Review Article - Clinical Practice (2022) Volume 19, Issue 2
Minimal invasive post endodontic monoblock restorations: iii-endocrown review
- Corresponding Author:
- Nagy Abdulsamee
Consultant Prosthodontics
Professor and Head of Dental Biomaterials
Faculty of Dentistry, Deraya University, Egypt
E-mail: nagyabdulsamee@gmail.com
Received: 27 January, 2022, Manuscript No. fmcp-22-52604 Editor assigned: 29 January, 2022, PreQC No. fmcp-22-52604 Reviewed: 15 February, 2022, QC No. fmcp-22-52604 Revised: 20 February, 2022, Manuscript No. fmcp-22-52604 Published: 28 February, 2022, DOI. 10.37532/ fmcp.2022.19(2).1880-1896
Abstract
The most difficult task is the rehabilitation of highly damaged endodontically treated teeth, which have a higher probability of failure than viable teeth. Although the traditional crown supported by radicular metal posts is still extensively used in dentistry, it has been heavily criticized for its invasiveness. There are currently new materials and treatment possibilities based solely on adhesion. The endocrown is advised for the repair of severely damaged molars, which necessitates the use of particular restoration techniques to meet biomechanical criteria. They make it possible to undertake a more conservative, quicker, and less expensive dental procedure. It is recommended when the pulp chamber provides suitable conditions for retention. The coronal portion of an endocrown is merged into the apical projection, which occupies the pulp chamber space and possibly the root canal openings. It preserves tooth structure while being minimally invasive. With the introduction of new ceramics and adhesives, this endocrown may be viewed as a viable alternative to traditional crown-root anchored restorations. Clinical investigations have demonstrated that the endocrown has a long functional life, and it has emerged as a potential option for the cosmetic and functional restoration of endodontically treated molar teeth.
Keywords
Endocrown, post-endodontic restoration, extensive coronal destruction, coronal rehabilitation, molars, monoblock, adhesive restoration.
Abbreviations
ETT: Endodontically Treated Teeth, CAD/CAM: Computer-Aided Design/Computer-Aided Manufacturing, MIT technique: Modified Indirect Technique
Introduction
One of the most difficult tasks in reconstructive dentistry is the repair of severely damaged Endodontically Treated Teeth (ETT) [1]. Many writers condemn the use of posts because of the risks of root perforation, root weakening, and tooth loss when teeth are restored using posts [2]. The introduction of adhesion, pushed by the invention of efficient dentin adhesives, was the genuine breakthrough in the restoration of endodontically treated teeth. The main benefit of adhesive restorations is that macro retentive materials are no longer required if sufficient surface is supplied. Radicular posts have become the exception rather than the rule when performing traditional restorative methods. Less invasive preparations with optimal tissue preservation are currently considered the “gold standard” for recovering ETT [2]. Endocrowns are used to restore endodontically treated premolars [3] and molars [4] with significant tissue loss using this logic.
Pissis (the predecessor of the endocrown approach) was one of the first to describe the ceramic monoblock technique for restoring teeth with substantial coronal structural loss in 1995 [5]. On the other hand, Bindl and Mormann coined the term “Endocrown” in 1999 [6]. The endocrown is a full-coverage porcelain crown that is cemented to a depulped back tooth. Micromechanical retention is achieved in this endocrown by the interior section of the pulp chamber and the cavity border, and micro retention is obtained using the adhesive cementation approach [7]. This approach is especially useful when there is severe crown tissue loss, inter-arch space is limited, and standard post-and-crown rehabilitation is not viable due to insufficient ceramic thickness [8].
Compared to traditional crowns, endocrowns are simple to place and take only a few minutes to heal. The advantages of endocrowns are their low cost, quick preparation time, ease of application, minimum chair time, and attractive qualities [2]. Endocrowns are also an option for teeth with short or atresia clinical crowns, as well as calcified, curved, or short root canals that prevent post-application [4].
Since the turn of the century, the word monoblock has been used in dentistry to describe a single unit. Dr. Pierre Robin invented the ‘Monobloc’ in orthodontics in 1902, combining upper and lower acrylic detachable appliances to treat patients with the syndrome that was eventually named after him. By combining two functional matrices (i.e. the maxilla and the mandible) into a single unit, this one-piece appliance was later used to treat patients with Class II division 1 malocclusion and serves as a predecessor to modern functional appliances [9]. Patients with obstructive sleep apnea have since been treated using modified versions [10].
When executed with the proper technique and indication, the combination of a post and a filling core produces satisfactory long-term outcomes. However, the limitations of intra radicular posts, such as root anatomy, presence of dilacerations and short roots, reduction in tooth strength, treatment complexity in some cases, high cost, and concerns about cementation material, have led clinicians to seek other options, such as the use of adhesive endodontic crowns, also known as Endocrowns [6,11].
Cases of endodontically treated teeth in which an intracanal post cannot be placed, or those with insufficient coronal height, significant destruction, and subsequent dental structure stripping, may benefit from the construction of the entire Endocrown restorations. This treatment entails creating onlays, overlays, and full crowns that make use of the entire depth, extension, and inclination of the pulp chamber’s internal walls to promote restoration stability and retention without the need to remove obstructions (such as filling materials) from the root canals [12-14].
Diseased pulps must be replaced with restorative materials until they can be regenerated [15,16], they have to be replaced by some form of restorative materials. Endodontic and restorative instruments have compromised the root’s stiffness [17,18], therefore the sealing quality and tooth-strengthening capability of endodontic replacement monoblocks are essential considerations.
Due to the remarkable advancements in adhesive dentistry over the last several decades, there are now a variety of resin adhesives with high binding strength and thin film thickness. Because of the advancement of these materials, high-strength restorative materials that can be etched and then luted with adhesives for greater retention are now available. Endocrown is a relatively new indirect restorative procedure for the restoration of endodontically treated posterior teeth that have gained clinical appeal. The coronal component of the endocrown is integrated into the apical projection, which occupies the pulp chamber space and perhaps the root canal openings [19].
Endocrowns are a relatively new treatment, and few dentists arecompetentlyin performing them. Nonetheless, as compared to typical single crowns with posts and cores, they are simple and quick to complete. The goal of this review was to highlight Endocrown by addressing its preparation principles, indications, contraindications, materiautilizedsed in its construction, benefits, drawbacks, and clinical cases described in the literature.
â Preparation for endocrown
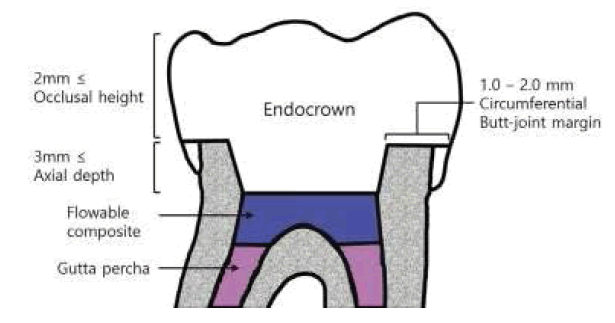
The preparation for the endocrown includes an occlusal reduction to achieve the height of the occlusal space of at least 2 mm in the axial direction. The supragingival or equi gingival circumferential butt-joint margin is approximately 1.0 to 2.0 mm in width, with an axial preparation to make a central retention cavity inside the pulp chamber that eliminates undercuts in the access cavity [5,20]. This design makes both the crown and core a single unit monoblock structure; thus, the root canal preparation can be omitted. The suggested dimensions of the retention cavity are 5 mm diameter and 5 mm depth in molars, but the precise dimensions are not determined [8]. Sometimes, it could be necessary to apply the composite resin on the pulp chamber walls or floor to block the undercuts (FIGURE 1) [19].
Figure 1: Schematic drawing of the tooth preparation for the endocrown restoration. The flowable composite resin could be applied for blocking undercuts [19].
The endocrown preparation consists of a circumferential 1.0 mm-1.2 mm depth butt margin and a central retention cavity inside the pulp chamber that constructs both the crown and core as a single unit monoblock structure and does not take support from the root canals [5,6]. The suggested dimensions are a 3 mm diameter cylindrical pivot and a 5 mm depth for the first maxillary premolars and a 5 mm diameter and a 5 mm depth for molars [5], but the precise dimensions for the preparation of the neutral retention cavity were not determined [8]. The thickness of the ceramic occlusal portion of endocrowns is usually 3 mm-7 mm [20].
