Research Article - Interventional Cardiology (2021) Volume 13, Issue 1
Native arteriovenous fistula, surgical outcomes and primary failure in Taiz Yemen: A prospective study
- Corresponding Author:
- Ismail S. Al-Shameri
Department of General Surgery,
Authority of Althawra Hospital,
Taiz University Factuality of medicine,
Taiz,
Yemen,
Email: Ismailsamer17@gmail.com
Received date: December 16, 2020 Accepted date: January 11, 2021 Published date: January 18, 2021
Abstract
Background: Haemodialysis (HD) is a lifesaving and life-sustaining management for patients with End Stage Renal Disease (ESRD). There are number of vascular access options including native Arteriovenous Fistulas (AVF), artificial arteriovenous grafts (AVG) and dialysis catheters. AVF is generally recognized as the cornerstone of long-term dialysis treatment due to its superior patency and lower complication rates. The present study investigates surgical outcomes and complications post AVF creation by Parachute Vascular Anastomosis Technique (PVAT) in Taiz, Yemen.
Materials and methods: This prospective study of 196 patients who underwent a native AVF created by parachute anastomosis technique from October 2017 to September 2019 in Authority of Althawra hospital in Taiz- Yemen. Detailed physical examination (inflow arterial pulses and outflow veins) was performed. Patients with abnormal physical examination were sending for preoperative sonography mapping. Non-dominant upper extremity was used as priority site for vascular access creation. AVF was performed under local anesthesia. Patients were followed up in outpatient clinic for six months.
Result: Total of 231 AVF in 196 patients, 121 (61.7%) were male and 75 (38.3%) were female. Mean age was 48.5 ± 16.8 (range 9–85) years. A majority of AVF were brachiocephalic 112 (48.5%) while the remaining was radiocephalic 74 (32%) and brachiobasilic 43 (18.6%). Most of patients had left non-dominant upper arm AVF. The immediate patency rate (palpable thrill intra operative) was 218(94.4%) with an overall functional rate (successful use of the AVF for six consecutive sessions of HD) of 198 (85.7%). The primary failure rate (within 3 months) was 33 (14.3%). Six months primary patency was 186 (80%). During study period, the most common complication of AVF was thrombosis 30 (13%).
Conclusion: Based in our result and literature review we could report excellent functional rate (85.7%) of AVF created by parachute vascular anastomosis technique. For that, parachute technique may be suggested as one of optimal selection to create AVF especially in elderly, diabetic patients.
Keywords
Haemodialysis access; Arteriovenous fistula; Parachute anastomosis technique; Primary failure
Introduction
Haemodialysis (HD) is a lifesaving and life-sustaining management for patients with ESRD, It is the most prevalent dialysis treatment modality and is identical to transplantation in terms of patient numbers, the latter modality considered to be is the preferred treatment for ESRD [1,2]. The optimal delivery of HD has been shown to result in improved patient outcomes. The success of HD mainly depends on the establishment of vascular access that is safe and reliable with minimal complication; which still a big challenge for vascular surgery as most hospitalizations, morbidity and mortality in those patients are due to impairment and complications of vascular access [3-5].
There are number of vascular access options including native arteriovenous fistulas (AVF), artificial arteriovenous grafts (AVG) and dialysis catheters [6]. AVF is generally recognized as the cornerstone of long-term dialysis treatment due to its superior patency and lower complication rates [7]. Over last 50 years, AVF still represents the favorite vascular access to provide HD in terms of access patency [8], patient mortality [9,10], morbidity [11] and health cost [12] compared to other types. Kidney Disease Outcomes and Quality Initiative (KDOQI) guidelines recommend that 40% incident and 50% prevalent HD patients should undergo dialysis with an AVF [13].
AVF is created by a surgical anastomosis between native artery and vein, to allow access to vascular system for HD [14,15]. The preferred type of AVF is radiocephalic fistula which was the first AVF designed in 1966 by Brescia [16]. However, this access often fails to mature in the elderly patient with underlying vascular disease, particularly in diabetics [17]. Second preferred type is brachiocephalic fistula [18,19]. This type of fistula is being placed with increased frequency because of the high failure rate of radiocephalic fistula, followed by a brachiobasilic transposition fistula [20].
Failure of an AVF not only interrupts a functional access but also reduces the number of sites at which another access can be made. In addition, subjecting the patients to interventional procedures is required to salvage the failing AVFs. Therefore, it is important to evaluate risk factor that effect AVF patency and identify failure rate and post- operative complications that may occur after AVF placement [5].
To date, no publication has been reported on creating and outcomes of AVF in our city. Thus, Present study was conducted to identify functional, primary failure rate and complication of native AVF creation by (PVAT) in Taiz, Yemen from October 2017 to September 2019.
Patients and Methods
This prospectively study was conducted at Department of vascular surgery, Authority of Althawra Hospital in Taiz- Yemen, from 1st October 2017 to 30th September 2019. All patients with ESRD, who refer for creation AVF were include in this study. A total of 196 patients underwent 231 AVF operations were enrolled in the study. Details Demographic, Clinical, and preoperative dialysis variables were obtained for every patient. Allen’s test and arterial pulses (i.e. axillary, brachial, radial, and ulnar) were examined. Patients with visible veins on the clinical examination were directly scheduled for AVF creation while patients with non-visible veins were undergo vein mapping by ultrasonography (US) before being scheduled for surgery [21]. The distal part of the non-dominant extremity was selected as priority anatomical site, whenever possible [22]. All operations were created by the single Resident surgeon supervise by senior cardiovascular consultant.
