Research Article - Interventional Cardiology (2020) Volume 12, Issue 6
Left main PCI in a peripheral centre in India: A unique challenge
Gurunath Parale*Department of Medicine, Ashwini cooperative hospital, Solapur, Maharashtra, India
- Corresponding Author:
- Dr. Gurunath Parale
Honorary Assistant Professor of Medicine
Ashwini cooperative hospital
Solapur, Maharashtra, India
Email: parale8@yahoo.com
Received date: August 26, 2020 Accepted date: September 11, 2020 Published date: September 18, 2020
Abstract
Aims/Objectives: To study the feasibility, outcome of ULMPCI in a peripheral centre.
Methods: 83 consecutive patients from February 2008 till September 2019 who underwent PCI of left main coronary were included in this study. Data of all these patients with regard to clinical presentation, procedural details and follow up was obtained. Syntax and Euroscore was calculated in all patients. Primary endpoint was MACCE (mortality, stroke, and revascularisation).
Results: Mean age of the patients was 64.3 years, and majority of the patients presented with ACS 54(65%). Majority of patients had multiple risk factors 58(69.9%) and also renal failure 63(75.63%). Mean Syntax score was 23.61 and mean euroscore 36.04. A cumulative MACCE rate at the end of 5 years was 17/83(20.5%). Mean event-free survival was 7.2 years. Except Euroscore which predicted MACCE at 6 months no other parameters including Syntax score were predictive though lower syntax score had higher event free survival.
Conclusion: PCI of left main coronary artery in challenging environment of a peripheral centre is feasible with comparable results and many times life saving
Keywords
Left main; Percutaneous coronary intervention (PCI); Peripheral
Introduction
TAs per the findings published by the Institute of Health Metrics and Evaluation, India has the highest prevalence of coronary artery disease (CAD) [1]. As much as a quarter of all deaths in India are attributable to coronary artery disease [1]. Among all the risk subsets of CAD, occlusion of the left main coronary artery has the highest risk with an increased mortality. It is reported that as much as seventy percent of the Indian population lives in rural India and many of them are required to travel a long distance to access basic health care. It is obvious that they have to travel farther to get access to a tertiary level treatment such as PCI (Percutaneous coronary intervention) [2].
The challenges of doing a PCI in a so-called ‘B’ grade town like ours, away from the glitter of metro cities, are many. These challenges can be broadly included into the following two categories:
• Challenges due to the infrastructure.
• Challenges due to socio-economic issues.
Challenges due to the infrastructure include the following
• Lack of trained para medical personnel.
• Non-availability of experienced surgical back-up team.
• Lack of high-end equipment including cath-lab, IVUS (Intravascular Ultrasound) etc.
In fact, all the PCI procedures included in this study, right from the arterial puncture to stent- deployment, were performed by a single operator without any skilled assistance.
Challenges arising out of socio-economic demographics
• Lack of awareness of the heart disease or its gravity.
• Preponderance of practitioners of ‘alternative medicine’.
• General taboo against any form of intervention.
• Poor penetration of public health-care and Medical Insurance. In fact, a large chunk (70-80%) pays out-of-pocket for the treatment and many of them land in inextricable cycle of poverty after the treatment [2].
These challenges are further compounded while dealing with PCI in a left main coronary artery disease because of its inherent complexity and the risks involved.
Despite these challenges, PCI was deemed essential and performed eventually because without PCI, these patients stared at near- certain death. The uniqueness of this study is due to the unique challenges faced by the cardiologist.
Background
An occlusive disease involving an unprotected left main coronary artery carries a very high risk among all the subgroups of coronary artery disease (CAD) [3,4]. The coronary artery by-pass graft (CABG) surgery is an established technique to provide long-term benefits and reduced mortality in this sub-category of patients [5]. Even though, PCI has surpassed CABG as the most commonly performed re-vascularization procedure in other group of patients, disease of left main coronary artery continues to confound the cardiologist and CABG continues to be a preferred technique in this subset of patients [6]. However, this scenario is slowly changing in recent years, thanks to rapid improvements in the technological finesse of PCI. This is true even in India wherein the national registry has shown an increasing trend of LMPCI [7]. Some of the recent trials have shown comparable results in PCI visa via CABG. Two of the popular trials recently have compared outcome of PCI and CABG in patients with a disease in an unprotected left main coronary artery [8-10].