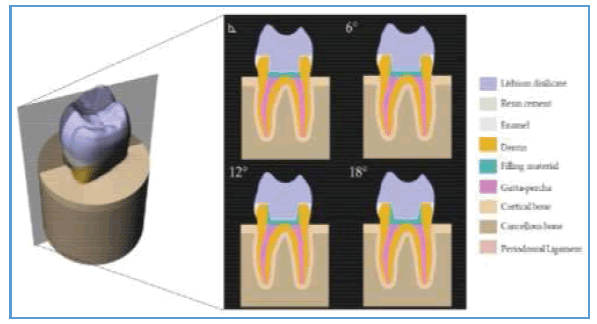
A study evaluated the effect of pulp chamber extension angles and filling material mechanical properties on the biomechanical response of a ceramic endocrown and concluded that flexible filling materials, e.g., resin cement and bulk-fill flowable resin composite, should be preferred to seal the orifice of the root canal system when an endocrown restoration is planned as rehabilitation. In addition, the pulp chamber axial walls should be prepared using 6° and 12° divergences to balance the stress magnitude in the adhesive interface for restorative modality (FIGURE 2) [21].
Indications
Successfully root treated molars in cases with excessive loss of coronal dental tissue due to caries limited interocclusal space due to clinically reduced crown height as seen in partially erupted molars of the mixed dentition stage; roots that are too short, obliterated, dilacerated, or fragile for conventional post and crown; or favourable pulp chamber retention cavity. Not applicable for premolars or incisors due to the ratio of core diameter to remaining dentine radicular walls. Supragingival margins interproximally. The adequate thickness of buccal and palatal cusps. Adequate height of buccal and palatal cusps. Not applicable with less than 50% height [22].
Endocrowns are especially indicated in cases of molars with short, obliterated, dilacerated, or fragile roots. They may also be used in situations of excessive loss of coronal dental tissue and limited interocclusal space, in which it is not possible to attain an adequate thickness of the ceramic covering on the metal or ceramic substructures [23].
Contraindications of endocrown
These include an evidential increase in functional and lateral stresses as with steep occlusal anatomy, wear facets or parafunctional habits; in cases where adhesion cannot be assured; pulpal chambers less than 3 mm in depth; or cervical margins less than 2 mm in width for most of the circumference [24]. In such cases, fullcoverage crowns, with or without post, could be the alternative. Although endocrowns are desirable for all teeth, they should be restricted to the restoration of posterior teeth, especially molars. In a previous study, the endocrowns with premolars were more likely to fail than with the molars [20]. This could be because the premolars have a smaller dental structure area in the pulp chamber and consequently a smaller adhesive surface. Additionally, the configuration of premolars, where the height is greater than the width, could create a long lever arm and hence, increase the risk of adhesive rupture and displacement [23].
Advantages of Endocrowns
They have several advantages over conventional full-coverage crowns. They are easier to handle, less complex, more practical, less expensive, and less time-consuming [25]. Conventional intracanal posts with intraarticular retentive supports for coronal restoration can generate a wedge effect on the root and have a longer laboratory time [26]. Moreover, in the case of failure, the invasive procedure could lead to the larger loss of tooth structure, making it difficult to re-intervene [27].
In the previous studies, the endocrown restorations presented greater fracture strength than indirect conventional crowns retained with glass fiber posts and resin composite cores [4,8]. Some authors showed that the fracture resistance of endocrowns with an occlusal thickness of 5.5 mm was two times higher than that of ceramic crowns with a classic preparation and an occlusal thickness of 1.5 mm [28]. The design of preparation is conservative and involves minimal biological width compared to conventional crowns [29]. In a study of 3D Finite Element Analysis of molars restored with endocrowns and posts during masticatory simulation, teeth restored by endocrowns were potentially more resistant to failure than those with fiber-reinforced posts [30].
Additionally, the normal enamel is still retained after the cavity preparation, which improves the durability of the adhesive system. The bonding surface offered by the pulpal chamber of the endocrown is often equal or even superior to that obtained from the bonding of a radicular post of 8 mm depth [31,32]. However, endocrowns have a disadvantage in debonding and there is a possibility of root fracture because of the difference in the modulus of elasticity between the hard restoration and soft dentin.
Materials used for construction of Endocrown
The recent changes in the methods available for restoring endodontically treated posterior teeth depend on the improvement of the adhesive techniques, composite resin materials, fiber posts, and indirect ceramic materials [33]. Different materials like feldspathic, glass-ceramic, hybrid composite resin, and the newest CAD/CAM (computer-aided design/ computer-aided manufacturing) resin blocks can be used for the fabrication of Endocrown. Reinforced, acid etchable dental ceramics have been the materials of choice for the fabrication34 of endocrowns, because they guarantee the mechanical strength needed to withstand the occlusal forces exerted on the tooth, as well as the bond strength of the restoration to the cavity walls [4,5,34].
Different materials can be used to fabricate an endocrown like feldspathic and glassceramic, hybrid composite, and the newest CAD/CAM ceramic and composite blocks. Scientific literature is still not clear about which material is best indicated for such restorations. The authors prefer micro-hybrid composite resins-lab-made or in the form of CAD/CAM blocks-claiming their stress absorbing properties and their practical benefits like the possibility to modify and repair the surface easily [35]. Lithium-disilicate reinforced glass-ceramics (e.g. IPS e.max Press and CAD, Ivoclar, Schaan-Liechtenstein) may be alternatives to this concept above all for esthetic reasons. Several in-vitro studies and some in-vivo trials have confirmed the validity of this adhesive approach, especially for molars [3,20,36-38]. By relying on adhesion, no radicular posts are necessary anymore on molars and at the present moment, it is difficult to decide if posts are necessary on premolars and front teeth. If yes, they may only be considered in the case of extremely destructed teeth. Consequently, in many instances, restoration of ETT teeth may follow the same principles as the restoration of vital teeth [23].
Clinical cases of Endocrown reported in the literature
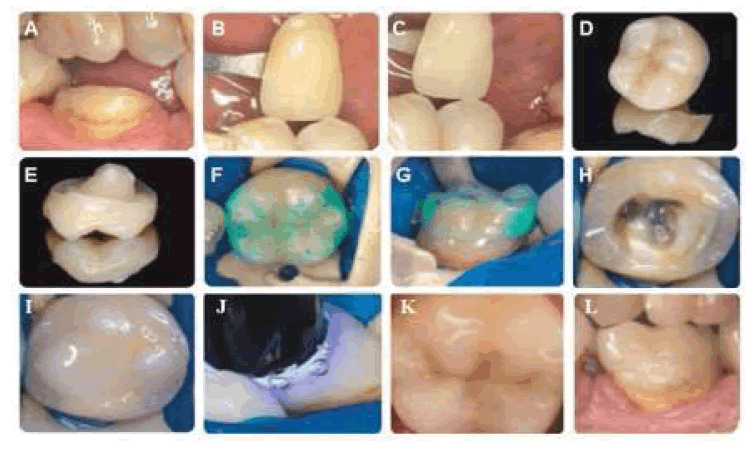
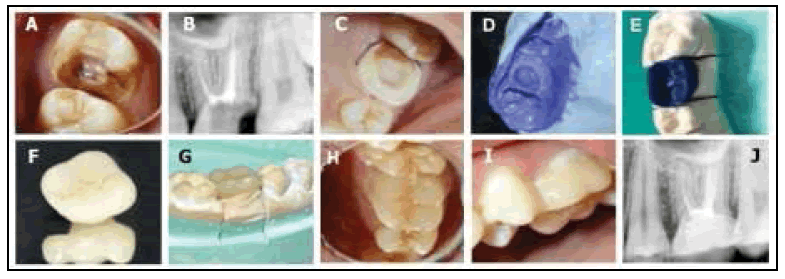
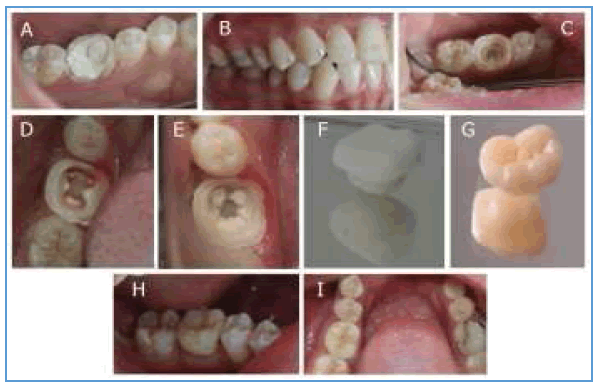
â Case 1: Composite endocrown constructed by indirect technique
This patient attended for root canal treatment and reconstruction of tooth 36. Following root canal treatment, reconstruction techniques allow for preserving the tooth’s hard tissues of sufficient amount to justify producing an endocrown. An endocrown is produced from composite because of the slightly lower cost and ease of repair of any potential damage (FIGURE 3A-FIGURE 3J) [33].