Outcome parameter
Maturation (Functional) of AVF was be defined as the successful use of the AVF for six consecutive sessions of HD. This definition for the evaluation of AVF maturation has been validated in the literature in several previous studies [23-25]. Primary failure define as an AVF that has never been usable for dialysis or that fails within three months of use [26,27]. In our study, primary patency of AVF at immediate, 30 and 90 days, and at 6 months had been measured.
Procedure detail
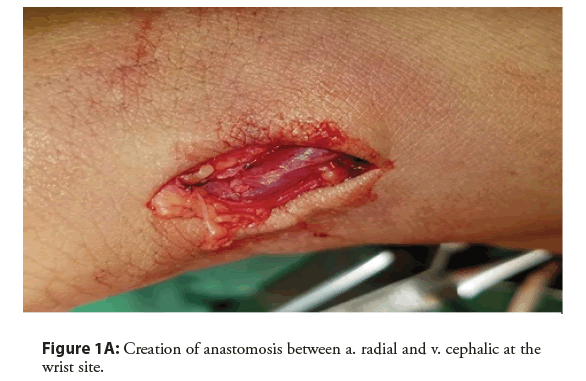
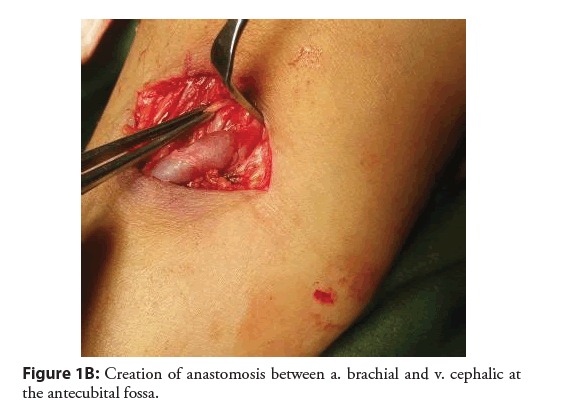
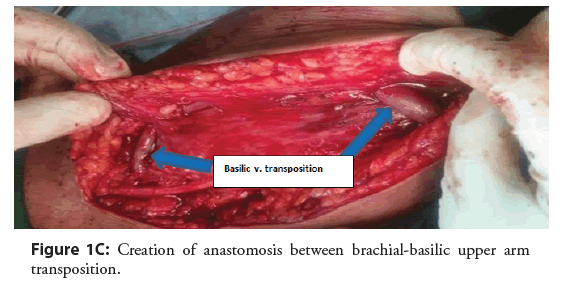
AVF was routinely created under local anesthesia (2% xylocaine\3 mg\kg) or regional anesthesia and sedation for brachiobasilic transposition anesthesia. Antibiotic did not give before the procedure. After cleansing and sterilizing the site of operation. A longitudinal incision (3 cm) made for the wrist or forearm region and a horizontal incision for the elbow antecubital region, the artery and vein are dissected and freed. Exposure of the vein was performed in a way to prevent its angulation and bending. At this stage, the distal part of the vein ligated. Heparinized isotonic saline pushed by syringe 20 cc with a feeding infant tube 6 fh for the proximal part of the vein then occluded via bulldog to block retrograde flow. After confirming vein suitability, the suitable artery suspended and arterial flow controlled with bulldog, small arterial branches were preserved. A longitudinal arteriotomy about 5-8 mm was performed in the forearm while a 4-6 mm performed in arm with surgical blade number 11 and Pott’s scissors. The side underwent arteriotomy was suspended from both sides and an adequate view was achieved. End-to-side anastomosis by parachute vascular anastomosis techniques using 6/0 or 7/0 propylene sutures [28-31]. Anastomoses started from the opposite side (3 mm ahead of the middle of the posterior walls) of the artery. Suturing was continuous along the posterior vessel wall until extend beyond the arterial angle of anastomosis. At this time, both ends of the propylene suture were wet with heparinized saline and gentle pulling was applied, in a direction perpendicular to the axis of the both vessel walls to approximate “parachute” it together. Then the anterior vessel was suturing together with a continuation fashion until the anastomosis is finished at the same point at the beginning. After the last suture, both ends of the suture material were pulling gently, but putting the knot was delayed until the unclamping of the radial or brachial artery. This permits the anastomosis site to become expanded to its widest size and prevents a purse-string effect at the anastomosis site. Thrill over fistula was confirmed, followed by adequate hemostasis before closure. The wound was closed in one layer using 3/0 absorbable mattress sutures for the skin with gentle antiseptic dressing was made.
Follow-up schedule
All patient discharges on operation day with oral antibiotics and analgesics for three days. Patients were instructed to start hand exercise on the second postoperative day with ball. Skin stitches ware removed on the 10th post- operative day. The follow up performed on an outpatient basis, at 7th and 14th day then at 4 and 6 weeks post- operative, where fistula was released to puncture for HD. Periodic follow up was performed for at least 6 months (average 6 to 24 months). In follow up visit, all patients were be evaluated for the presence or absence thrill or complications i.e. seroma, hematoma, infection, bleeding, thrombosis, aneurysms, steal syndrome and venous hypertension.
