Research Article - Interventional Cardiology (2022)
Major clinical outcomes of stent or balloon angioplasty: A systematic review of successful reperfusion analysis
- Corresponding Author:
- Idiberto José Zotarelli Filho
FACERES-Department of Medicine of Sao Jose do Rio Preto, Sao Paulo, Brazil, E-mail: dr.idibertozotarelli@faceres.com.br
Received date: 16-Aug-2022, Manuscript No. FMIC-22-72001; Editor assigned: 18-Aug-2022, PreQC No. FMIC-22-72001 (PQ); Reviewed date: 01-Sep-2022, QC No. FMIC-22-72001;Revised date: 08-Sep-2022, Manuscript No. FMIC-22-72001 (R);Published date: 15-Sep-2022, DOI: 10.37532/1755-5310.2022.14(S11).281
Abstract
Introduction: According to the World Health Organization (WHO), Cardiovascular Disease (CVD) is the leading cause of death in the world, and in Brazil, CVD is responsible for about 384 thousand deaths per year. In percutaneous coronary intervention, the successful treatment of the coronary lesion is primarily associated with its effective clearance through dilation and/or treatment by some percutaneous device. With the advent of metallic stents and, consequently, the elimination of the phenomenon of immediate elastic retraction of the vessel, there were quite reduced residual stenosis measures concerning those obtained with balloon procedures only.
Objective: It was to highlight the main clinical outcomes of stent or balloon angioplasty through a systematic review of successful reperfusion analysis.
Methods: The rules of the Systematic Review-PRISMA Platform were followed. The research was carried out from February 2022 to June 2022 and developed based on Scopus, PubMed, Science Direct, Scielo, and Google Scholar. The quality of the studies was based on the GRADE instrument and the risk of bias was analyzed according to the Cochrane instrument.
Results: A total of 108 articles were found. In total, 68 articles were fully evaluated and 23 were included and evaluated in this study. And of the total of 23 articles, only 09 articles were developed as the main clinical results. Of the initial total of articles, 16 articles were excluded because they did not meet the GRADE classification, and 45 were excluded because they presented a risk of bias. The results suggest that, even in the era of stents, the analysis of complex lesion morphology can serve as a result stratified, helping in decision making since it significantly impacts late clinical evolution. Also, carotid artery stenting and a retrograde approach had greater odds of successful reperfusion and good functional outcomes at 3 months than balloon angioplasty and an anterograde approach.
Conclusion: The clinical outcomes of angioplasty with a stent showed successful reperfusion concerning the use of the balloon, favoring a faster recovery of patients for hospital discharge.
Keywords
Angioplasty • Cardiovascular disease • Reperfusion • Hospital discharge • Success rate
Introduction
According to the World Health Organization (WHO), Cardiovascular Disease (CVD) is the leading cause of death in the world. It is estimated that 17.7 million people died from CVD in 2015, representing 31% of all deaths globally, and more than ten million occur due to Atherosclerotic Coronary Disease (ACD) [1,2]. In addition, more than three quarters, about 37%, of CVD deaths occur in low- and middle-income countries, and, in Brazil, CVD is responsible for about 384 thousand deaths per year [3].
Furthermore, Coronary Diseases (CD) result from occlusion or narrowing of the arteries due to the formation of atherosclerotic plaques [4]. The CD is associated with a set of risk factors, including advanced age, gender, smoking, obesity, hypertension, diabetes, genetic factors, hypercholesterolemia, and a sedentary lifestyle [5].
The pathophysiological manifestation of CD coronary insufficiency is characterized by the imbalance between the supply and consumption of oxygen at the myocyte level [5,6]. Thus, the goal of treatment of stable angina depends on increased myocardial oxygen supply and reduced demand, which are closely related to contractility, left ventricular parietal stress, myocardial mass, heart rate, and post-load variations determined by blood pressure [4-6].
Within the therapeutic arsenal for the treatment of acute myocardial infarction with ST-segment elevation to the electrocardiogram, primary percutaneous coronary intervention is the most important reperfusion strategy [7-11]. However, its accomplishment within the deadlines defined in the evidence of the studies is a great challenge [12]. The diagnosis of CD is based on the association of clinical history and complementary examinations, since the majority of patients with CD present normal physical examination. Thus, complete anamnesis and evaluation of personal and family history are fundamental [13].