Figure 3: Composite endocrown; A): prepared tooth for an endocrown; B and C): show the two chosen basic shades; D and E): Prepared endocrown fabricated from Premise Indirect composite; F and G): Control of contact points using occlusion spray; H): The tooth following application of bonding system; I): Composite cement on the prepared surface, J): Curing of the cement; K and L): Endocrown - final view (occlusal view and buccal view) [33].
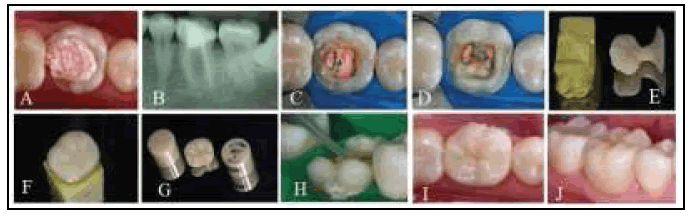
â Case 2: CAD-CAM Endocrowns
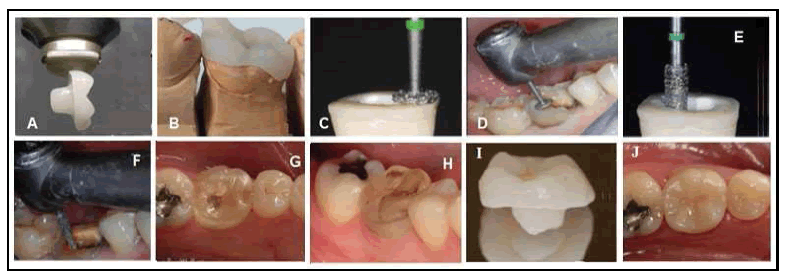
The tooth preparation that is done for Endocrowns is very different compared to that of conventional crowns [39]. Endocrown is manufactured as a one-piece restoration that extends in the pulp chamber of the tooth. It strives to preserve the enamel to facilitate good adhesion and has a supracervical butt joint that is present on the occlusal surface of the tooth [40]. Endocrowns have an extension that goes in the pulpal chamber and thus preserves the canal width that is violated during post-space preparation. Endocrowns can be made through Computer-Aided Designing or by pressure milling (FIGURE 4A and FIGURE 4B) [41].
Figure 4: CAD-CAM Endocrowns: Photo A-J [44].
Steps in preparation of endocrown
Before we start with the tooth preparation for Endocrowns, the first thing that needs to be done is to ensure good endodontic treatment [41].
â Depth of the pulpal chamber
Sufficient enamel should be present to facilitate good adhesion. The pulp chamber should have sufficient depth for better retention of the endocrown. A study conducted concluded that the depth of the pulp chamber is more than 2 mm facilitates better retention of the Endocrown, depth less than 2 mm will lead to fracture whereas more than 5 mm also causes irreversible root fracture [42]. Another study compared the fracture resistance for Endocrowns with depths 5 mm, 3 mm, and 1 mm and concluded that the more the depth of the endocrown in the pulp chamber, the better is the retention produced [43]. The shape of the pulp chamber cavity is generally trapezoid in the lower molars and triangular in the upper molars [41].
â Occlusal preparation
The occlusal reduction focuses on reducing the height of the tooth overall to give appropriate clearance from the opposite tooth. The minimum reduction that is to be done is around 2 mm and is made in the axial reduction. Tooth surfaces are grooved and are then reduced accordingly. A wheel bur should be used for the reduction, and it has to be held parallel to the tooth’s occlusal surface (FIGURE 4C and FIGURE 4D). The aim is to make a flat surface on the tooth, and the extent of the cervical margin is determined. The cervical margin is also called the cervical sidewalk. The extent of the cervical margin should be supragingival, but if required depending on the amount of tooth structure available or any other esthetic requirement, the cervical margin can also be extended subgingivally. In areas where the cervical margin has to change, its position should be done within the limit of 60 degrees [41].
â Axial preparation
During the axial preparation, the focus has to be on removing the undercuts in the pulp chamber (FIGURE 4E and FIGURE 4F). For this purpose, a conical or a cylindrical bur can be used, and the endodontic access cavity and pulp chamber become continuous. Precaution should be taken to not touch the pulpal floor and to not do excessive cutting in the chamber walls that will reduce the thickness of enamel. Once the axial preparation is done, it is very important to finish the walls of the preparation so that there are no rough surfaces since an impression must be made and they will impair the same. A red or yellow band bur can be used to smoothen the walls of the preparation [41].
After the tooth preparation is done, the impression is made for the same in elastomeric materials like polyvinyl siloxane. For CADCAM crowns these impressions are then digitized according to the database of the machine using the biogeneric option. A lithium disilicate block is milled in the machine to make the Endocrown (FIGURE 4G and FIGURE 4H). The fit of the Endocrown is then checked in the patient’s mouth, and all the high points and marginal discrepancies are removed. The fit is rechecked until the most appropriate bite is seen (FIGURE 4I). Once the correct fit is obtained, the crown is sintered, glazing is done, and any pigments, if needed, are added [44].
â Cementation of the endocrown
Cementation of the Endocrown is similar to that of any ceramic crown and requires complete isolation. The internal surface of the restoration must be etched with 5% hydrofluoric acid for 20 seconds and rinsed. The restoration then must be dried for 20 seconds, and a silane coupling agent has to be applied to it. The adhesive cement is mixed and applied on the Endocrown which is then seated on the prepared tooth. Any excess cement is then removed from all the surfaces, and the cement is cured (FIGURE 4J) [44].
â Case 3: Endocrown constructed from lithium disilicate by the lost wax technique
A 22 year old female reported to the department for restoration of maxillary left first molar with a crown. There was extensive destruction of coronal structure and it had adequate interocclusal space. The periapical radiograph revealed endodontically treated root canals with no periapical changes (FIGURE 5A). The gingival tissue was healthy. Endocrown was decided as a treatment option for restoration of this tooth as only half of the residual tooth structure was remaining. Preparation of the tooth (FIGURE 5B and FIGURE 5C) following the principles of Bindl et al [20] and Chang et al, [8], the impression was taken (FIGURE 5D), and a model obtained from this impression upon which wax pattern for the endocrown was done (FIGURE 5E) [45].
Figure 5: Endocrown constructed from lithium disilicate by the lost wax technique Photos A-J [45].
The wax pattern was invested for making a mold into which a melted ceramic pellet of lithium disilicate-based ceramic was injected into this mold which was fired in a furnace at 850°C. Endocrown was fitted on the crown and occlusal adjustments were done with finishing burs. Self Adhesives composite was used for bonding the endocrown to the prepared tooth (Figure 5F and FIGURE 5I) and a prospect-operatingray was taken (FIGURE 5J) [45].
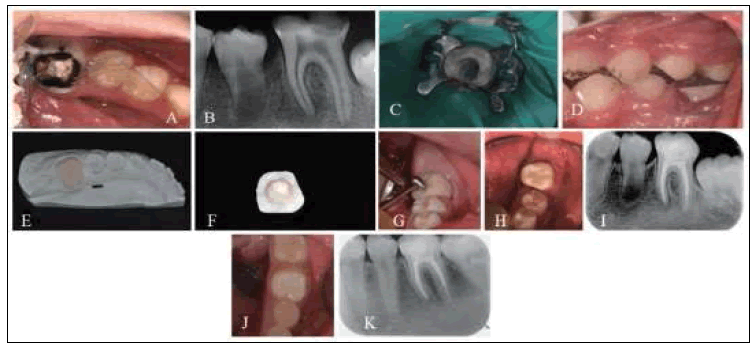
â Case 4: Endocrown constructed by injection molding of leucite reinforced ceramic
A 23-year-old female patient presented for evaluation at the Department of Restorative Dentistry, Bauru School of Dentistry, University of S˜ao Paulo, Brazil. Radiographic and clinical examinations were performed initially (FIGURE 6A and FIGURE 6B), and a provisional restoration of a non-vital molar tooth 46 was identified. After removing the provisional restoration, an endocrown restoration was recommended due to the amount of remaining tooth structure (FIGURE 6C).
