, but information on real world scenarios is scarce.
Objective: To determine if Directional Atherectomy with Antirestenotic Therapy (DAART) is effective on the management of Chronic Limb-Threatening Ischemia (CLTI) on real world Latin-American patients.
Secondary objective: To evaluate quality of life.
Design: Observational, retrospective non-randomized study.
Methodology: Retrospective analysis of a single center, single arm case series. Primary outcomes overall survival and amputation-free survival. Secondary outcome, Quality of Life (QoL) measured using the EQ-5D-5L questionnaire.
Results: thirty-one patients were treated with DAART in a 6 year period with a 93.5% rate of technical success, overall survival and amputation-free survival were 87% and 88% with a mean follow-up of 57 months. Most of them reported good QoL.
Conclusion: DAART is useful on the treatment of Latin-American patients with advanced CLTI.
Keywords
Atherectomy • Chronic limb-theatening ischemia • Quality of life
Introduction
Peripheral Arterial Disease (PAD) is an important cause of lower extremity pain and amputation and affects over 200 million adults worldwide [1]. Endovascular therapy is currently the main treatment option, including traditional Plain Balloon Angioplasty (POBA) with or without stenting. However, the permeability for POBA in femoropopliteal lesions can be as low as a 45% of primary patency after 3 years [2]. Use of stents has not consistently led to improvement in results either [3]. Nevertheless, atherectomy devices combined with angioplasty (known as directed atherectomy with antirestenotic therapy, DAART) have emerged as an option by debulking atheroesclerotic plaque, providing success in terms of patency [4]. This technique’s results have been previously reported, but there are few outcomes studies on real world scenarios regarding Latin-American patients.
We report our experience in the treatment of femoropopliteal atheroesclerotic lesions using directional atherectomy in a period of almost 6 years and analyze the procedure’s outcomes on limb preserving and quality of life. Our main objective was to determine whether DAART is an effective technique for the management of advanced CLTI on real world Latin-American patients.
Materials and Methods
Single center, single arm, retrospective non-randomized study on a major public hospital, serving medium and low income patients in Latin-America. The studied period starts with the first femoropopliteal DAART (FP DAART) in our center in October 2014 to March 2020.
At our institution, every patient affected by Critical Limb-Threatening Ischemia (CLTI) on advanced stages (Rutherford 4 to 6) undergo an arteriography and are then evaluated by a vascular surgery committee. The most appropriate management is offered, generally choosing FP DAART for elderly patients with heavily calcified lesions (Table 1).
| Inclusion criteria | Exclusion criteria |
|---|---|
| Rutherford classification 4-5 | Contraindication to antiplatelet therapy, anticoagulants, thrombolytic drugs, or any other drug anticipated to be used |
| Evidence of 70% stenosis or occlusion in the superficial femoral or popliteal confirmed by angiography | |
| Hypersensitivity to radiocontrast that cannot be adequately pre-treated | |
| TASC 2 A, B, C | Uncontrollable hypercoagulable condition or refuses blood transfusion |
| Identifiable distal target vessel, which upon completion of the intervention, is anticipated to provide reconstitution of blood flow to the foot | Life expectancy <12 months |
| Any comorbid condition(s) that precludes safe percutaneous intervention | |
| Reference vessel diameter is 4 mm–6 mm | Previous bypass affecting the target limb |
| Previous amputation above the metatarsal line on the target limb |
Table 1: Inclusion and Exclusion criteria for DAART at our center.
First, we conducted a revision of all cases and their clinical files, searching for demographic and clinical data, their last medical evaluation, and other basic information. We then re-evaluated the anatomy of the lesion (TASC II) and procedure details. Lastly, we updated the clinical evaluation by applying a telephonic questionnaire which included different aspects from the primary and secondary outcomes. All patients, female and male, with atherectomy procedures on the indicated period were included. No exclusion criteria was initially applied, though failed procedures were excluded from further analysis. Missing data not found on clinical files were mostly acquired directly from patients on their telephonic evaluation.