In Percutaneous Coronary Intervention (PCI), the successful treatment of the coronary lesion is primarily associated with its effective clearance through dilation and/or treatment by some percutaneous device. In the era of balloon angioplasty, a reduction in diameter stenosis ≥ 20% associated with residual stenosis <50% at the lesion site at the end of the procedure was acceptable as a procedure success criterion [12,13].
With the advent of metallic stents and, consequently, the elimination of the phenomenon of immediate elastic retraction of the vessel, there were quite reduced residual stenosis measures to those obtained with balloon procedures only. Even so, previous studies in different clinical settings have shown a significant association between the degree of residual stenosis and the risk of adverse events, including restenosis and stent thrombosis [14-16].
The angiographic success of PCI should be accompanied by the absence of Major Adverse Cardiovascular And Cerebrovascular Events (MACCE), characteristically death (cardiac or non-cardiac), Acute Myocardial Infarction (AMI), or emergency revascularization procedure [17,18]. Thus, it is recommended as a criterion for the success of PCI, to obtain angiographic success, 282as defined by residual stenosis <20% by visual analysis, and flow Thrombolysis In Myocardial Infarction (TIMI 3). In cases of AMI with ST elevation, optimal parameters of myocardial perfusion and corrected TIMI flow is also sought after recanalization of the target vessel. The success of the procedure can be obtained by the angiographic success associated with the absence of ACE (defined as a combined outcome of cardiac death, AMI with a CK-MB criterion >5 times the ULN, or urgent myocardial revascularization) during the procedure- reported hospitalization index [19-22].
Therefore, in this scenario, the present study aimed to highlight the main clinical outcomes of stent or balloon angioplasty through a systematic review of successful reperfusion analysis.
Materials and Methods
Study design
The rules of the Systematic Review-PRISMA Platform (Transparent reporting of systematic reviews and meta-analysis-HTTP://www.prisma-statement.org/) were followed.
Data sources and research strategy
The search strategies for this systematic review were based on the keywords (MeSH Terms): “Angioplasty. Cardiovascular disease. Reperfusion. Hospital discharge. Success rate”. The research was carried out in February 2022 to June 2022 and developed based on Scopus, PubMed, Science Direct, Scielo, and Google Scholar. Also, a combination of the keywords with the booleans “OR”, “AND”, and the operator “NOT” were used to target the scientific articles of interest.
Study quality and bias risk
The quality of the studies was based on the GRADE instrument and the risk of bias was analyzed according to the Cochrane instrument.
Results and Discussion
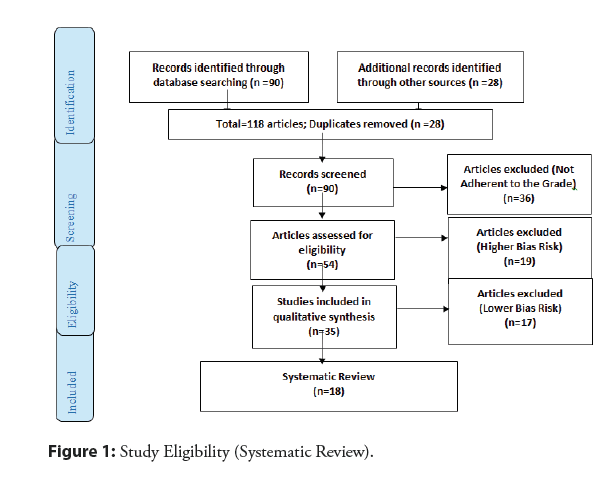
A total of 118 articles were found. Initially, duplication of articles was excluded. After this process, the abstracts were evaluated and a new exclusion was performed, removing the articles that did not address the theme of this article. In total, 78 articles were fully evaluated and 35 were included and evaluated in this study. And of the total of 35 articles, only 18 articles were developed as the main clinical results. Of the initial total of articles, 36 articles were excluded because they did not meet the GRADE classification, and 19 were excluded because they presented a risk of bias that could compromise the credibility of the studies (Figure 1).