Figure 6: Endocrown with Leucite- Reinforced Ceramic Photos A-J [46].
Shade selection was then performed. The surrounding teeth were restored with composite resin in a single section and covered with a rubber dam. The pulp chamber was exposed and the occlusal surface was prepared with a diamond bur (Mani, Japan) (FIGURE 6D). The entire cavity and interocclusal space were evaluated. An impression was obtained using retraction cords. The heavy-bodied and light-bodied impression materials were used. Provisional restoration was constructed from a bisacodyl resin.
The endocrown was fabricated with an injected leucite reinforced ceramic using the heat press technique (FIGURE 6E). The VITA AKZENT Plus was custom applied to enhance the shading and optical characteristics of the restoration (FIGURE 6F and FIGURE 6G). The molar after removal of the provisional restoration (FIGURE 6C) where the tooth is first prepared by making the coronal pulp chamber continuous with the access cavity (FIGURE 6D). The internal surface of the prepared Endocrown was etched with hydrofluoric acid for 60 s, rinsed with running water, dried with an air syringe then was treated with a silane coupling agent. After this, it was cemented onto the prepared tooth shown in FIGURE 6H-FIGURE 6J [46,47].
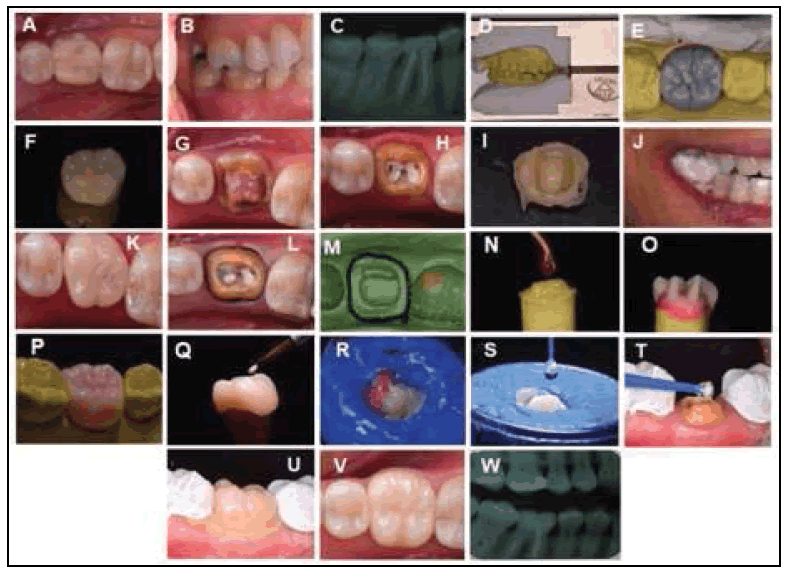
â Case 5: Endocrown) made of pure lithium disilicate based porcelain
A 39-year-old woman, presented to the Graduate clinic of the Bauru Dental School (FOB), University of São Paulo (USP), with the complaint that tooth #36 had an extensive and Unsatisfactory Composite resin restoration (FIGURE 7A), involving all the cusps, and a short coronal portion (FIGURE 7B). After a radiographic exam, the presence of duly filled root canals was found (FIGURE 7C). In clinical planning, the removal of restorative materials and fabrication of an adhesive endodontic crown (Endocrown) made of pure lithium disilicate-based porcelain were indicated. In the first session, the working models were obtained by taking impressions of the mandibular and maxillary hemiarches. The models were mounted in an articulator (FIGURE 7D) to fabricate the provisional restoration by the MIT technique (Modified Indirect Technique) recommended by Fraudeani [48] (FIGURE 7E and FIGURE 7F). This technique makes it easier to obtain the best shape, function, and esthetics in the shortest clinical time. After obtaining the impression, a silicone matrix and another rigid acetate model were fabricated. Using the silicone matrix, the provisional restoration was fabricated with heat-activated acrylic resin, while the purpose of the acetate matrix was to place the provisional restoration into the correct position at the time of relining.
Figure 7: Stages of Endocrown construction from pure lithium disilicate: Photos A-W [47].
In the second session, all the unsatisfactory restorative material was removed from tooth #36, using a diamond-coated rounded tip 1014. Acrylic resin-based material and metal orthodontic wires at the entrances of the root canals were found within the pulp chamber, which was completely removed (FIGURE 7G). After this, the canal entrances were sealed with conventional, chemically activated glass ionomer cement, injected into canal orifices (FIGURE 7H). Afterward, tooth preparation was performed according to the principles followed for Endocrown. In the same session, the provisional restoration was adapted, using the acetate matrix, and relining was performed with self-polymerizing acrylic resin (FIGURES 7I and FIGURE 7J). Next, polishing was performed, paying special attention to the cervical third region of the provisional restoration, to eliminate possible irregularities that could compromise gingival hemostasis. The restoration was cemented with eugenol-free temporary cement (FIGURE 7K).
After 7 days, the provisional restoration was removed and the prepared tooth was prepared for final impression taking (FIGURE 7L), then a final impression was taken (FIGURE 7M) and sent to the lab. At this laboratory stage, the model was poured twice, with the die of the first model being obtained by the alveolus technique [14] (FIGURE 7N), waxing was progressively performed and the wax was sculptured accordingly Kano [49] (FIGURE 7O and FIGURE 7P). The wax pattern of the Endocrown crown was included, filled with Drone lining plaster, and taken to the Programat EP 3000 furnace using the lost wax technique, for 15 min at 906°C degrees. Next, the Lithium disilicate LT tablet, shade A2, was injected into the EP 600 Ips Empress programmable ceramic press furnace, resulting in the fabrication of a monolithic crown in a single block.
In the following session, the patient returned for a try-in of the crown and to test the occlusion, internal and proximal adjustments, since this type of indirect restoration has sufficient thickness for adjustments to be performed before cementation. Right after this, the Endocrown was sent back to the laboratory for the application of the colorant and glaze (Ivoclar Vivadent, Barueri, Brazil) (FIGURE 7Q). The external cervical margin of the crown was protected with wax and then etched with 10% hydrofluoric acid for 20 s (FIGURE 7R), abundantly washed, and dried. Next, two coats of Monobond Silane were applied, with a 1-minute interval between each application (FIGURE 7S). After solvent evaporation, the Scotchbond Multi-Purpose Plus adhesive agent system was applied, without polymerization. Next, the tooth was treated with 37% phosphoric acid for 15 s, then abundantly washed and dried, followed by the application of the Scotchbond Multi-Purpose Plus adhesive system (FIGURE 7T). The primer and adhesive were applied by the manufacturer’s instructions and polymerized. Final cementation on the tooth was done using the All Ceram Core dual cement shade A2 (FIGURE 7U). Final aspect of the restoration (FIGURE 7V); Final radiograph (FIGURE 7W) [47].
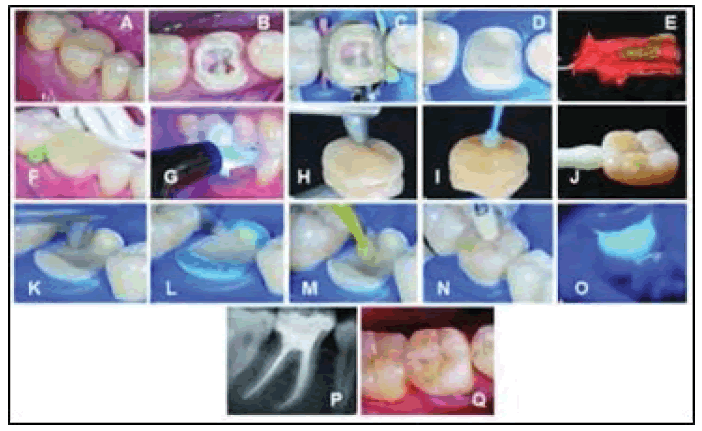
â Case 6: Endocrown constructed by full-adhesive indirect strategy
In the clinical case presented, the large amount of tissues lost due to pathology and to the endodontic treatment supports the use of an “adhesive indirect overlay restoration for devitalized teeth” or “endocrown” instead of a full crown. This technique allows for the conservation of sound dentin and, above all, peripheral enamel, maintaining the possibility to bond margins of the future restorations to it, which is known to have a beneficial effect on marginal stability [50]. The adhesive procedure also prevents the use of a post and a core which would be necessary for a typical crown preparation. Moreover, the adhesive cavity configuration keeps all margins of the restoration away from the periodontium, which is beneficial for hygiene and periodontal health [51]. A conventional indirect composite technique is thus accomplished [52,53].