• SYNTAX (Synergy between PCI with Taxus and Cardiac Surgery).
• PRECOMBAT (Premier of Randomized Comparison of Bypass Surgery versus Angioplasty Using Sirolimus-Eluting Stent in patients with left main coronary artery disease.
Five-year rates of major adverse cardiac and cerebro-vascular events (MACCE) in SYNTAX study were not significantly different following PCI and CABG (36.9% vs. 31.0%; p=0.12). However, repeat re-vascularization was found to be more frequent in PCI group (26.7% vs. 15.5%; p=0.01). The results of MACCE were similar in PRECOMBAT trial) 17.5% vs. 14.3%; p=0.26). The PCI group of patients required more frequent re-vascularization procedures in this trial too.
The data in India on this subject is scarce. Moreover, whatever published scientific data on this subject is available in India comes from larger institutes in the metro cities where multiple operators are involved in the trials and studies [7,11,12]. To our knowledge, the present study is the largest, single-operator study with long- term follow-up, coming out of a peripherally located town under less than ideal conditions.
Methods
This single operator registry consists of analysis of consecutive 83 consecutive patients undergoing unprotected left main PCI from February 2008 to September 2019. Decision to perform PCI was taken after due consideration to coronary anatomy, hemodynamic condition, comorbidities, urgency of the situation and patient preference. A written informed consent was obtained from all patients. Approval of ethical committee was obtained for data analysis. Individual patient’s data, procedural details were obtained from the computerized software or individual case files. Euroscore was calculated in all patients. Angiograms of all patients were reviewed to calculate syntax score. Follow up data was obtained from computerized software, case files. Incomplete patients’ data was refreshed after telephonic contact when required.
Medications
All patients were preloaded with aspirin and clopidogrel or ticagrelor. Intravenous unfractionated heparin was administered to all patients monitoring ACT (Activated clotting time). Gp IIb/IIA inhibitors were used in majority of patients and avoided if bleeding risk was deemed high. All patients were put on dual antiplatelet treatment as per the guidelines.
Procedural details
Complete revascularization was attempted in all except in moribund or very elderly wherein only culprit artery was stented. Bifurcation stenting was done as per standard guidelines. High pressure post dilatations were done in all and final balloon kissing was done after bifurcation stenting and proximal optimization done when indicated. Intravascular ultrasound to optimize stent optimization was done only in recent patients when it was available.
Follow up
Clinical follow up was done in all discharged patients at one month, 3 months and then every 6 months. Stress test was done after 6 months and yearly in those who could walk on treadmill.
Repeat angiogram was done in symptomatic patients or who had stress test changes. Primary end points of study were mortality total and, repeat revascularization like CABG.
Definitions
Left main stenting: Any stent placed in left main coronary either for disease in left main for ostial LAD and circumflex lesions.
Procedural success
Successful deployment of stent in left main with less than 10% residual stenosis and TIMI III flow without major peri procedural complications like shock, cardiac death.
Major adverse cardiovascular and cerebrovascular events (MACCE): Mortality, stroke, revascularization (CABG surgery)
Deaths were considered cardiac if the patient had typical history, ECG documentation of ischemia or sudden death. Rest all deaths were considered non-cardiac.