Study analysis
Data collection and analysis conducted using SPSS (IBM SPSS Statistics 24.0). Initially, descriptive analysis of outcome and variables predominantly was analyzed as frequencies, tables and percentages for categorical variable and mean and SD for continuous variable. The association between variable and outcome or complication were analyzed by the Chi-square (x2) or fisher test for the categorical variable and unpaired Student’s t-test for the continuous variable with the corresponding 95% Confidence Interval (CI). P-values ≤ 0.05 were considered statistically significant.
Results
A total of 231 AVF procedures in 196 patients, 121(61.7%) were male and 77(38.3%) were female with male to female ratio of (1.5:1). The mean age was 48.5 ± 16.8 (range 9-85) years, majority (48.5%) of the patients belonged to age group 41–63 years; followed by (25.1%) patients belonging to 19–40 years of age.
Table 1 show that, functional rate of the fistula was highest 42/47 (89%) in the age group equal and more than 64 years followed by 97/112 (86.6%) in the age grouped 41–63 years. Function rates in other age groups were 48/58 (82.6%) in 19–40 years and 11/14 (78.6%) in <18 years. The function rates in male were 121/140 (86.4%) and 77/91 (84.6%) in female subjects, while the failure rates of AVF were 19/121 (13.6%) and 14/91 (15.4%) in male and female subjects, respectively. However, this difference was statistically insignificant (p=0.7).
| Function, µ (%) | Failure, µ (% | Total, µ (%) | |
|---|---|---|---|
| Age groups | |||
| <18 | 11(78.6) | 3(21.4) | 14(100) |
| 19-40 | 48(82.6) | 10(17.2) | 58(100) |
| 41-63 | 97(86.6) | 15(13.4) | 112(100) |
| 64+ | 42(89.3) | 5(10.7) | 47 (100) |
| Gender | |||
| Male | 121(86.4) | 19(13.6) | 140(100) |
| Female | 77(84.6) | 14(15.4) | 91(100) |
| Total | 198(85.7) | 33(14.3) | 231(100) |
Table 1: Age and gender distribution of patients along with the function rate of AVF (n=231).
Medical history of disease (Table 2) included hypertension in 146 (74%), diabetes in 53 (27%), CHD in 31 (15.8%) and PAD in 19 (9.7%) patients. In addition, patients with history of smoking and chewing Qat were 41 (20.9%), 15 (7.7%) respectively.
| History of Disease | Frequency | Percentage (%) |
|---|---|---|
| HTN | 146 | 74.50% |
| Diabetes | 53 | 27% |
| IHD | 12 | 6.10% |
| CHF | 31 | 15.80% |
| PAD | 19 | 9.70% |
| CVA | 12 | 6.10% |
| Smoking | 41 | 20.90% |
| Chewing Qat | 15 | 7.70% |
Table 2: History of disease and risk for patients undergoing hemodialysis.
Regarding the time of dialysis initiation majority of patients 180 (91.8%), were be referred late (after initiation or within 1 month). As in our finding, 144 (73.5%) patients had non-tunneled catheter at time of AVF creation. Furthermore, 175 (89.3%) patients have already had other forms of vascular access before AVF creation; one or more non-tunneled catheters were be used. Table 3 shows other pre-dialysis history of patients before AVF creation.
| Dialysis history baseline items | Frequency (%) |
|---|---|
| Non-tunneled Dialysis catheters used/Number | |
| NO | 21(10.7) |
| YES (Use one) | 90(45.9) |
| Use tow | 44(22.4) |
| Use three | 19(9.7) |
| Use four or more | 22(11.2) |
| Current catheter at time of operation | |
| NO | 52(26.5) |
| YES | 144(73.5) |
| Pervious AVF | |
| NO | 123(62.8) |
| YES | 73(37.2) |
| Previous procedures same limb | |
| No prior procedure | 139(70.9) |
| One prior procedure | 46(23.5) |
| Two prior procedures | 11(5.6) |
| Dialysis at time of surgery | |
| NO | 32(16.3) |
| YES | 164(83.7) |
Table 3: Pervious dialysis history baseline character before AVF creation.
In this study, all the patients had native AVFs with end-toside anastomotic (parachute) technique. No grafts were used. Majority of patients 183 (79.2%) had left non-dominant arm. The most common AVF was the brachiocephalic 112 (48.5%), then radiocephalic 74 (32%), Brachiobasilic 43 (18.6%), one ulniobasalic AVF and on brachiobrachial AVF (Table 4). The first time cannulation were achieved after four, four to six and more than six weeks in 43 (18.6%), 134 (58%) and 28 (12.1%) patients respectively.
| Baseline characteristics | Patient, µ (%) | Failure, µ (%) | Total, µ (%) | p-value |
|---|---|---|---|---|
| Access Side | ||||
| Left | 157(68) | 26(11.3) | 183(79.3) | 0.9 |
| Right | 41(17.7) | 7(3) | 48(20.8) | |
| Fistula Configuration | ||||
| Radiocephalic AVF | 55(23.8) | 19(8.3) | 74(32) | 0.016 |
| Brachiocephalic AVF | 99(42.9) | 13(5.6) | 112(48.5) | |
| Brachiobasilic AVF | 42(18.2) | 1(0.4) | 43(18.6) | |
| Ulniobasalic AVF | 1(0.4) | 0 | 1(0.4) | |
| Brachiobrachial AVF | 1(0.4) | 0 | 1(0.4) | |
| TOTAL | 198(85.7) | 33(14.3) | 231(100) | |
| Intraoperative Thrill | ||||
| YES | 189(81.8) | 18(7.8) | 207(89.6) | 0 |
| NO | 9(3.9) | 15(6.6) | 24(10.5) | |
| TOTAL | 198(85.7) | 33(14.3) | 231(100) | |
| When Using Post Operation (weeks) | ||||
| < 4 wks | 43(18.6) | |||
| 4 - 6 wks | 134(58) | |||
| > 6 wks | 28(12.1) | |||
Table 4: AVF procedure (intra-operation) characteristics (n=231).