The indirect restoration is then fabricated in the lab. In that specific case, the endocrown was milled from a CAD/CAM composite resin block and then esthetically modified with a freehand technique. Workflow (FIGURE 8) for this case was as follows:
Figure 8: A-Q: Describe the construction of Endocrown by fulladhesive indirect strategy [33].
1. Photos 8 A-D describe the preparation of the cavity for the indirect restoration A) After 1 week the dental dyscromia is reduced through bleaching. The tooth is ready to be prepared,
2. B) Old composite is removed and the cusps are reduced 2-3 mm, C) Cavity is isolated and adhesively treated. A hybrid composite resin is applied in the mesial and distal boxes to relocate margins occlusally. The use of a transparent shade in the first part of the pulp chamber facilitates the detection of the root canals in case of endodontic reintervention, and D) Lingual and vestibular enamel is refurbished. All dentin is covered by a thin layer of composite resin. The cavity is ready to be impressed.
3. Photos 8 E-G describe the impression and temporization of the cavity: E) An half bite tray records the cavity and the occlusion at the same time, F) The cavity is finally isolated with a layer forming glycerin gel and a soft resin temporary material is inserted into the cavity. Interproximal wedges minimize bleeding and material over-filling and G) The soft resin is then polymerized incorrect occlusion.
4. The indirect restoration is then fabricated in the lab. In that specific case, the endocrown was milled from a CAD/ CAM composite resin block and then esthetically modified with a free-hand technique. Photos 8 H-J describe the adhesive treatment of the workpiece: H) The intaglio surface is first sandblasted, I) A silane coupling agent is applied and a bonding resin is successively spread into the cavity without being pre-cured, and J) The endocrown is ready to be luted.
5. Photos 8 K-M describe the adhesive treatment of the cavity: K) Composite resin inside the cavity is sandblasted, L) Enamel is etched with H3PO4 acid, and M) The bonding resin is applied and left uncured.
6. Photos 8 N, O describe luting of the endocrown: N) A thin layer of a preheated restorative composite resin is used as luting cement and spread into the cavity. Then, the restoration is forced in place manually and then with the help of ultrasonic energy. Excess of luting composite at the margins are removed with a probe and interproximal floss, and O) The full polymerization of the endocrown.
Postoperatively photo 8 P is the final radiograph and 8 Q is the final aspect of the restoration [33].
â Case # 7: Endocrown fabricated from lithium disilicate ceramic (IPS e.Max CAD)
A 23-year-old female was referred to the medicine dental department in UHC Sahloul, Sousse, for treatment of tooth #46. Radiographic and clinical examinations were performed initially, and an extensive glass ionomer cement restoration of a nonvital tooth 46 was identified (FIGURE 9A and FIGURE 9B). The tooth was treated endodontically. After removing the restoration, an endocrown restoration was recommended because of the amount of remaining tooth structure and the thickness of the walls (FIGURE 9C). The prosthetic decision was to restore the tooth [46] with an endocrown fabricated from lithium disilicate ceramic (IPS e.Max CAD). The preparation for the endocrown is different from the conventional complete crown where achieving achieve an overall reduction in the height of the occlusal surface of at least 2 mm in the axial direction and getting a cervical margin or “cervical sidewalk” in the form of a butt joint. The cervical margin has to be supragingival and enamel walls less than 2 mm have to be eliminated. Differences in levels between the various parts of the cervical margin should be linked by a slope of no more than 60° to escape a staircase effect. All other procedures for such preparation are followed. Gutta-percha was removed to a depth not exceeding 2 mm to profit from the saddle-like anatomy of the cavity floor. A nonabrasive instrument was required to maintain the integrity of the canal entrance. No drilling of dentin was carried out. The remaining tooth structure was still strong (FIGURE 9D). We ended the preparation by lining the root canal entrances with glass ionomer cement to protect the orifice of the canal (FIGURE 9E). Impression of the tooth was taken by double impression technique using additional silicone. Selection of the ceramic shade was performed and sent with the impression to the laboratory. A provisional acrylic resin restoration was made by using the bltechnicallyhnic and cemented eugenol-free free temporary cement (FIGURE 9F). The endocrown was fabricated in the laboratory using CCAD-CAMtechnology and was positioned on the master cast (FIGURE 9G). Then we made a try-in of the endocrown and tested occlusion, internal, and proximal adjustments. Right after this, we sent it back to the laboratory for the application of the colorant and glaze. In the following session, the internal surface of the endocrown was etched with hydrofluoric acid, rinsed with water, and dried with an air syringe. Next, a coat of a silane coupling agent was applied for 1 minute and dried.
Figure 9: Endocrown fabricated from lithium disilicate ceramic (IPS e.Max CAD) photos A-I [54].
A rubber dam was used to achieve proper isolation, and then phosphoric acid was applied onto the tooth surface for 15 sec on dentin and 30 sec on enamel, then abundantly washed and dried, applied with adhesive, and polymerized for 20 sec with light curing. A thin layer of a dual polymerizing resin was applied to the prosthetic endocrown and then was inserted into the tooth and polymerized at intervals of 5 seconds, making it easy to remove cement excesses. After that, it was polymerized for 60 seconds on all surfaces. The restoration was examined for any occlusal interference using ceramic finishing instruments (FIGURE 9H). The final restoration is shown in FIGURE 9I [54].
The use of the endocrown in pediatric dentistry
In pediatric dentistry, partially erupted molars with extensive coronal destruction or less coronal height have an insufficient crown height to gain retention for the full crown cast restoration, Endocrown appears to be a suitable option for restoring the endodontically treated teeth in these situations [29]. Two clinical case reports on endocrown restorations performed in partially erupted mandibular and maxillary first molars with extensive coronal destruction due to dental caries [19].
Endocrown on Erupting Permanent First Molars Using a Polyglass Composite Resin
â Case # I: On Erupting lower left mandibular first molar
A 9-year-old male patient, with delayed development and mental retardation, visited the clinic for the disabled in Chonnam National University Dental Hospital with a chief complaint of multiple caries. The intraoral examination revealed that multiple teeth were affected by caries, especially, the left mandibular first molar with extensively destructed coronal structure (FIGURE 10A). On radiographic examination, a periapical lesion was detected, indicating the need for endodontic treatment (FIGURE 10B). The coronal height of the remainder crown of the tooth was less than 3 mm.
Figure 10: Endocrown on Erupting lower mandibular left Permanent First Molars Using with a Polyglass Composite Resin Photos: A-K [19].
Under general anesthesia, multiple restorations with composite resin were done to restore the decayed teeth and root canal treatment was performed on the left mandibular first molar. Due to the insufficient interocclusal space, post-endodontic restoration was planned with a conservative approach using endocrown fabricated with the ceramic-filled polyglass composite resin.
For following appointments, an intramuscular injection of midazolam in conjunction with nitrous oxide was performed to induce conscious sedation. Before the preparation for the endocrown, the shade selection was done and the floor of the pulpal chamber was flattened with a flowable resin. The preparation was initiated and its margin was almost an equigingival or partially subgingival butt joint.
An apical projection cavity into the entire pulp chamber was made for a single unit restoration comprising of the crown and the core (FIGURE 10C). The interocclusal space and the entire cavity were evaluated (FIGURE 10D). An impression was taken with polyvinyl siloxane light and mono body impression materials using a retraction cord. Provisional restoration was constructed with a light-cure material.
The endocrown was fabricated with a polyglass composite resin, in the laboratory (FIGURE 10E and FIGURE 10F). The try-in of the finished endocrown was followed by checking the proximal contacts with the surrounding teeth and the marginal fit on the prepared tooth. The internal adhesive surfaces were abraded with 50 μm aluminum oxide airborne particles at 2 bar for 2 seconds. The tooth surface was etched with 37% phosphoric acid for 20 seconds, rinsed with running water, and dried with oil-free air. The dentin adhesive was applied and lightcured for 20 seconds. A dual curable resin luting cement was then applied on the internal surface of the endocrown. The endocrown was placed on the prepared tooth, and light pressure was applied with a ball burnisher over the center of the restoration to spread the cement uniformly (FIGURE 10G). Light curing was done over the margin, and excessive resin cement was removed. It was then examined carefully for occlusal interference and finished with the composite finishing and polishing system.