Our main objective was to determine whether DAART is an effective technique for the management of advanced CLTI on real world Latin-American patients. Briefly, the procedure is performed with the TurboHawk and HawkOne directional atherectomy system (Medtronic), with a filter for distal embolization prevention, according to a previously described technique by Zeller, et al. [5]. After atherectomy, patients either undergo Plain Balloon Angioplasty (POB) or Drug Coated Balloon angioplasty (DCB).
The primary outcomes, overall survival and amputation-free survival, were used to evaluate our main objective. Secondly, we focused on Quality of Life (QoL), which was measured using a previously validated questionnaire, EQ-5D-5L (EuroQol Research Foundation). The EQ-5D-5L has been validated for measuring QoL on populations all over the world and it focuses on five major items (mobility, self-care, performance of usual activities, pain/discomfort, anxiety/depression). It also assesses self-perception of global health with an analogue scale ranging from 0 to 100%. A specially adapted version for telephonic evaluation on Chilean patients was used [6]. EuroQol Research Foundation reviewed and authorized the utilization of this instrument. Other variables such as technical success (defined as <50% residual stenosis), adherence to pharmacologic treatment and ability to walk were also registered. The local institutional ethics committee approved this investigation.
Descriptive analysis was performed, evaluating demographic and clinical characteristics, including prevalence of cardiovascular risk factors, Rutherford stage, and TASC II classification. Procedure details (treated artery, use of POBA, DCB, stent, outflow arteries, residual stenosis, intraoperative complications) were also analyzed. Results were evaluated focused on overall survival, amputation-free survival, ability to walk, adherence to medical treatment and QoL. The safety profile for atherectomy and DCBA was assessed by evaluating the 30-day frequency of major amputation and all-cause mortality. Results were expressed as mean and Standard Deviation (SD) for continuous variables and values and percentage for categorical variables.
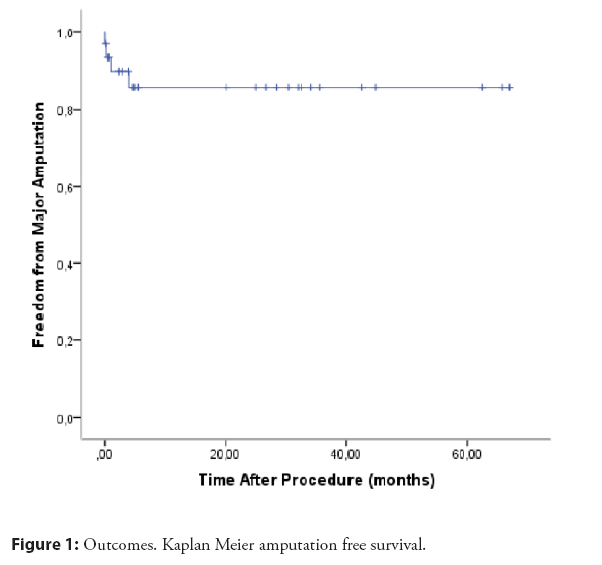
Amputation-free survival at 1, 6, 12 and 36 months was calculated using Kaplan–Meier test. p value0.05 was considered statistically significant. Data was analyzed using ISSP. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. P Huerta has previously worked as an advisor for Medtronic.
Results
FP DAART was offered to thirty-one patients in the studied period. There were two failed procedures (93.5% technical success). The resulting twenty-nine cases were predominantly males, with a mean age of 70 years, and with a heavy burden of cardiovascular risk factors. Both hypertension and diabetes were common amongst the group (93.5% and 67.7% respectively), probably reflecting PAD’s current world profile (Table 2). Advanced CLTI was the indication for the vast majority (>90% Rutherford 4 or 5). 18 out of 29 were able to answer the telephonic interview, 7 out of 29 could not be contacted. 4 patients were dead at the time of final follow up.