On assessing the patency of 231 fistulas, (n=198, 85.7%) fistulas were patent. Among this 198 patent fistulas, brachiocephalic fistula was 43%, followed by radiocephalic (23.8%) and Brachiobasilic fistulas (18.2%). We found that, the proximal fistula site (arm) and the present of good thrill intraoperative of AVF were significantly associated with a more favorable outcome of AVF Primary patency (P=0.016), (P=0.000) respectively. In our study, the primary patency rate was 203 (87.9%) at 1st month, 193(83.9%) at 3 months and 184(80.0%) at 6 months. Thirty- three (14.3%) fistulae failed within the first 3 months. Failing AVFs were managed by new fistula in our series. The most common complication was thrombosis 30 (13%) followed by noninfectious fluid collections (hematoma/seroma/lymphocele) 24 (10.4%), wound infection 17 (7.4%), bleeding 9 (3.9%) and Postoperative edema 10(4.3%). Aneurysm, venous hypertension and steal syndrome were found in 9 (3.9%), 4 (1.7%) and 3 (1.3%) cases respectively (Table 5).
| Complication | Frequency | % |
|---|---|---|
| Thrombosis | 30 | 13% |
| Noninfectious fluid collections (hematoma/seroma/lymphocele) | 24 | 10.40% |
| Infectious | 17 | 7.40% |
| Limp edema | 10 | 4.30% |
| Bleeding | 9 | 3.90% |
| Infection and burst fistulae | 7 | 3% |
| Aneurysmal degeneration | 9 | 3.90% |
| Venous hypertension | 4 | 1.70% |
| Steal syndrome | 3 | 1.30% |
| Ischemic naturopathy | 3 | 1.30% |
Table 5: Post-operative Complications of AVF.
Discussion
Effective formation and sufficient function of AVF in patients with ESRD need a multidisciplinary approach in determining and resolving the leading causes for primary failure. The process of AVF maturation is multifaceted and leftovers poorly understood, in spite of numerous studies describing the pathophysiology of the procedure and biomechanical issues associated with maturation. The Intimal Hyperplasia (IH) has been recognized as the highest pathohistological change, which arises in the blood vessels and was related with the primary failure of AVF [32]. However, the creation of AVF is the first step for the patients who need an efficient durable vascular access for HD.
The rate of primary failure of AV fistulas is highly variable and has ranged from 47 to 60 percent in randomized trials, but the published rates depend heavily on the definition of failure [33,34]. Mc Lafferty et al., described adequate AVF maturation of 82% and a primary failure rate of 18% in patients with AVF [35]. Monroy-Cuadros et al. noticed AVF failure in 81 patients out of 831 studied cases (rate=10%) [36], and Sari et al. reported 15.3% for incidence rates of primary AVF failure and never using AVF after operation [37].
Unsurprisingly, in a meta-analysis on 46 articles (7,393 AVFs), the generally risk of primary failure was 23%, but it enlarged in the elderly to 37% [38,39], and primary fistula patency was established in 26 of 43 patients (60%), meaning that AVF failure rate was equal to 40% [40]. In the previous years, a worse condition has been reported showing that from 101 fistulas only 47 fistulas (46.5%) established sufficiently to be used for HD, on behalf of the AVF failure rate of 53.5% [41]. Gjorgjievski et al., reported sufficient functioning was accomplished in 83.71%, and primary failure noticed in 16.29% of the created fistulae [42].
We define primary failure as an arteriovenous (AV) fistula that has never been usable for HD or that fails within three months of use [26,27]. In our study, adequate maturation was achieved in 85.7%, and primary failure occurred in 14.3% of the created fistulae. As discuses above, the rate of primary AVF failure in this study was similar or better compared to the average reported AVF failure rates in other parts of the world (Table 6).
| Reference | Publishing Year | Country/region | No. Patients/procedure | AVF Failure rate |
|---|---|---|---|---|
| Miller, et al. | 1999 | Birmingham, US | 101 | 53.50% |
| Tordoir, et al. | 2003 | Netherlands | 43 | 40% |
| Mc Lafferty, et al. | 2007 | Southern Illinois University, SIU | 113 | 18% |
| Monroy-Cuadros, et al. | 2010 | Canada | 831 | 10% |
| MacRae, et al.; Al-Jaishi, et al. | 2014 | London/UK | 7393 | 23-37% |
| Dekhaiya, et al. | 2016 | India | 150 | 23.33% |
| Sari, et al. | 2016 | Turkey | 36 | 15.30% |
| Gjorgjievski, et al. | 2019 | Macedonia | 178 | 16.29% |
| Our Study | 2020 | Yemen | 231 | 14.30% |
Table 6: Post-operative Complications of AVF.