The final restoration is shown in the figures below (FIGURE 10H and FIGURE 10I). The clinical and radiographic evaluation revealed no secondary caries, fracture, or defect of the endocrown after a 2-year follow-up (FIGURE 10J and FIGURE 10K) [19].
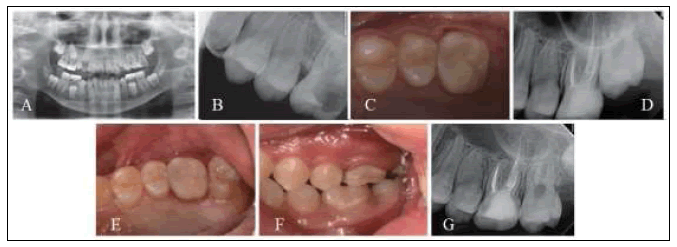
â Case # II: Endocrown on Erupting left Permanent maxillary First Molars
A 9-year-old female patient visited the department of pediatric dentistry at Chonnam National University Dental Hospital with a chief complaint of pain in the left maxillary first molar. A clinical examination showed a pulp polyp resulting from extensive carious exposure. Based on the clinical and radiographic findings, the maxillary left first molar was diagnosed with chronic hyperplastic pulpitis (FIGURE 11A and FIGURE 11B), and the root canal treatment was performed. Considering the amount of remaining tooth structure and the partially erupting stage of the tooth, the endocrown was selected as the post-endodontic restoration along with an additional request for esthetics by the patient.
The tooth preparation and the impression for endocrown were performed after the shade selection, in a similar way as described in the previous case. The Artglass® composite resin was used for the fabrication of the endocrown in the laboratory. After a try-in, the endocrown was cemented using a dual curable resin luting cement (FIGURE 11C and FIGURE 11D). Clinical and radiographic evaluation of a 2-year follow-up showed no secondary caries, fracture, or defect of the tooth (FIGURE 11E-FIGURE 11G) [19].
Figure 11: Endocrown on Erupting left Permanent maxillary First Molar Using with a Polyglass Composite Resin Photos: A-G [19].
Discussion
Planning the restorative treatment of devitalized teeth is a challenge to the dentist, particularly with regards to the choice of the root retention system, making it difficult to decide which is the best treatment option to guarantee the clinical longevity of the treatment [55]. In addition to the type of retainer, the friability of the depulped teeth and variable root anatomy [6,11] and the risk involving a possible root perforation during preparation [2], make it even more difficult to choose the most adequate rehabilitative treatment for these teeth.
In today’s adhesive dentistry era; Endocrown can be considered as a conservative and feasible alternative to conventional post and core crown. Endocrowns are suggested for a tooth that has a clinically low crown with calcification present in the roots or when the roots are very slender and cannot support a post [41]. In cases of molars with obliterated, short, dilacerated, or fragile roots endocrowns are specially indicated. They may be done when there is excessive loss of tooth structure and limited interocclusal space in which case it is not possible to have sufficient thickness of ceramic covering on the metal substructures [7]. But if the depth of the pulp chamber is less than 3 mm or the cervical margin is less than 2 mm wide and if adhesion cannot assured, in such cases endocrowns are contraindicated [41].
The Endocrown fits perfectly with the concept of bio integration and can serve as a most conservative and esthetic option for restoration of non-vital posterior tooth [45]. The recent changes in the methods available for restoring endodontically treated teeth depend on the improvement of the adhesive techniques, composite resin materials, fiber posts, and indirect ceramic materials. Focusing on the relevant advantages: 1) reinforcing of healthy residual dental tissues, 2) bioeconomy of dental tissues and 3) aesthetic, ergonomic and economic advantages, and 4) bioeconomy of periodontal tissues of the conservative bonded techniques helps the clinician to choose the proper restoration.
â Reinforcing of healthy residual dental tissues
The reinforcing effects of adhesive restorations have long been known [56,57]. Conservative bonded restorations are more and more preferred to traditional metal full crowns. 20 The best current approach for restoring endodontically treated teeth seems to: minimize tissue sacrifice, especially in the cervical area so that a ferrule effect can be created, use adhesive procedures to strengthen remaining tooth structure and optimize restoration stability and retention, use post and core materials with physical properties close to those of natural dentin [58].
â Bioeconomy of dental tissues
There is a direct relationship between the remaining tooth structure and fracture resistance. According to Nagasiri and Chitmongkolsuk’s study, greater remaining tooth structure means greater longevity for the teeth [59]. The scientific literature on post-endodontic restoration is unanimous: the prognosis of root-filled teeth depends not only on the success of the endodontic treatment but also on the amount of remaining dentine tissue, and the nature of final restoration [60,61].
A mini-invasive approach should be performed during all the steps of the treatment. It is important to reduce the removal of healthy dental tissues during the endodontic therapy (preparation of access cavity, root canal instrumentation) and during the restoration procedures (post-space preparation, final cavity preparation, selection of the type of the restoration). It is also important to use conservative techniques during irrigation and canal obturation [62]. The lengthening life expectancy and the increasing numbers of elderly persons who want to retain their remaining dentitions for as long as possible, lead the clinician to prefer a conservative restoration, to extend the ‘‘molar life cycle’’ and limit the use of osseointegrated implants [63].
â Esthetic, ergonomic and economic advantages
The chromatic integration of the adhesive restorations offers an immediate appreciable aesthetic result. The ‘‘chameleon effect’’ is excellent in posterior teeth, also in maxillary premolars. In upper posterior elements with aesthetic implications, bleaching techniques and paramarginal preparations (veneer lay preparations) could be necessary to guarantee an aesthetic restoration with minimally invasive performances [64]. The supragingival margins of the partial adhesive restorations result in healthy periodontal tissues and simplify oral hygiene techniques (brushing and flossing) and professional inspection. It is easier to diagnose marginal leakage and to perform the early treatment.
Indirect composite restoration permits repair and replacement: it is an interim stage before placement of a full crown, with the advantage of preserving the residual tissues for subsequent prosthetic treatment [65]. The composite overlay is a restoration that allows for future retreatment of the root canal system [66] and is a treatment option in clinical cases with dubious prognoses. The use of one single material for the direct restoration, for the build-up, and the production of the overlay is another ergonomic advantage. The dental technician procedure for inlay execution is simpler if compared to a full crown. These ergonomic advantages result in economic benefits for patients and dental offices.
â Bioeconomy of periodontal tissues
Preserving intact coronal and radicular tooth structure and maintaining cervical tissue to create a ferrule effect are considered to be crucial to optimize the biomechanical behavior of the restored tooth [2,58,67]. A conservative approach in cavity preparation and restoration often means mini-invasive surgical crown lengthening, and sometimes, no periodontal surgery.
The main disadvantage of full coverage restoration is excessive cutting, which causes excessive application of force and moisture contamination due to subgingival margins. In cases of CAD-CAM end crowns, the restorative portion of the endodontic treatment can be completed in a single visit, which is not possible for cases with full coverage crowns with post cementation [44]. CAD-CAM is the preferred choice for making endocrowns since its more time-saving compared to heat-pressed systems [68]. CAD-CAM systems have the option of biogeneric selection which is a database from which the anatomy of the tooth and the antagonist can be selected, and hence the step of waxing for occlusion is eliminated. In cases where an intraoral scanner is not present with the dentist, a traditional impression can be made and later scanned thereby eliminating the need for an intraoral scanner [44].
The cervical margin for endocrown should be at least 2 mm wide for most of the circumference to facilitate a good adhesion, and if that’s not possible then endocrowns are contraindicated. Glass ceramic restorations are the best choice for making endocrowns as they are biocompatible and have the advantage of biomimicry since the coefficient of wear is very close to enamel [40]. The glass-ceramic restoration also offers a single monolithic restoration that enhances bonding. The cervical sidewalk that is made in endocrown offers a butt joint that enhances bonding, the conventional full coverage restorations require crimping that is prohibited in endocrowns. A broad and stable surface is achieved, which offers a better distribution of compressive forces along the butt joint and the wall of the pulp chamber. The preparation is parallel to the occlusal surface that distributes the force along the major axis of the tooth, and hence that increases retention [40]. For fabrication of the endocrown, a monolithic, lithium disilicate-based ceramic, IPS e.max (Ivoclar Vivadent, Schaan, Liechtenstein) is used, which has adequate physical properties and greater translucence [69]. According to the manufacturer, there are two types of ceramics of the IPS e.max system: the monolithic type with an occlusal dimension of 1.5 mm thickness, without the need for a later porcelain coating; and the lithium disilicate coping (minimum 0.8 mm) covered with a porcelain coating (maximum 0.7 mm). Both have sufficient strength for the restoration of posterior teeth (=/- 400 MPa), in addition to not promoting excessive wear of the antagonist teeth [70]. There is also the possibility of using CAD/ CAM for fabricating restorations in a single block. However, considering that the walls of the preparation were very thin, the option was to use ceramic injection by the lost wax technique [71].