In this context, regarding the type of stent, a study showed that the statistical results with the use of conventional stents had 2.8 times greater chances of success in angioplasty than the use of the balloon and 1.55 times greater chances of success in angioplasty than not using the stent. The use of the drug-eluting stent, on the other hand, had 4.09 times greater chances of success in angioplasty compared to the use of the balloon and 2.23 times greater chances of success in angioplasty compared to not using the stent [21]. Also, access via the right radial presented 2.42 times greater chances of success in angioplasty compared to the left radial approach. The right radial approach, on the other hand, presented 2.10 times greater chances of success in angioplasty compared to the right ulnar approach and had 2.12 greater chances of success in angioplasty than the right femoral approach and 2.06 greater chances of success in angioplasty to the right brachial approach [21].
Also, Kastrati, et al. [23] evaluated the impact of the modified ACC/AHA classification on patients treated with stents. In this analysis, the success rate of the procedure was 98.9% for simple injuries (A/B1) and 97.6% for complex injuries (B2/C) (p=0.02). At 30 days, the rate of stent occlusion was lower in simple lesions compared to complex lesions (1.3% vs. 2.7%; p=0.02). At 6-month angiographic follow-up, binary restenosis rates were 24.9% in simple lesions and 33.2% for complex lesions (21.7% vs. 26.3% vs. 33.7% vs. 32.6% for types A vs. B1 vs. B2 vs. C, respectively; p<0.001). Correspondingly, AMI-free survival or target vessel Revascularization (RVA) at 12 months was 81.1% for simple injuries and 75.6% for complex injuries (p<0.001) (85.2% vs. 79.4% vs. 75.9% vs. 75.2%, respectively; p=0.003).
Even with Drug-Eluting Stents (DES), greater angiographic complexity is associated with a worse clinical prognosis [24-26].
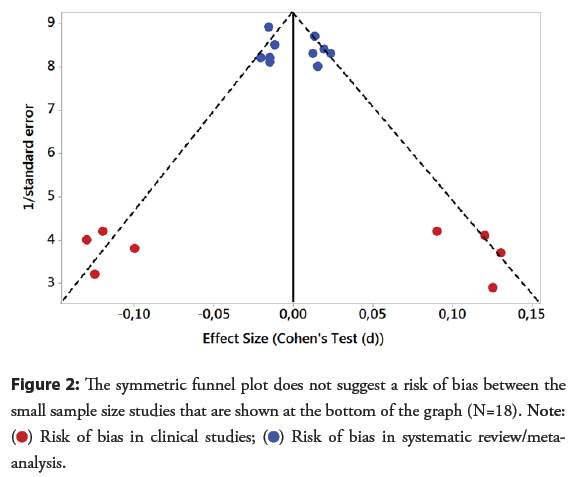
Therefore, these results suggest that, even in the era of stents (including DES), the analysis of complex lesion morphology can serve a result stratified; helping in decision making since it significantly impacts late clinical evolution (Figure 2).
In this scenario, coronary artery disease results in higher morbidity, mortality, and medical costs than any other illness in the developed world. The improvement of coronary artery disease non-invasive detection is still a current problem. According to Palmiero, et al. [27], the primary prevention of cardiovascular events in the elderly is a relevant problem due to the lack of evidence for safe and effective therapy. Life expectancy has increased dramatically in the last two decades, and the proportion of individuals 80 and older has grown rapidly in Europe and the United States. Therefore, it is important to implement the estimation of cardiovascular risk factors in the elderly for the patients’ quality of life and to prolong their healthy life expectancy by choosing the best treatment for each patient, sharing the choice with himself whenever possible, and always remembering elderly Patients usually have multiple comorbidities that require a high number of medications, thus reducing the potential benefits of cardiovascular disease prevention.
It is not uncommon for patients who present with an atherosclerotic coronary disease without ST elevation to have no electrocardiographic or laboratory abnormalities. Because of this, adequate assessment of the probability of atherosclerotic disease is fundamental [4,28]. The presence of one or more risk factors for coronary atherosclerotic disease considerably increases the possibility of being the patient with an acute myocardial ischemic disease. Older age, male gender, family history of coronary disease, diabetes, hyperlipidemia, hypertension, smoking, chronic renal failure, previous infarction or atherosclerotic or carotid disease are widely known risk factors [5].