Statistical analysis
Statistical analysis was done using IBM SPSS Statistical Software (IBM SPSS Statistics version 16.0, IBM SPSS, USA). Continuous variables were expressed as mean+standard deviation (SD) and categorical variables were expressed as percentage. p values ≤ 0.05 were considered significant. Demographic, clinical, angiographic, and procedural variables were tested to determine significant (p<0.05) univariate correlates of immediate and long-term poor outcomes on Cox regression analysis. Multiple variable Cox proportional hazard analyses were then performed, with the enter method for all pertinent covariates. Results of multiple variable Cox analyses are reported as hazard ratios with 95% Confidence Intervals (CI) and p values. Kaplan–Meier survival analysis was used to analyse actuarial survival rates, Mean survival time was reported.
Results
A total of 83 patients were included in the study (Table 1). Mean age of the patients was 64.3 ± 13.7 years with range of 42-91 years. Men comprised 62(74.7%) and females constituted 21(25.30%). A total of 46(55.4%) patients were diabetics, HTN (Hypertension) was present in 45(54.2%) and Multiple-risk factors were present in 58(69.9%) patients. Renal dysfunction was present in 63(75.63%). The most common clinical presentation was ACS 54(65%) unstable angina in 27(32.5%) ST elevation myocardial infarction (STEMI) in 26(31.3%) and Non-ST elevation myocardial infarction (NSTEMI) in 1(1.2%) and rest had stable angina in 29(34.9%). The mean syntax score was 23.61+9.25. Mean EUROSCORE was 36.04+27.73. A total of 12(19.3%) patients had LV dysfunction, moderate (EF 30%- 40%) in 5(7.1%) and severe (<30%) in 7(11.2%).
| Characteristics | |
| Age | 64.3 ± 13.7 |
| Male/Female | 62/21 |
| Diabetic | 46(55.4%) |
| HTN | 45(54.2%) |
| Multiple risk factors | 58 (69.9%) |
| LVEF in % | 46.1+13.9 |
| Syntax score | 23.61+9.25 |
| Euro score | 36.04+27.73 |
| Renal dysfunction | 63(75.63%) |
| Clinical presentation | |
| Stable Angina | 29(34.9%) |
| Unstable Angina | 27(32.5%) |
| NSTEMI | 1(1.2%) |
| STEMI | 26(31.3%) |
Table 1: Basic characteristics.
Lesion location was in Ostial/Shaft LM (Left Main) in 52(62.6%), and in 31(37.35%) patients had at terminal LM (Table 2). Among total 83 lesions single stent procedure was done in 40(48.19%), multiple stents (≥ 2) were used in 41(39.4%) patients.
| Characteristics | Frequency (%) |
| Site of lesion | |
| Ostial/Shaft | 52(62.65%) |
| Terminal | 31(37.35%) |
| Access site | |
| Femoral | 83(100%) |
| Radial | 0 |
| Single stent | 40(48.2%) |
| Multiple stents (≥ 2) | 41(49.4%) |
| Number of vessels intervened | |
| Single vessel (LM alone) | 19(22.9%) |
| Guiding Catheter size | |
| 6F | 0 |
| 7F | 83(100%) |
| LM+1 additional vessel | 23 |
| LM+2 or more vessels | 9 |
| Syntax score | |
| <22 | 43(51.8%) |
| 22-32 | 14(16.9%) |
| >32 | 26(31.3%) |
| Other procedural details | |
| IVUS | 14(16.9%) |
| IABP/ECMO | 0 |
| Mean stent length(mm) | 22.25 ± 11.1 |
| Mean stent Diameter(mm) | 3.18 ± 0.4 |
| ROTA | 0 |
| Kissing Balloon | 10(12%) |
| Cutting balloon | 0 |
Table 2: Angiographic and procedural characteristics (n=83).
Among total 31 terminal/bifurcation lesions, single-stent procedure was done in 14(45.16%) and two-stent procedure was done in 15(48.39%) patients and only thrombus aspiration was done in 2(6.45%) patients. Mean stent length was 22.25 ± 11.1 and mean stent diameter was 3.18 ± 0.4.
All procedure was performed through femoral artery approach. All femoral PCI were done with 7F guiding catheter. Imaging with IVUS was used in 14(16.9%) patients. IABP or ECMO was not utilized in any of the patients.