One of the main doubts involve the choice of cement for the fixation of inter radicular posts, considering the innumerable commercial brands in the market, as well as the quality and quantity of cement and its polymerization, its relationship with the root canal length, and the cavity configuration factor (C Factor) [72,73]. There is also the possibility of the presence of air bubbles forming during the insertion of the cement and placement of the glass fiber post [74]. Therefore, simpler, fa,ster, and more conservative alternatives for the restoration of endodontically treated teeth with a short crown are the restoration denominated endocrowns [5,75-77].
The option to use dual cement was justified by the fact that the light-curing unit light needed to pass through the ceramic thickness. Allen is a permanent adhesive resin, dual polymerizing cement; it is radiopaque and has a wide spectrum of applications in indirect restorations. The combination of the two polymerization mechanisms, physical and chemical, guarantee polymerization of the product in situations even in the absence of access to light. It has adequate bonding and mechanical properties and is also easy to apply due to the double-bodied syringe that self mixes the cement and prevents the incorporation of air bubbles into it [47].
Conclusions
In the restoration of ETT with severe coronal tissue loss, endocrowns have been employed as an alternative to traditional post-core and fixed partial dentures. Endocrowns have greater aesthetics and mechanical performance than previous procedures, as well as a lower cost and shorter clinical time [75]. The use of bonded overlays like endocrowns for the coronal restoration of an ETT is becoming more popular as a replacement for traditional full-crown restorations. This shift in thinking is due to a more cautious approach that maintains tooth tissues and allows for reintervention in the event of failure. Endocrowns also avoid several technical processes during the manufacturing process, such as post cementation, core fabrication, temporary crowns, and potential crown lengthening, all of which add to treatment time and cost. All of these stages in between can encourage bacterial infiltration and lead to endodontic re-infection [33].
Full coverage crowns can be replaced with endocrowns, which are a less invasive and conservative option. Endocrowns rely on the pulp chamber for anchorage, which is less damaging than the alternatives, which rely on posts for better retention. The restoration’s margin is supragingival, which helps to preserve the periodontium at the edges and makes impression taking easier, while also preserving more natural tooth structure and increasing strength. When utilized in conjunction with CAD-CAM, glass-ceramic restorations produce a monolithic restoration with increased strength and, owing to the butt joint, a better distribution of forces along the joint and axial walls, which minimizes the force delivered to the pulpal floor. Endocrowns are a suitable option for restoring extensively damaged posterior teeth and are a good example of bio integration.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ree M, Schwartz R. The endo-restorative interface: current concepts. Dent Clin North Am. 54, 345-374 (2010).
- Dietschi D, Duc O, Krejci I, et al. Biomechanical considerations for the restoration of endodontically treated teeth: A systematic review of the literature, part II (evaluation of fatigue behavior, interfaces, and in vivo studies). Quintessence Int. 39, 117-129 (2008).
[Google Scholar] [Crossref]
- Lin CL, Chang YH, Pai CA. Evaluation of failure risks in ceramic restorations for endodontically treated premolar with mod preparation. Dent Mater. 27,431-438 (2011).
- Biacchi GR, Basting RT. Comparison of fracture strength of endocrowns and glass fiber post retained conventional crowns. Oper Dent. 37, 130-136 (2012).
- Pissis P. Fabrication of a metal-free ceramic restoration utilizing the monobloc technique. Pract Periodontics Aesthet Dent. 7, 83-94 (1995).
[Google Scholar] [Crossref]
- Bindl A, Mormann WH. Clinical evaluation of adhesively placed cerec endo-crowns after 2 years--preliminary results. J Adhes Dent. 1, 255-265 (1999).
[Google Scholar] [Crossref]
- Biacchi GR, Mello B, Basting, R. The Endocrown: An alternative approach for restoring extensively damaged molars. J Esthet Restor Dent. 25, 383-390 (2013).
- Chang CY KJ, Lin YS, Chang YH. Fracture resistance and failure modes of CEREC endocrowns and conventional post and core-supported CEREC crowns. J Dent Sci. 4, 110-117 (2009).
- Wahl N. Orthodontics in 3 millennia. Chapter 9: functional appliances to midcentury. Am J Orthod Dentofacial Orthop. 129, 829-833 (2006).
- Cozza P, Ballanti F, Prete L. A modified monobloc for treatment of young children with obstructive sleep apnea. J Clin Orthod. 38, 241-247 (2004).
[Google Scholar] [Crossref]
- Göhring TN, Peters OA. Restoration of endodontically treated teeth without posts. Am J Dent Oct. 16, 313-317 (2003).
[Google Scholar] [Crossref]
- Zarow M, Devoto W, Saracinelli M. Reconstruction of endodontically treated posterior teeth: with or without a post? Guidelines for the dental practitioner. Eur J Esthet Dent Winter. 4, 312-327 (2009).
[Google Scholar] [Crossref]
- Leirskar J, Nordbu H, Thoresen NR, et al. A four to six-year follow-up of indirect resin composite inlays/Onlays. Acta Odontol Scand. 61, 247-251 (2003).
- Tysowsky GW. The science behind lithium disilicate: a metal-free alternative. Dent Today. 28, 112-113 (2009).
[Google Scholar] [Crossref]
- Nakashima M, Akamine A. The application of tissue engineering to the regeneration of pulp and dentin in endodontics. J Endod. 31, 711-718 (2005).
- Goldberg M, Lacerda-Pinheiro S, Jegat N, et al. The impact of bioactive molecules to stimulate tooth repair and regeneration as part of restorative dentistry. Dent Clin North Am. 50, 277-298 (2006).
- Reeh ES, Messer HH, Douglas WH. Reduction in tooth stiffness as a result of endodontic and restorative procedures. J Endod. 15, 512-516 (1989).
- Lang H, Korkmaz Y, Schneider K, et al. Impact of endodontic treatments on the rigidity of the root. J Dent Res. 85, 364-368 (2006).
- Jeong H, Kim S, Kim J, et al. Post-endodontic restoration on erupting first molars using endocrown with a polyglass composite resin: report of two cases. J Korean Acad Pediatr Dent. 46, 111-118 (2019).
- Bindl A, Richter B, Mormann WH. Survival of ceramic-computer-aided/manufacturing crowns bonded to preparations with reduced macro retention geometry. Int J Prosthodont. 18, 219-224 (2005).
[Google Scholar] [Crossref]
- Tribst JPM, Lo Giudice R, dos Santos AFC, et al. Lithium disilicate ceramic endocrown biomechanical response according to different pulp chamber extension angles and filling materials. Materials. 14, 1-13 (2021).
- Rocca GT, Krejci I. Crown and post-free adhesive restorations for endodontically treated posterior teeth: from direct composite to endocrowns. Eur J Esthet Dent. 8, 156-179 (2013).
- Valentina V, Aleksandar T, Dejan L, et al. Restoring endodontically treated teeth with all-ceramic endo-crowns-case report. Serbian Dent J. 55, 54-64 (2008).
- Carlos RB, Thomas Nainan M, Pradhan S, et al. Restoration of endodontically treated molars using all-ceramic endocrowns. Case Rep Dent. 2013, 210763 (2013).
- Randall RC. Preformed metal crowns for primary and permanent molar teeth: a review of the literature. Pediatr Dent. 24, 489-500 (2002).
- Sorensen JA, Engleman MJ. Effect of post adaptation on fracture resistance of endodontically treated teeth. J Prosthet Dent. 64:419-424 (1990).
- Bergman B, Lundquist P, Sjogren U, et al. Restorative and endodontic results after treatment with cast post and cores. J Prosthet Dent. 61, 10-15 (1989).
- Mörmann WH, Bindl A, Luthy H, et al. Effects of preparation and luting system on all-ceramic computer generated crowns. Int J Prosthodont. 11, 333-339 (1998).
- Koleventi A, Sakellari D, Arapostathis KN, et al. Periodontal impact of preformed metal crowns on permanent molars of children and adolescents: a pilot study. Pediatr Dent. 40, 117-121 (2018).