| Age | 70,1 (Years, Median) |
|---|---|
| Gender | |
| Male n (%) | 20 (64,5) |
| Female n (%) | 11 (35,4) |
| Risk Factors | |
| Hypertension, n (%) | 29 (93.5) |
| Diabetes, n (%) | 21 (67.7) |
| Smoking, n (%) | |
| Ex-smoker | 11 (35.4) |
| Current smoker | 14 (45.1) |
| Coronary disease | 6 (19.3) |
| CKD | 4 (12.9) |
| Clinical Presentation | |
| Rutherford 3 | 2 (6,5) |
| Rutherford 4 | 10 (32.2) |
| Rutherford 5 | 19 (61.2) |
Note: CKD: Chronic Kidney Disease defines as GFR<60 ml/min.
Table 2: Clinical and demographic characteristics of the DAART patients at our center.
Primary outcome of overall survival and amputation-free survival were 87% and 88% with a mean follow-up of 57 months. There were 3 major ipsilateral amputations, and only one case was done before 30 days from the procedure (Figure 1). At the end of follow up there were no cases of clinically driven TLR and there were 4 deaths, all of them non-related to PAD and several months or years after FP DAART.
All of the cases were done by a vascular surgeon as previously detailed, using the Medtronic direct atherectomy device, with a distal filter and post atherectomy DCB angioplasty for most of them. Regarding the procedure itself, FP DAART was conducted on a variety of different vascular lesions, from TASC II A to D, with no significant residual stenosis (Table 3). Notably, although Superficial Femoral Artery (SFA) and Popliteal Artery (PA) were the main target, many cases needed below the knee concomitant procedures (32.2% outflow BTK angioplasties). Despite good general results, complications did occur, being dissection of the treated vessel the most frequent (6 cases, 19.3%). 3 out of 6 were on the SFA and therefore stented.
| Procedural characteristics | N (%) |
|---|---|
| TASC II for femoropopliteal disease | |
| A | 5 (16.1) |
| B | 10 (32.2) |
| C | 9 (29.0) |
| D | 7 (22.5) |
| Target vessels | |
| SFA | 20 (64.5) |
| SFA+PA | 10 (32.2) |
| PA | 1 (3.2) |
| Successful revascularization | |
| Yes | 29 (93.5) |
| No | 2 (6.4) |
| Runoff vessels | |
| 0 | 0 |
| 1 | 10 (32.2) |
| 2 | 12 (38.7) |
| 3 | 9 (29.0) |
| Access | |
| Femoral crossover access | 28 (96.5) |
| Femoral Ipsilateral | 1 (3.5) |
| Concomitant endovascular procedure | |
| None | 20 (64.5) |
| Inflow | 1 (3.2) |
| Outflow | 10 (32.2) |
| Complications | |
| SFA rupture | 1 (3.2) |
| Dissection | 6 (19.3) |
| Occlusion | 2 (6.4) |
| Access site complications | 0 |
Note: SFA: Superficial Femoral Artery; PA: Popliteal Artery.
Table 3: Procedures were considered successful whenever on line perfusion to the foot was achieved. Concomitant procedures were needed when in presence of other critical lesions.
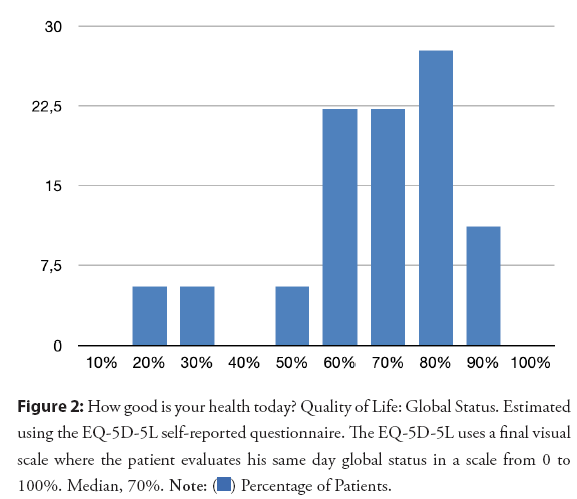
QoL was evaluated using the EQ-5D-5L questionnaire. A large proportion of patients reported slight or no problems at all for the five measured areas, including mobility (Figure 2 and Table 4). Self-perception of global health was 60% or more for the majority of the 18 patients who answered the telephonic evaluation. Ability to walk was specially evaluated. Only 4 patients reported suffering claudication on their last medical examination. The impact on QoL for those patients is relatively unknown, since 2 of them were unreachable for answering the EQ-5D-5L questionnaire.