The initial diagnosis of ACD with supra ST is temporarily confounded with its treatment. Due to the severity and drama of the disease, diagnosis and treatment go hand in hand, with no loss of time [8]. The central symptom of Sudden Cardiac Arrest (SCA) with supra ST is chest pain that lasts for more than 20 minutes, which does not subside with rest, nor with the use of nitrates [9]. As in cases of ACD without supra ST, the pain is usually in oppression, it can radiate to one or both arms, jaw, or nape. Also in these cases some present atypical symptoms, usually elderly, women, or diabetics. For this reason, these patients may reach 30.0% of those who seek the service, and receive less frequently adequate therapy according to some who emergency [9,10].
The CT angiographic strategy the time to diagnosis by 4.0% and the difference in hospitalization costs by 38.0%, without any rate of adverse events to the scintigraphy [7]. The purpose of the ACRIN-PA study was to evaluate the safety of CT angiography in the evaluation of patients with low and intermediate-risk chest pain compared to the traditional approach. None of the patients with negative CT angiography had the primary endpoint analyzed, composed of cardiac death or infarction within the first 30 days after admission. Also, patients in the angio-CT group had a higher rate of discharge from the emergency units (49.6% vs. 22.7%) and fewer days of hospitalization (18 hours vs. 24.8 h, p<0.001), without significant differences in the incidence of coronary angiography or revascularization in 30 days [7].
Over the past two decades, several studies have compared invasive strategy to conservative (or selective invasive) strategy. In meta-analysis by Mehta, et al. [11] (79212 studies the implementation of an invasive strategy patients, resulting in an 18.0% reduction in the relative risk of non-fatal infarction and death (14.4% vs. 12.2%, OR), 0.82, 95% CI 0.72-0.93, p=0.001). Also, another meta-analysis with 7 studies and 8375 patients, Bavry, et al. [28] revealed that the invasive strategy was associated with a 25.0% reduction in death (4.9% vs. 6.5%, RR=0.95% CI 0.63-0.90, p=0.001), 17.0% in non-fatal infarction rates (7.6% vs. 9.1%, RR 0.83 CI 95% 0.72-0, 96) and 31% in rehospitalization due to unstable angina (RR 0.69 95% CI 0.65-0.74 ).
Besides, a study reported techniques on single-stage angioplasty and left common carotid and left internal carotid artery ostium stent in an octogenarian man with a transient ischemic attack. Neurological examination showed transient left-sided visual obscurity or transient amaurosis and right hemiparesis. Duplex imaging of the carotid artery revealed 80% Left Internal Carotid Artery stenosis (LICA) and 95% left Common Carotid Artery ostium (left CCA). Immediate brain magnetic resonance was not possible. Angioplasty and stenting of both lesions (left CCA and LICA) were successfully performed without complications in one session. The stent of the ostial lesion of the common carotid artery and internal carotid artery in one session could be performed even in the acute neurological phase and also in very elderly patients [29].
Also, Drug-coated Balloon Angioplasty (DBA) has emerged as an effective management strategy worldwide. In June 2016, DBA became available for the treatment of minor coronary lesions again in Japan; however, to date, there has been no multicenter analysis in a post-approval real-world clinical setting. Thus, a multicenter study from June 2016 to July 2017, involved a total of 111 lesions (102 patients) treated with DBA for minor de novo coronary lesions enrolled in six Japanese institutions. The primary endpoint was the target lesion revascularization rate at 12 months. Angiographic follow-up parameters were binary restenosis and late lumen loss. Follow-up clinical data at 12 months were available for 106 lesions, excluding five lesions requiring salvage stenting. The target lesion revascularization rate was 5.7% (6/106 lesions). No cardiac death or thrombosis of the target lesion was observed. The binary restenosis rate was 14.4% and the LLL was 0.0017 mm ± 0.37 mm. DBA angioplasty for small coronary lesions again in the real-world environment in Japan is effective with acceptable 12-month results [30].
A retained or retained coronary angioplasty guidewire is a rare but serious complication of coronary interventions. The failed attempt for percutaneous transluminal coronary angioplasty in the left anterior descending artery in a 35-year-old man was complicated by entrapment of the guidewire. Under cardiopulmonary bypass and cardioplegic arrest, the entire length of the trapped guidewire was successfully recovered from the left anterior descending artery and the aorta through an aortotomy following revascularization with the left internal mammary artery [31].