The mean age of patients with ESRD undergoing AVF in our series was 48.3 years which was similar or close to other studies [43,44]. However, the mean age in developed countries was one or two decades older [25,38,42]. The influence of age on the patency of AVF is still controversial. Al-Jaishi et al., [38] and Gibson et al., [45] found that age had no effect on primary patency. The results in our study confirm that patient age is not a factor in the success of procedure and AVF should not be suspended from patients based on age similar observation was also found by other study [43,44,46,47].
We did not find a significant effect of gender on AVF patency in our study. In a literature review of 2012, Smith et al., 48 also found the same result. On the other hand, there’re studies found significant differences in outcomes of AV fistula creation when comparing males and females [48-50]. In one study, females were at greater risk for failure of the AV fistula to mature compared with the males in spite of preoperative vascular mapping (hazard ratio 2.42, 95% CI 1.32-4.45) [51]. The reasons for these differences are not clear. It has been suggested that females have smaller vessels [45,52].
As has been alluded in many studies delayed presentation of ESRD patients to the hospital in developing countries and late referral for AVF creation have provided the need for temporary vascular access to have HD [53-55]. Early referral strategy significantly decrease morbidity [56], mortality [57,58], dialysis catheter insertion [59], urgent HD [60] and length of hospital stay [61]. In our study, majority of patients 180(91.8%) were referred late. We found that nine out of 10 patients in our series had a previous central venous access for emergency HD before referral for AVF creation. All this, adversely affect the available of suitable peripheral and central venous. So that, more proximal vein was used for AVF creation. This issues recognized clearly in our study, as about fifty present 105(46%) of our patients had their first native AVF creation in proximal upper limb veins. For that, numerous studies recommended the need for early referral and education for predialysis patients to prevent the use of peripheral (upper limb vein preservation strategy) and central venous catheters and to avoid their subsequent complications [35,62].
The left upper limb being the nondominant limb in most of the patients were used for the creation of AVF in the majority (79.3%) of our patients. The preference for the nondominant limb is as a result of the need to carry out minimal work or activities with the limb to preserve the delicate AVF, especially in the first two weeks following surgery. Similar preference for the non-dominant upper limb is also practiced in other study [43]. Brachiocephalic (48.5%) was the most common type AVF followed by radiocephalic type (32%). Shan et al., [63] and Mc Lafferty et al., [35] found similar observation. In other hand many studies found radiocephalic most common [42,25].
AV fistula takes a number of weeks to mature, on average perhaps 4–6 weeks [64,65].
In our study, the first time cannulation were achieved after four, four to six and more than six weeks postoperative in 43(18.6%), 134(58%) and 28(12.1%) patients respectively. Surgical techniques are important factor that effect AVF patency [66]. Despite being variable in clinical applications, the end-to-side anastomosis technique is applied with 4 quadrant, 2-quadrant, oval, diamondshaped or parachute techniques. There are reports of the common use of the standard parachute end-to-side anastomosis technique not only in Cardio vascular surgery, but also in many surgical fields including hepatobiliary surgery and gastrointestinal surgery [29-31,67]. The parachute technique may be an optimal selection in distal AVF where vascular structures are of lesser caliber, especially in DM, elderly patients, and diffuse vessel calcification [29,30,68,69]. In our study, all patients underwent end-to-side anastomosis (parachute) technique for AVF creation. With an immediate patency (palpable thrill intra operative) [46] was 218 (94.4%). In other study, immediate patency was 78%-90% [46,70,71].
Thrombus is the most common complication of AVF operations with a rate of 3-14.5% [16,44]. In our study, thrombosis was 13% of our patient. These figures were in agreement with the literature data. The most common cause of vascular access thrombosis is venous neointimal proliferation [72]. Similar finding was found [44]. Noninfectious fluid collections (hematoma/seroma/ lymphocele) were 24(10.4%) all management simply by dressing and evacuation of fluid (Figures 1A-1C).
In the studies by Dekhaiya et al. [44] and Schinstock et al. [5] infection was 8% and 26.8% respectively, while in our patients, Infection was found in 17 (7.4%), majority of these cases 10 (4.4%) management with observation (antibiotic) or aspirated and drainage. other seven (3%) infection progressive lead to burst fistulae, which management with emergency surgical intervention.
In the series, steal syndrome was observed in 1.6%-8.0% [5,44,73] while in our study this rate was 3(1.3%). History of diabetic disease was found statistically related to developed steal syndrome complication (p=0.002). However, female gander was not found to be statistically related to steal syndrome (p=0.33). Among these three cases, two cases were management by DRIL procedure, and one case by ligation with permanent tunneled catheters. Aneurysmal degeneration was found in 3.9% of our patients. While other studies it was observed in 2.0% to 8.5% cases [53,73]. Venous hypertension of arm was developed in four cases, we found statistically related between pervious central dialysis catheter used and venous hypertension (p=0.001).
Conclusion
Functional AVF is the gold standard for vascular access for hemodialysis. We report, excellent functional rate (85.7%) of AVF created by parachute vascular anastomosis technique with primary failure rate (14.3%) compare to other study. For that, parachute technique may be suggested as one of optimal selection to create AVF especially in elderly, diabetic patients. The most common complication post AVF fistula was thrombosis 30 (13%), followed by noninfectious fluid collections 24 (10.4%), wound infections 17 (7.4%), bleeding 9 (3.9%), postoperative edema 10 (4.3%), aneurysmal degeneration 9 (3.9%), venous hypertension 4 (1.7%) and steal syndrome 3 (1.3%).