Figure 2: How good is your health today? Quality of Life: Global Status. Estimated using the EQ-5D-5L self-reported questionnaire. The EQ-5D-5L uses a final visual scale where the patient evaluates his same day global status in a scale from 0 to 100%. Median, 70%.
| Quality of life | Mobility N (%) | Self-care N (%) | Usual Activities N (%) | Pain/Discomfort N (%) | Anxiety/Depression N (%) |
|---|---|---|---|---|---|
| Level 1 (Not problems) | 8 (44.4%) | 13 (72.2%) | 11 (61.1%) | 9 (50%) | 10 (55.5%) |
| Level 2 (Sligt problems) | 2 (11.1%) | 2 (11.1%) | 2 (11.1%) | 5 (27.7%) | 5 (27.7%) |
| Level 3 (Moderate problems) | 5 (27.7%) | 1 (5.5%) | 4 (22.2%) | 2 (11.1%) | 3 (16.8%) |
| Level 4 (Severe problems) | 1 (5.5 %) | 2 (11.1%) | 1 (5.5%) | 2 (11.1%) | 0 |
| Level 5 (Extreme problems/unable to do) | 2 (11.1%) | 0 | 0 | 0 | 0 |
| TOTAL | 18 (100%) | 18 (100%) | 18 (100%) | 18 (100%) | 18 (100%) |
Table 4: Estimated using the EQ-5D-5L self-reported questionnaire. Each item assess one aspect of the patient’s current health status by grading their capacity to complete the task or condition. Most of them reported minor difficulties.
Finally, not all patients were receiving a complete secondary prophylaxis for PAD (statins and antiplatelets) at the time of final follow up. 77% were still on statins, and 55% on antiplatelets.
Discussion
Our main objective was successfully met, as both primary outcome of overall survival and amputation-free survival were similar to previously published experiences [4,7]. Follow up at our center is mainly clinical, and relies on imaging and eventually redo when symptoms and ischemia demand so. Thus, patency is not formally evaluated on this report. Being this a symptom and clinically driven study, QoL was a relevant aspect. The application of the EQ-5D-5L questionnaire gave us most appealing results, revealing most of the patients had a fair QoL and considered their health status positively. As stated, many of them were even able to walk with little or no help.
Currently, endovascular intervention is the first-line therapy for femoropopliteal territory, but continues to be a challenge particularly in long, highly calcified lesions. Debulking atherectomy may allow for a more uniform angioplasty result at lower pressures with consequently less vessel barotrauma and improved luminal gain, thereby decreasing the risk of recoil and dissection that may require permanent metal stenting [5,7,8]. Also, exposing smooth muscle cells in the arterial wall may improve drug uptake from DCB [9]. Although atherectomies have been criticized (as in the most recent European guidelines) [1], one of the most appealable results may be the femoropopliteal in line revascularization avoiding the use of a stent in the Hunter region. Another point of interest when discussing DAART is the lack of evidence for CLTI patients, since the vast majority of current publications are mainly based on claudicants.
In recent years, paclitaxel coated balloon angioplasty has shown superior anti restenotic results and has been widely used in femoropopliteal arterial disease. Katsanos, et al. reported that DCB angioplasty could reduce by more than half the rates of restenosis and TLR, regardless of stent placement [10]. We, however, did not use DCB in 8 cases because it was initially not available at our center. These 8 cases underwent POBA, with mixed final results: 3 major ipsilateral amputations and 3 claudicants.