Another study aimed to conduct a longitudinal retrospective and observational study on the impact of angioplasty procedures in patients older than 80 years and with anemia. A total of 185 participants were submitted for eligibility analysis. This study was a longitudinal retrospective and observational model on the profile of patients who followed a follow-up of angioplasty in Brazil. The predictors were anemia and older patients. The multivariate analysis showed that anemic patients older than 80 years who performed statistical angioplasty died, with a significance level of 33.97% in the female group, and 34.40% in the male group, with a total of 68.40% of deaths in terms. The Graph matrix-Plot model shows the results of the regression analysis between continuous predictors and response, with p<0.05 as significant. All the results showed p<0.05 because the presence of the predictor “anemia” negatively influenced the angioplasty procedure in the patients. Thus, it was shown that patients with anemia showed a significant increase in life risk with death occurring after an angioplasty procedure [32].
Besides, a study aimed to conduct a retrospective longitudinal and observational study on the metabolic, behavioral, and clinical profile of patients with angioplasty. A total of 1035 participants were submitted for eligibility analysis. This study followed the longitudinal profile of the patients who followed a retrospective and observational model at Santa Casa Misericórdia Hospital, São José, Brazil. The predictors were: clinical, coronary segment affected, laboratory abnormality, types of procedures, previous AMI, previous ATC, and previous ATC/Actual ATC. The result of the statistical correlation of regression between the continuous predictors and the response was demonstrated using the MatrixPlot model graph. All presented statistical differences with p>0.05, except between the previous predictor’s segment affected xDM, laboratory abnormality x gender, laboratory abnormality × sedentary lifestyle, AMI × gender, and previous ATC × gender. All the latter presented statistical significance, with p<0.05. It confirmed the literary findings in the questions that involve the direct correlation between the main cardiovascular risk factors such as Diabetes mellitus, sedentary lifestyle, age, SAH, smoking, and dyslipidemia in the increase of angioplasty procedures [33].
Moreover, according to the successful use of the right radial approach for angioplasty, a recent systematic review study carried out a systematic review of the main approaches to the use of the right and left distal radial approach. The 39 studies analyzed showed that the distal radial route is reliable, safe, effective, and comfortable. The studies also reported that there is a low rate of obstruction of the distal radial artery. There is also early hemostasis, low risk of hematoma formation, low level of pain perceived artery compartment by patients, reduced risk of a syndrome, saving the radial for possible future myocardial revascularization graft, and the operator’s ability to work at a safe distance from the radiation source. The average success rate in the analyzed studies was 97%. The average rate of occlusion of the distal radial artery was 0.5%. Other complications at the access site were hematoma (0.2%), pulsatile hematoma (<0.1%), infection (0.1%), dissection (0.1%), arteriovenous fistula (<0.1%). Therefore, distal radial access is a reliable, safe, effective, and comfortable route for cardiovascular interventions. They have less arterial obstruction and short hemostasis, with difficulty in cannulation being the main disadvantage [34].
Finally, a meta-analysis study compared the efficacy and safety of acute carotid artery stenting with balloon angioplasty alone in the treatment of cervical injury in occlusions. Clinical trial 285results showed that stent placement in the acute carotid artery was associated with higher odds of a modified Rankin Scale score ≤ 2, OR=1.95 (1.24-3.05), and successful reperfusion, OR=1.89 (1.26-2.83), with no differences in mortality rates or symptomatic intracranial hemorrhage. In addition, a retrograde approach was significantly associated with a modified Rankin Scale score of ≤ 2 (OR, 1.72 (95% CI, 1.05-2.83)), and no differences were found in thrombolysis status. Therefore, carotid artery stenting and a retrograde approach had greater chances of successful reperfusion and good functional outcomes at 3 months than balloon angioplasty and an anterograde approach [35].
Conclusion
The clinical outcomes of angioplasty with a stent showed successful reperfusion concerning the use of the balloon, favoring a faster recovery of patients for hospital discharge and allowing greater comfort to the patient. Also, clinical trial results showed that stent placement in the acute carotid artery was associated with higher odds of a modified rankin scale score, and successful reperfusion with no differences in mortality rates or symptomatic intracranial hemorrhage. Besides, distal radial access is a reliable, safe, effective, and comfortable route for cardiovascular interventions.