References
- Pauly RP, Gill JS, Rose CL, et al. Survival among nocturnal home haemodialysis patients compared to kidney transplant recipients. Nephrol Dial Transplant. 24(9): 2915-2919 (2009).
- Schold JD, Buccini LD, Goldfarb DA, et al. Association between Kidney Transplant Center Performance and the Survival Benefit of Transplantation Versus Dialysis. Clin J Am Soc Nephrol. 9(10): 1773-1780 (2014).
- Casey ET, Murad MH, Rizvi AZ, et al. Surveillance of arteriovenous hemodialysis access: A systematic review and meta-analysis. J Vasc Surg. 48(5): S48-S54 (2008).
- Vachharajani TJ, Vachharajani V. Obstacles for clinical monitoring in hemodialysis patients because of multiple vascular accesses. Semin Dial. 23(1): 114-116 (2010).
- Schinstock CA, Albright RC, Williams AW, et al. Outcomes of arteriovenous fistula creation after the fistula first initiative. Clin J Am Soc Nephrol. 6(8): 1996-2002 (2011).
- Vazquez MA. Vascular access for dialysis: Recent lessons and new insights. Curr Opin Nephrol Hypertens. 18(2): 116-121 (2009).
- Konner K. History of vascular access for haemodialysis. Nephrol Dial Transplant. 20(12): 2629-2635 (2005).
- Woods JD, Turenne MN, Strawderman RL, et al. Vascular access survival among incident hemodialysis patients in the United States. Am J Kidney Dis. 30(1): 50-57 (1997).
- Astor BC, Eustace JA, Powe NR, et al. Type of vascular access and survival among incident hemodialysis patients: The choices for healthy outcomes in caring for ESRD (CHOICE) study. J Am Soc Nephrol. 16(5): 1449-1455 (2005).
- Dhingra RK, Young EW, Hulbert-Shearon TEE, et al. Type of vascular access and mortality in U.S. hemodialysis patients. Kidney Int. 60(4): 1443-1451 (2001).
- Hoen B, Paul-Dauphin A, Hestin D, et al. EPIBACDIAL: A multicenter prospective study of risk factors for bacteremia in chronic hemodialysis patients. J Am Soc Nephrol. 9(5): 869-876 (1998).
- Manns B, Tonelli M, Yilmaz S, et al. Establishment and Maintenance of Vascular Access in Incident Hemodialysis Patients: A Prospective Cost Analysis. J Am Soc Nephrol. 16(1): 201-209 (2004).
- Navuluri R, Regalado S. The KDOQI 2006 Vascular Access Update and Fistula First Program Synopsis. Semin Intervent Radiol. 26(2): 122-124 (2009).
- Gibbons CP. Primary Vascular Access. Eur J Vasc Endovasc Surg. 31(5): 523-529 (2006).
- Tannuri U, Tannuri ACA, Watanabe A. Arteriovenous fistula for chronic hemodialysis in pediatric candidates for renal transplantation: Technical details and refinements. Pediatr Transplant. 13(3): 360-364 (2009).
- Brescia MJ, Cimino JE, Appel K, et al. Chronic hemodialysis using venipuncture and a surgically created arteriovenous fistula. N Engl J Med. 275(20): 1089-1092 (1966).
- Rodriguez JA, Armadans L, Ferrer E, et al. The function of permanent vascular access. Nephrol Dial Transplant. 15(3): 402-408 (2000).
- Rubens F, Wellington JL. Brachiocephalic fistula: A useful alternative for vascular access in chronic hemodialysis. Cardiovasc Surg. 1(2): 128-130 (1993).
- Weale AR, Bevis P, Neary WD, et al. Radiocephalic and brachiocephalic arteriovenous fistula outcomes in the elderly. J Vasc Surg. 47(1): 144-150 (2008).
- Dagher F, Gelber R, Ramos E, et al. The use of basilic vein and brachial artery as an A-V fistula for long term hemodialysis. J Surg Res. 20(4): 373-376 (1976).
- Lee K, Chong T, Goh N, et al. Outcomes of Arteriovenous Fistula (AVF) Creation, Effect of Preoperative vein mapping and Predictors of Fistula Success in Incident Hemodialysis Patients-A Single-center Experience. 22(5): 382-387 (2017).
- Adequacy H, Adequacy PD, Access V. Updates Clinical Practice Guidelines. Blood Pressure. (2006).
- Bhalodia R, Allon M, Hawxby AM, Maya ID. Comparison of Radiocephalic Fistulas Placed in the Proximal Forearm and in the Wrist. Semin Dial. 24(3): 355-357 (2011).
- Renaud CJ, Pei JH, Lee EJC, et al. Comparative outcomes of primary autogenous fistulas in elderly, multiethnic Asian hemodialysis patients. J Vasc Surg. 56(2): 433-439 (2012).
- Bashar K, Zafar A, Elsheikh S, et al. Predictive Parameters of Arteriovenous Fistula Functional Maturation in a Population of Patients with End-Stage Renal Disease. James LR, ed. PLoS One. 10(3): 1-15 (2015).
- Asif A, Roy-Chaudhury P, Beathard GA. Early arteriovenous fistula failure: a logical proposal for when and how to intervene. Clin J Am Soc Nephrol. 1(2): 332-339 (2006).