- Dejak B, Mlotkowski A. 3d-finite element analysis of molars restored with endocrowns and posts during masticatory simulation. Dent Mater. 29, e309-317 (2013).
- De Munck J, Van Landuyt K, Peumans M, et al. A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res. 84, 118-132 (2005).
- Peumans M, Kanumilli P, De Munck J, et al. Clinical effectiveness of contemporary adhesives: a systematic review of current clinical trials. Dent Mater. 21, 864-881 (2005).
- Polesel A. Restoration of the endodontically treated posterior tooth. Giornale Italiano di Endodonzia. 28, 2-16 (2014).
- Otto T. Computer-aided direct all-ceramic crowns: preliminary 1-year results of a prospective clinical study. Int J Periodontics Restorative Dent. 24, 446-455 (2004).
- Rocca GT, Bonnafous F, Rizcalla N, et al. A technique to improve the esthetic aspects of CAD/CAM composite resin restorations. J Prosthet Dent. 104, 273-275 (2010).
- Krejci I, Duc O, Dietschi D, et al. Marginal adaptation, retention and fracture resistance of adhesive composite restorations on devital teeth with and without posts. Operative Dentistry. 28, 127-135 (2003).
- Magne P, Knezevic A. Thickness of CAD-CAM composite resin overlays influences fatigue resistance of endodontically treated premolars. Dent Mater. 25, 1264-1268 (2009).
- Lin C, Chang Y, Pa C. Estimation of the risk of failure for an endodontically treated maxillary premolar with MODP preparation and CAD/CAM ceramic restorations. J Endod. 35, 1391-1395 (2009).
- Goodacre CJ, Campagni WV, Aquilino SA. Tooth preparations for complete crowns: an art form based on scientific principles. J Prosthet Dent. 85, 363-376 (2001).
- Höland W, Schweiger M, Watzke R, et al. Ceramics as biomaterials for dental restoration. Expert Rev Med Devices. 5, 729-745 (2008).
- Fages M and Bennasar B. The endocrown: a different type of all-ceramic reconstruction for molars. J Can Dent Assoc. 79, d140 (2013).
- Hayes A, Duvall N, Wajdowicz M, et al. Effect of endocrown pulp chamber extension depth on molar fracture resistance. Oper Dent. 42, 327-334 (2017).
- Dartora NR, de Conto Ferreira MB, Moris ICM, et al. Effect of intracoronal depth of teeth restored with endocrowns on fracture resistance: in vitro and 3-dimensional finite element analysis. J Endod. 44, 1179-1185 (2018).
- da Cunha LF, Gonzaga CC, Pissaia JF, et al. Lithium silicate endocrown fabricated with a CAD-CAM system: A functional and esthetic protocol. J Prosthet Dent. 118, 131-134 (2017).
- Mahesh BA, Gade Vandana G, Patil Sanjay P, et al. Endocrown: conservative treatment modality for restoration of endodontically treated teeth-a case report. Endodontology. 27, 188-191 (2015).
- da Cunha LF, Mondelli J, Auersvald CM, et al. Endocrown with leucite-reinforced ceramic: case of restoration of endodontically treated teeth. Case Rep Dent. 2015, 750313 (2015).
- Menezes-Silva R, Espinoza CAV, Atta MT, et al. Endocrown: A conservative approach. Braz Dent Sci. 19, 121-131 (2016).
- Fradeani M, Giancarlo Barducci. Prosthetic treatment A systematic approach to esthetic, biologic, and functional integration. In: Esthetic rehabilitation in fixed prosthodontics. 2, 154-159 (2008).
[Google Scholar] [Crossref]
- Kano P. Challenging nature: wax-up techniques in aesthetics and functional occlusion. London: Quintessence. (2011).
[Google Scholar] [Crossref]
- Pashley DH, Tay FR, Breschi L, et al. A State of the art etch-and-rinse adhesives. Dent Mater. 27, 1-16 (2011).
- Dietschi D, Bouillaguet S. Restoration of the endodontically treated tooth in Cohen S, Hargreaves KM (eds) pathways of the pulp. St. Louis, Mo: Elsevier Mosby. 777-807 (2006).
[Google Scholar] [Crossref]
- Rocca GT, Krejci I. Bonded indirect restorations for posterior teeth: from cavity preparation to provisionalization. Quintessence Int. 38, 371-379 (2007).
- Rocca GT, Krejci I. Bonded indirect restorations for posterior teeth: the luting appointment. Quintessence Int. 38, 543-553 (2007).
- Dogui H, Abdelmalek F, Amor A, et al. Endocrown: an alternative approach for restoring endodontically treated molars with large coronal destruction. Case Rep Dent. 2018, 1581952 (2018).
[Google Scholar] [Crossref]
- Heydecke G, Butz F, Hussein A, et al. Fracture strength after dynamic loading of endodontically treated teeth restored with different post-and-core systems. J Prosthet Dent. 87, 438-445 (2002).
- Sheth JJ, Fuller JL, Jensen ME. Cuspal deformation and fracture resistance of teeth with dentin adhesives and composites. J Prostheth Dent. 60, 560-569 (1988).
- Hansen EK, Asmussen E, Christiansen NC. In vivo fractures of endodontically treated posterior teeth restored with amalgam. Endod Dental Traumatol. 6, 49-55 (1990).
- Dietschi D, Duc O, Krejci I, et al. Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature: Part 1. Composition and micro-and macrostructure alterations. Quintessence Int. 38,733-743 (2007).
- Nagasiri R, Chitmongkolsuk S. Long-term survival of endodontically treated molars without crown coverage: a retrospective cohort study. J Prosthet Dent. 93, 164-170 (2005).
- Kishen A. Mechanisms and risk factors for fracture predilection in endodontically treated teeth. Endod Topics. 13, 57-83 (2006).
- Assif D, Gorfil C. Biomechanical considerations in restoring endodontically treated teeth. J Prosthet Dent. 71, 565-567 (1994).
- Tang W, Younong W, Smales R. Identifying and reducing risks for potential fractures in endodontically treated teeth. J Endod. 4, 609-610 (2010).
- Simonsen RJ. New materials on the horizon. J Am Dental Assoc. 122, 24-31(1991).
- Magne P. No post, no crown: biomimetic restorative dentistry. (2008).
[Google Scholar] [Crossref]
- Cavalli G. Il restauro del dente trattato endodonticamente. Inc BrennaF, Berschi L, Cavalli G, et al., editors. Odontoiatria Conservativa procedure di trattamento e prospettive future. Capitalo12. Milano: Elsevier Masson (2009).
[Google Scholar] [Crossref]
- Schwartz R, JordanR. Restoration of endodontically treated teeth: the endodontist’s perspective: Part 1. AAE Spring-Summer. (2004).
[Google Scholar] [Crossref]
- McLean A. Predictably restoring endodontically treated teeth. J Canadian Dental Assoc. 64, 782-787(1998).
- Sedrez-Porto JA, de Oliveira da Rosa WL, da Silva AF, et al. Endocrown restorations: a systematic review and meta-analysis. J Dentistry. 52, 8-14 (2016).
- Lepe X, Bales Dj, Jhonson GH. Retention of provisional crowns fabricated from two materials with the use of four temporary cements. J Prosthet Dent. 81, 469-75 (1999).
- Stappert CF, Att W, Gerds T, et al. Fracture resistance of different partial coverage ceramic molar restorations: an in vitro investigation. J Am Dent Assoc. 137, 514-522 (2006).
- Esquivel-Upshaw JF, Rose WF Jr, Barrett AA, et al. Three years in vivo wear: core-ceramic, veneers, and enamel antagonists. Dent Mater. 28, 615-621 (2012).
- Alster D, Feilzer AJ, de Gee AJ, et al. Polymerization contraction stress in thin resin composite layers as a function of layer thickness. Dent Mater. 13, 146-150 (1997).
- Perdigao J, Gomes G, Augusto V. The effect of dowel space on the bond strengths of fiber posts. J Prosthodont. 16, 154-164 (2007).
- Ishikiriama SK, Maenosono RM, Oda DF, et al. Influence of volume and activation mode on polymerization shrinkage forces of resin cement. Braz Dent J. 24, 326-329 (2013).
- Sevimli G, Cengiz S, Oruç MS. Endocrowns: Review. J Istanb Univ Fac Dent. 49, 57-63 (2015).
- Yousief SA, Aman FA, Almutairi MM, et al. CAD-CAM Endocrowns vs. Crowns. EC Dent Sci. 19, 01-07 (2020).
[Google Scholar] [Crossref]