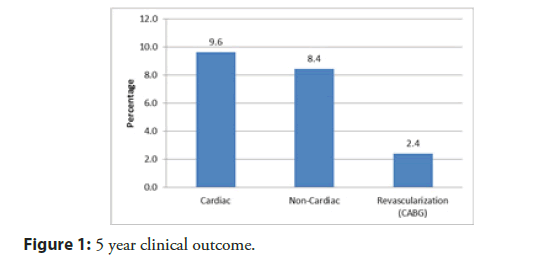
Table 3 shows the details of combined MACCE. A cumulative MACCE rate was 17/83 (20.5%) at the end of 5 years. At end of follow-up period, the incidence of Cardiac death was 8(9.6%), non-Cardiac death was 7(8.4%) and CABG was 2(2.4%).
| In hospital | 30 Days | 3 Months | 6 Months | 1 Year | 3 Years | 5 Years | |
|---|---|---|---|---|---|---|---|
| Cardiac | 3 | 3 | 3 | 5 | 8 | 8 | 8 |
| Non-cardiac | 1 | 1 | 1 | 2 | 2 | 5 | 7 |
| Revascularization (CABG) | 1 | 1 | 1 | 1 | 1 | 1 | 2 |
| Total MACCE | 5 | 5 | 5 | 8 | 11 | 14 | 17 |
Table 3: Events details of MACCE over 5 years (cumulative).
Procedural success was 99% (82/83). There were total of 4(4.8%) in-hospital deaths. 30-day outcome at the end of 30-day follow-up, the incidence of Cardiac death was 3(3.6%) only (all in-hospital) and one non-cardiac. Total MACCE rate upto 30 days were 5(6%) as one patient underwent CABG surgery.
3 months outcome: At the end of 3 months follow-up, the incidence of Cardiac death was 3(3.6%) only (all in-hospital). Total MACCE rate upto 3 months was 5(6%).
6 months outcome: At 6 months, there were a total of 8(9.6%) MACCE and 5(6.0%) cardiac deaths, with total three new deaths out of which 2 cardiac deaths occurring between 3 months and 6 months.
1-Year outcome: At 1 year, there were a total of 11(13.2%) MACCE and 3 new deaths due to cardiac cause between 6 months to 1 year.
3-Year outcome: At 3 year, there were a total of 14(16.8%) MACCE and no new deaths due to cardiac cause between 1-3 years.
5-Year outcome: At 5 year, there were a total of 17(20%) MACCE and no new deaths due to cardiac cause between 1-5 years. Further, there were a total of 2 (2.4%) CABG and one new case of CABG after successful stenting (Figure 1).
Event-free survival
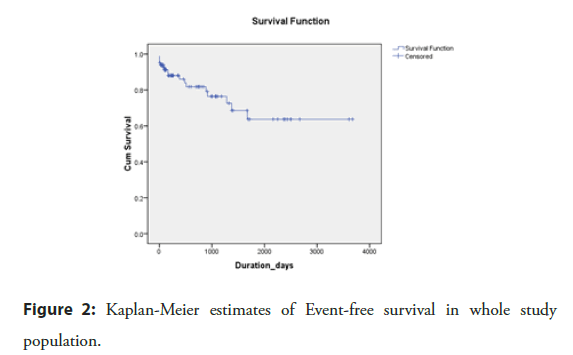
Mean event-free survival was 7.2 years (95% CI 5.95-8.37). Actuarial survival rate free of MACCE was 80%, 78.6%, and 66.7% at 1 year, 3 years, and 5 years, respectively and overall rate was 79.5% (Figure 2).