We used stents for persistent post angioplasty flow limiting dissection after DAART in 3 cases, all of them in the SFA. The PA is subject to high biomechanical stress due to repetitive flexion and extension thus, the fear of stent fractures and restenosis has led to uncertainties in how stents should be used for optimal treatment of PA lesions. Luckily, none of our cases that compromised the PA required stenting.
This report has several limitations. Firstly, is a retrospective non-randomized review without a comparative group. Secondly, only 18 patients were contacted for a telephonic evaluation, the rest of them were unreachable. Nevertheless, there are few cases of true loss to follow-up, since the rest of them have had recent clinical evaluation registered on their file. It is relevant to mention as well, that the Chilean public health system intends to treat patients in their local hospital, so there’s little chance for some of the cases to undergo an amputation unknown for us. We believe a future investigation should better address the problem of improving follow-up and clinical evaluations in the Chilean population.
To our knowledge, this is one of the first reports on real world scenarios regarding Latin-American patients. The observed results demonstrate both the feasibility and clinical appealing outcomes of DAART on Chilean patients, suggesting it may be a valid option on highly calcified lesions with a variety of TASC II types of occlusions and critical stenosis.
Conclusion
DAART, although, can’t solely respond to advanced CLTI, since multi-level vascular compromise with synchronous below-the-knee occlusions is common. DAART may be a useful therapy tool for real world advanced CLTI, with multi-level stenosis and occlusions, especially when heavily calcified. These are complex cases that need thorough preparation and careful selection, ideally by a dedicated group. Follow up remains a challenge and an area for improvement.
References
- Conte MS, Bradbury AW, Kolh P, et al. Global vascular guidelines on the management of chronic limb-threatening ischemia. Eur J Vasc Endovasc Surg. 58(1S): S1-S109 (2019).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Laird JA, Schneider PA, Jaff MR, et al. Long term clinical effectiveness of a drug-coated balloon for the treatment of a femoropopliteal lesions. Circ Cardiovasc Interv. 12(6): e007702 (2019).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Chowdhury MM, McLain AD, Twine CP. Angioplasty versus bare metal stenting for superficial femoral artery lesions. Cochrane Database Syst Rev. 2014(6): CD006767 (2014).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Zhen Y, Chang Z, Wang C, et al. Directional atherectomy with antirestenotic therapy for femoropopliteal artery disease: A systematic review and meta-analysis. J Vasc Interv Radiol. 30: 1586-1592 (2019).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Zeller T, Langhoff R, Rocha-Singh K, et al. Directional atherectomy followed by a paclitaxel-coated balloon to inhibit restenosis and maintain vessel patency twelve-month results of the DEFINITIVE AR study. Circ Cardiovasc Interv. 10: e004848 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Global vascular guidelines on the management of chronic limb-threatening ischemia
- Gupta R, Malgor R, Siada S, et al. Critical appraisal of the contemporary use of atherectomy to treat femoral-popliteal atherosclerotic disease. J Vasc Surg. 75(2): 697-708.e9 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Shammas NW, Coiner D, Shammas GA, et al. Percutaneous lower-extremity arterial interventions with primary balloon angioplasty vs. Silverhawk atherectomy and adjunctive balloon angioplasty: Randomized trial. J Vasc Interv Radiol. 22(9): 1223-1228 (2011).
[CrossRef] [Google Scholar] [PubMed]
- Tzafriri A, Gaarcia-Polite F, Zani B, et al. Calcified plaque modification alters local drug delivery in the treatment of peripheral atherosclerosis. J Control Release. 264: 203-210 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Katsanos K, Spiliopoulos S, Paraskevopoulos I, et al. Systematic review and meta-analysis of randomized controlled trials of paclitaxel-coated balloon angioplasty in the femoropopliteal arteries: Role of paclitaxel dose and bioavailability. Endovasc Ther. 23(2): 356-70 (2016).
[CrossRef] [Google Scholar] [PubMed]