- Beathard GA, Arnold P, Jackson J, et al. Physician Operators Forum of RMS Lifeline. Aggressive treatment of early fistula failure. Kidney Int. 64(4): 1487-1494 (2003).
- Yabanoglu H, Bali C, Avci T, et al. The effect of surgeon’s fatigue on early term patency and complications of arteriovenous fistulasâ¯: A prospective cohort study. 25(3): 429-433 (2018).
- Soliman M, Morsy M, Bagul A. Modification of the parachute technique to simplify vascular anastomosis in kidney transplantation. Ann R Coll Surg Engl. 97(1): 79 (2015).
- Al Ganadi A, Alhamati M. Parachute Suture Technique with Arteriotomy by using Aortic Punch in Live Related Renal Transplant. J Transplant Technol Res. 5(2): 2-4 (2015).
- Yabanoglu H, Kus M, Arer IM, et al. Patency rates of the standard (parachute) and diamond-shaped end-to-side anastomosis techniques in arteriovenous fistulas created for hemodialysis. J Coll Physicians Surg Pakistan. 28(8): 597-602 (2018).
- Pushevski V, Dejanov P, Gerasimovska V, et al. Severe Endothelial Damage in Chronic Kidney Disease Patients Prior to Haemodialysis Vascular Access Surgery. Pril (Makedonska Akad na Nauk i Umet Oddelenie za Med Nauk. 36(3): 43-49 (2015).
- Irish AB, Viecelli AK, Hawley CM, et al. Effect of fish oil supplementation and aspirin use on arteriovenous fistula failure in patients requiring hemodialysis a randomized clinical trial. JAMA Intern Med. 177(2): 184-193 (2017).
- Dember LM, Beck GJ, Allon M, et al. Effect of clopidogrel on early failure of arteriovenous fistulas for hemodialysis. A randomized controlled trial. JAMA-J Am Med Assoc. 299(18): 2164-2171 (2008).
- McLafferty RB, Pryor RW, Johnson CM, et al. Outcome of a comprehensive follow-up program to enhance maturation of autogenous arteriovenous hemodialysis access. J Vasc Surg. 45(5): 981-985 (2007).
- Monroy-Cuadros M, Yilmaz S, Salazar-Bañuelos A, et al. Risk factors associated with patency loss of hemodialysis vascular access within 6 months. Clin J Am Soc Nephrol. 5(10): 1787-1792 (2010).
- Sarı F, TaÅkapan H, SıÄırcı A, et al. Evaluation of risk factors for arteriovenous fistula failure in patients undergoing hemodialysis. Erciyes Tip Derg. 38(1): 12-19 (2016).
- Al-Jaishi AA, Oliver MJ, Thomas SM, et al. Patency Rates of the Arteriovenous Fistula for Hemodialysis: A Systematic Review and Meta-analysis. Am J Kidney Dis. 63(3): 464-478 (2014).
- MacRae JM, Dipchand C, Oliver M, et al. Arteriovenous access failure, stenosis, and thrombosis. Can J Kidney Heal Dis. 3(1) (2016).
- Tordoir JHM, Rooyens P, Dammers R, et al. Prospective evaluation of failure modes in autogenous radiocephalic wrist access for haemodialysis. Nephrol Dial Transplant. 18(2): 378-383 (2003).
- Miller PE, Tolwani A, Luscy CP, et al. Predictors of adequacy of arteriovenous fistulas in hemodialysis patients. Kidney Int. 56(1): 275-280 (1999).
- Gjorgjievski N, Dzekova-Vidimliski P, Gerasimovska V, et al. Primary Failure of the Arteriovenous Fistula in Patients with Chronic Kidney Disease Stage 4/5. Open Access Maced J Med Sci. 7(11): 1782-1787 (2019).
- Salako AA, Badmus TA, Igbokwe MC, et al. Experience with arteriovenous fistula creation for maintenance hemodialysis in a tertiary hospital in South-Western Nigeria. In: Saudi Journal of Kidney Diseases and Transplantationâ¯: An Official Publication of the Saudi Center for Organ Transplantation, Saudi Arabia. 29: 924-929 (2018).
- Dekhaiya FA, Hathila TN, Doshi SA, et al. A prospective study of arteriovenous fistula creation in chronic renal failure patients in Bhavnagar, Gujarat, western India. 5(2): 5-9 (2016).
- Gibson KD, Gillen DL, Caps MT, et al. Vascular access survival and incidence of revisions: A comparison of prosthetic grafts, simple autogenous fistulas, and venous transposition fistulas from the United States Renal Data System Dialysis Morbidity and Mortality Study. J Vasc Surg. 34(4): 694-700 (2001).
- Rodrigues AT, Colugnati FAB, Bastos MG. Evaluation of variables associated with the patency of arteriovenous fistulas for hemodialysis created by a nephrologist. J Bras Nefrol. 40(4): 326-332 (2018).
- Voorzaat BM, van der Bogt KEA, Janmaat CJ, et al. Arteriovenous Fistula Maturation Failure in a Large Cohort of Hemodialysis Patients in the Netherlands. World J Surg. 42(6): 1895-1903 (2018).
- Smith GE, Gohil R, Chetter IC. Factors affecting the patency of arteriovenous fistulas for dialysis access. J Vasc Surg. 55(3): 849- 855 (2012).