Predictors of MACCE using univariate and multivariate analyses have been shown in Table 4. Stents in only LM [HR=0.32, (0.12-0.84), p=0.02] was significant factor predicting MACCE on univariate analysis as well as on multivariate analysis LM [HR=0.30, (0.11–0.87), p=0.03].
| Variable | Univariate | Multivariate | ||
|---|---|---|---|---|
| HR (95% CI) | p-value | HR (95% CI) | p-value | |
| Syntax score | 0.72(0.24–2.1) | 0.55 | 0.77(0.23–2.55) | 0.67 |
| Multiple stent | 0.54(0.20–1.42) | 0.21 | 0.71(0.25–2.04) | 0.53 |
| Stents in only LM | 0.32(0.12–0.84) | 0.02 | 0.30(0.11–0.87) | 0.03 |
| Stents in LM bifurcation | 0.94(0.31–2.8) | 0.9 | 0.75(0.05–12.2) | 0.84 |
| Multiple risk factors | 0.83(0.49–1.41) | 0.49 | 0.70(0.23–2.15) | 0.53 |
Table 4: Univariate and multivariate predictors of outcome.
There is no significant difference between duration less than 1 month and more than 1 month among event cases for syntax score (p=0.08) and Euroscore (p=0.73) (Table 5).
| ≤ 1 month | >1 month | z-value | p value | |
|---|---|---|---|---|
| Syntax score | 33.0 ± 6.2 | 24.07 ± 8.21 | 1.76 | 0.08 |
| Euroscore | 41.75 ± 24.66 | 38.27 ± 27.19 | 0.34 | 0.73 |
*Mann-Whitney U test
Table 5: Impact of Syntax score and Euroscore on MACCE at 1 month vs. later.
There is no significant difference between duration of less than 6 months and more than 6 months among event cases for syntax score (p=0.28) whereas, there is highly significant difference between duration of less than 6 months and more than 6 months among event cases for Euroscore (p=0.008) (Table 6).
| ≤ 6 months | >6 months | z-value | p value | |
|---|---|---|---|---|
| Syntax score | 24.82 ± 9.2 | 22.89 ± 9.3 | 1.08 | 0.28 |
| Euroscore | 45.70 ± 25.1 | 30.29 ± 22.8 | 2.65 | 0.008 |
*Mann-Whitney U test
Table 6: Impact of Syntax score and Euroscore on MACCE at 6 months vs. later.
Syntax score ≤ 32 vs. syntax score >32
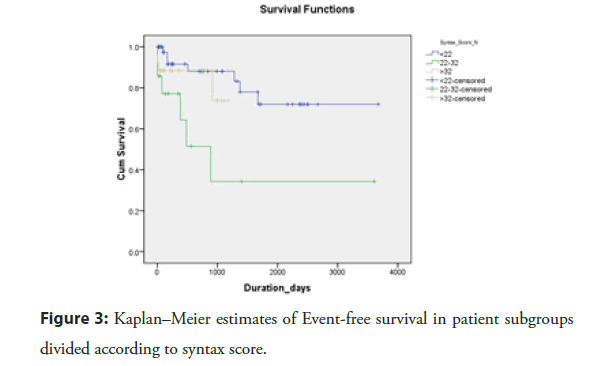
Patients with syntax score ≤ 32 had higher mean event-free survival [7.32 years (95% CI 6.0–8.64)] compared to patients with syntax score >32 [2.60 years (95% CI 2.11-3.10), p=0.55] (Figure 3).
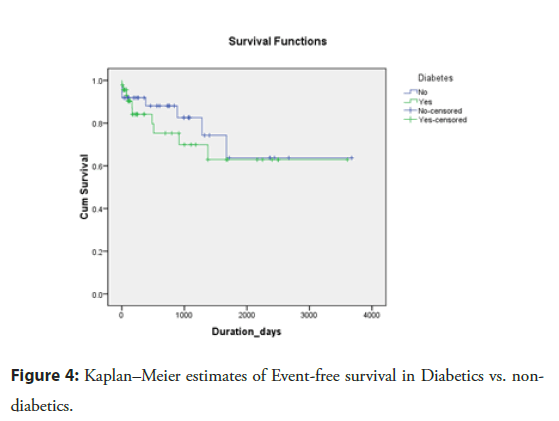
Diabetes vs. Non-diabetes
Diabetics vs. Non-Diabetic patients (Figure 4): Non-diabetic patients had a more mean event-free survival comparable with diabetic patients [7.36 years (95% CI 5.60–9.13) vs. 6.78 years (95% CI 5.14–8.41), p=0.54]. In non-diabetic patients, 5-year event-free survival rate was 81.1% while in diabetic patients the respective survival rate was 78.3%, which was not statistically different (p value=0.54) (Figure 4).