References
- WHO-World Health Organization. The top 10 causes of death
- WHO-World Health Organization. Doenças cardiovasculares.
- IBGE-Instituto Brasileiro de Geografia e Estatística
- Chhabra L, Zain MA, Siddiqui WJ. Angioplasty. StatPearls. (2022).
- El Amrawy AM, Camacho-Freire S, Gomez-Menchero A, et al. Ubclavian angioplasty during coronary interventions using radial approach. Kardiol Pol. (2022).
[Google Scholar] [PubMed]
- Miller C, Frood R, See TC, et al. British Society of Interventional Radiology Iliac Angioplasty and Stent Registry: fourth report on an additional 8,294 procedures. Clin Radiol. 74(6): 429-434 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Babunashvili AM, Dundua DP, Kartashov DS, et al. Coronary angioplasty and stenting in patients older than 80 years: Immediate and long-term results. Kardiologiia. 56(7): 54-62 (2016).
[Google Scholar] [PubMed]
- Pang J, David Marais A, et al. Heterozygous familial hypercholesterolaemia in specialist centres in South Africa, Australia and Brazil: Importance of early detection and lifestyle advice. Atherosclerosis. 277: 470-476 (2018).
[CrossRef] [Google Scholar] [PubMed]
- Nasseryan J, Hajizadeh E, Rasekhi A, et al. Investigation factors affecting the first recurrence of coronary artery disease in patients undergone angioplasty using cox survival model. Med J Islam Repub Iran. 30: 441 (2016).
[Google Scholar] [PubMed]
- Ribeiro ALP, Duncan BB, Brant LC, et al. Cardiovascular health in Brazil: Trends and perspectives. Circulation. 133(4): 422-33 (2016).
[CrossRef] [Google Scholar] [PubMed]
- Mehta SR, Cannon CP, Fox KA, et al. Routine vs. selective invasive strategies in patients with acute coronary syndromes: A collaborative meta-analysis of randomized trials. JAMA. 293(23): 2908-17 (2005).
[CrossRef] [Google Scholar] [PubMed]
- Ellis SG, Roubin GS, King SB, et al. Angiographic and clinical predictors of acute closure after native vessel coronary angioplasty. Circulation. 77(2): 372-9 (1988).
[CrossRef] [Google Scholar] [PubMed]
- Rozemeijer R, Wong CW, Leenders G, et al. Incidence, angiographic and clinical predictors, and impact of stent thrombosis: A 6-year survey of 6,545 consecutive patients. Neth Heart J. 27(6): 321-329 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Savage MP, Douglas JS, Fischman DL, et al. Stent placement compared with balloon angioplasty for obstructed coronary bypass grafts. Saphenous Vein De Novo Trial Investigators. N Engl J Med. 337: 740-7 (1997).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Serruys PW, de Jaegere P, Kiemeneij F, et al. A comparison of balloon-expandable-stent implantation with balloon angioplasty in patients with coronary artery disease. Benestent Study Group. N Engl J Med. 331: 489-95 (1994).
[CrossRef] [Google Scholar] [PubMed]
- Costa RA, Sousa AGMR, Moreira A, et al. Trombose de stent farmacológico no "mundo-real": Análise crítica do Registro DESIRE (Drug-Eluting Stent in the Real World). Rev Bras Cardiol Invas. 16: 144-54 (2008).
- Costa JR, Sousa A, Moreira AC, et al. Incidence and predictors of very late (≥ 4 years) major cardiac adverse events in the DESIRE (Drug-Eluting Stents in the Real World)-Late registry. JACC Cardiovasc Interv. 3(1): 12-8 (2010).
[CrossRef] [Google Scholar] [PubMed]
- Parodi G, Valenti R, Carrabba N, et al. Long-term prognostic implications of non-optimal primary angioplasty for acute myocardial infarction. Catheter Cardiovasc Interv. 68(1): 50-5 (2006).
[CrossRef] [Google Scholar] [PubMed]
- Laskey WK, Williams DO, Vlachos HA, et al. Changes in the practice of percutaneous coronary intervention: A comparison of enrollment waves in the National Heart, Lung, and Blood Institute (NHLBI) Dynamic Registry. Am J Cardiol. 87: 964-9 (2001).