- Obialo CI, Tagoe AT, Martin PC, Asche-Crowe PE. Adequacy and survival of autogenous arteriovenous fistula in African American hemodialysis patients. ASAIO. (2020)
- Puškar D, Pasini J, SaviÄ I, et al. Survival of primary arteriovenous fistula in 463 patients on chronic hemodialysis. Croat Med J. 43(3): 306-311 (2002).
- Peterson WJ, Barker J, Allon M. Disparities in fistula maturation persist despite preoperative vascular mapping. Clin J Am Soc Nephrol. 3(2): 437-441 (2008).
- Kazemzadeh GH, Modaghegh MHS, Ravari H, et al. Primary patency rate of native AV fistula: Long term follow up. Int J Clin Exp Med. 5(2): 173-178 (2012).
- Sahasrabudhe P, Dighe T, Panse N, et al. Prospective long-term study of patency and outcomes of 505 arteriovenous fistulas in patients with chronic renal failure: Authors experience and review of literature. Indian J Plast Surg. 47(3): 362-369 (2014).
- Arogundade FA, Sanusi AA, Hassan MO, et al. The pattern, clinical characteristics and outcome of ESRD in Ile-Ife, Nigeria: Is there a change in trend? African Health Sciences.
- Bakari A, Nwankwo E, Yahaya S, et al. Initial Five years of Arterio-Venous Fistula creation for Haemodialysis vascular access in Maiduguri, Nigeria. Internet J Cardiovasc Res. 4(2): 1-6 (2012).
- Eadington DW. Delayed Referral for Dialysis: Higher Morbidity and Higher Costs. Semin Dial. 8(5): 258-260 (2007).
- Innes A, Rowe PA, Burden RP. Early Deaths on Renal Replacement Therapy: The Need for Early Nephrological Referral. 7: 467-471 (1992).
- Mendelssohn DC, Curtis B, Yeates K, et al. Suboptimal initiation of dialysis with and without early referral to a nephrologist. Nephrol Dial Transplant. 26(9): 2959-2965 (2011).
- Goncalves EAP, Andreoli MCC, Watanabe R, et al. Effect of Temporary Catheter and Late Referral on Hospitalization and Mortality During the First Year of Hemodialysis Treatment. Artif Organs. 28(11): 1043-1049 (2004).
- Kim DH, Kim M, Kim H, et al. Early Referral to a Nephrologist Improved Patient Survival: Prospective Cohort Study for End-Stage Renal Disease in Korea. PLoS One. 8(1) (2013).
- Gøransson LG, Bergrem H. Consequences of late referral of patients with end-stage renal disease. J Intern Med. 250(2): 154-159 (2001).
- Oliver MJ, Rothwell DM, Fung K, et al. Late creation of vascular access for hemodialysis and increased risk of sepsis. J Am Soc Nephrol. 15(7): 1936-1942 (2004).
- Shah S, Maharjan N, Chapagain D, et al. Arterio-Venous (AV) Fistula: Surgical outcome in College of Medical Sciences Teaching Hospital, Bharatpur, Chitwan. J Coll Med Sci. 8(4): 1-6 (2013).
- Zonnebeld N, Huberts W, van Loon MM, et al. Natural vascular remodelling after arteriovenous fistula creation in dialysis patients with and without previous ipsilateral vascular access. Eur J Vasc Endovasc Surg. 59(2): 277-287 (2020).
- Robbin ML, Greene T, Cheung AK, et al. Arteriovenous Fistula Development in the First 6 Weeks after creation. Radiology. 279(2): 620-629 (2016).
- Kanko M, Sen C, Yavuz S, et al. Evaluation of arteriovenous fistulas made with the diamond-shaped anastomosis technique. Med Sci Monit. 18(9): 2010-2013 (2012).
- Hull JE, Kinsey EN, Bishop WL, et al. Factors Associated with Early Failure of Arteriovenous Fistulae for Haemodialysis Access. Sznitman J, ed. J Vasc Surg. 18(2): 5-9 (2013).
- Al-Hakkak SMM, Al-Faham FSM, Al-Wadees AA, et al. Assessment of arteriovenous fistulas made with the oval-shaped anastomosis technique in the end-stage renal disease patients. Int J Res Pharm Sci. 10(4): 3669-3673 (2019).
- Sen C, Hasanov A. Comparative geometric analysis of diamond and hole techniques in end-to-side microvascular anastomosis. Microsurgery. 28(4): 262-264 (2008).
- Wetzig GA, Gough IR, Furnival CM. One hundred cases of arteriovenous fistula for haemodialysis access: the effect of cigarette smoking on patency. Aust N Z J Surg. 55(6): 551-554 (1985).
- Sampathkumar K, Lobo V, Balasubramaniam J, et al. Vascular Access Creation and Care-Perspective from India. Adv Chronic Kidney Dis. 22(6): 466-470 (2015).
- Bonatti J, Oberhuber A, Schachner T, et al. Neointimal Hyperplasia in Coronary Vein Grafts: Pathophysiology and Prevention of a Significant Clinical Problem. Heart Surg Forum. 7(2): 72 (2005).
- Ferring M, Claridge M, Smith SA, et al. Routine preoperative vascular ultrasound improves patency and use of arteriovenous fistulas for hemodialysis: A randomized trial. Clin J Am Soc Nephrol. 5(12): 2236-2244 (2010).