[CrossRef] [Google Scholar] [PubMed]
- Cutlip DE, Windecker S, Mehran R, et al. Clinical end points in coronary stent trials: A case for standardized definitions. Circulation. 115: 2344-51 (2007).
[CrossRef] [Google Scholar] [PubMed]
- Toledo JFBD, Gubolino LA, Teixeirense PT, et al. Diagnostic and interventional coronary procedures by the distal radial artery in the anatomical snuffbox: A real world analysis. J Cardiovasc Dis Diagn. 6(5): 337 (2018).
- Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 37(3): 267-315 (2016).
- Kastrati A, Schomig A, Elezi S, et al. Prognostic value of the modified american college of Cardiology/American heart association stenosis morphology classification for longterm angiographic and clinical outcome after coronary stent placement. Circulation. 100(12): 1285-90 (1999).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Genereux P, Redfors B, Witzenbichler B, et al. Angiographic predictors of 2-year stent thrombosis in patients receiving drug-eluting stents: Insights from the ADAPT-DES study. Catheter Cardiovasc Interv. 89(1): 26-35 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Costa JR, Sousa AGMR, Costa RA, et al. To what extent does angiographic complexity influence the late outcomes of patients treated with drug-eluting stents? Comparison between on-label and off-label indications in the DESIRE Registry. Rev Bras Cardiol Invas. 17: 31-8 (2009).
- Gopalakrishnan M, Lotfi AS. Stent thrombosis. Semin Thromb Hemost. 44(1): 46-51 (2018).
- Palmiero P, Zito A, Maiello M, et al. Primary prevention of cardiovascular risk in octogenarians by risk factors control. Curr Hypertens Rev. 15(2): 78-84 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Bavry AA, Kumbhani DJ, Rassi AN, et al. Benefit of early invasive therapy in acute coronary syndromes: A meta-analysis of contemporary randomized clinical trials. J Am Coll Cardiol. 48(7): 1319-25 (2006).
[CrossRef] [Google Scholar] [PubMed]
- Ghasemi M, Mehrpooya M, Ghasemi F, et al. One-stage angioplasty and stenting of ostium of left common carotid artery and stenting of left internal carotid artery. Acta Med Iran. 55(1): 79-81 (2017).
[Google Scholar] [PubMed]
- Funayama N, Muratsubaki S, Kawahatsu K, et al. Clinical outcomes of SeQuent Please paclitaxel-coated balloons for de novo small coronary artery lesion in a Japanese multicenter post-approval registry. Coron Artery Dis. (2019).
[CrossRef] [Google Scholar] [PubMed]
- Ahmad T, Chithiraichelvan S, Patil TA, et al. Surgical retrieval of entrapped coronary angioplasty guidewire from the aorta. Asian Cardiovasc Thorac Ann. 24(1): 81-4 (2016).
[CrossRef] [Google Scholar] [PubMed]
- Neto WPG, de França JCQ, de Godoy MF, et al. Impact of the angioplasty procedure in cohort of the patients older than 80 years with anemia: An observational study. J Cardiovasc Dis Diagn. 7(2): 361 (2019).
- Junior JB, Buchalla M, Valeriano RC, et al. Statistical Approach to Longitudinal Retrospective Study with Over 1,000 Participants Shows Main Predictors of Cardiovascular Disease for Angioplasty. J Cardiol Curr Res. 11(1): 00368 (2018).
- Assumpcao OQ, Assumpcao VPF, Ramos Junior PW, et al. A systematic review of the main approaches to catheterization/ coronary angioplasty by a distal radial artery in the anatomical snuffbox. Interv Cardiol. 12(3): 23-32 (2020).
- Zevallos CB, Farooqui M, Quispe-Orozco D, et al. Acute carotid artery stenting vs. balloon angioplasty for tandem occlusions: A systematic review and meta-analysis. J Am Heart Assoc. 11(2): e022335 (2022).
[CrossRef] [Google Scholar] [PubMed]
 Risk of bias in clinical studies;
Risk of bias in clinical studies;  Risk of bias in systematic review/meta-analysis.
Risk of bias in systematic review/meta-analysis.