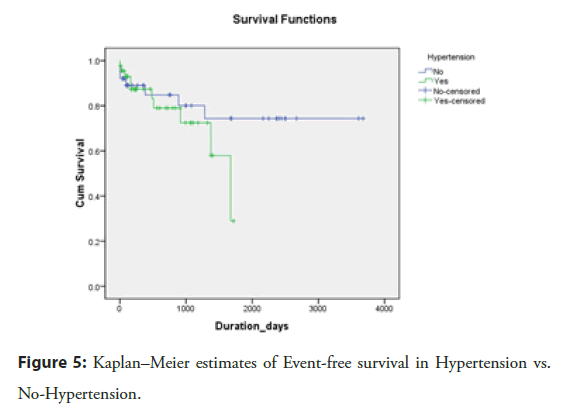
Hypertension vs. No-hypertension
Hypertension vs. No-Hypertension patients (Figure 5): No- hypertension patients had a mean event-free survival comparable with hypertension patients [7.86 years (95% CI 6.39-9.32) vs. 3.55 years (95% CI 2.94-4.16), p=0.33]. In non-hypertension patients, 5-year event-free survival rate was 81.6% while in hypertension patients the respective survival rate was 77.8%, which was not statistically different (p value=0.33).
Figure 5: Kaplan–Meier estimates of Event-free survival in Hypertension vs. No-Hypertension.
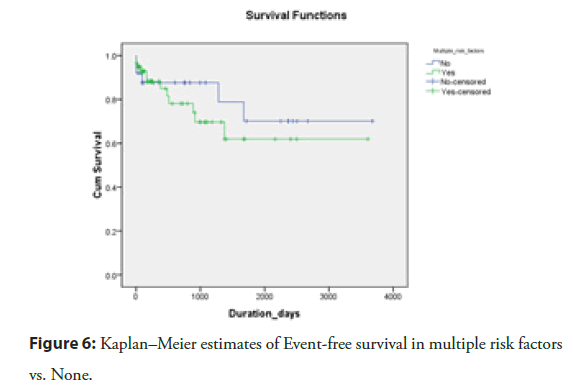
Multiple risk factors vs. none
Patients with no risk factors had higher a mean event-free survival comparable with multiple risk factor patients [7.78 years (95% CI 6.03-9.53) vs. 6.77 years (95% CI 5.23-8.31), p=0.49] (Figure 6). In patients without risk factors, 5-year event-free survival rate was 80.0% while in multiple risk factor patients the respective survival rate was 79.3%, which was not statistically different (p value=0.49).
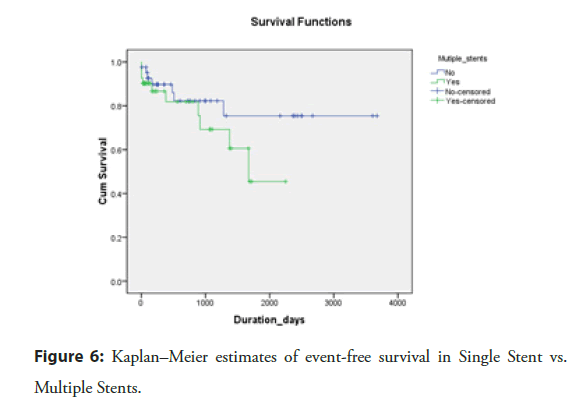
Single stent vs. multiple stents
Single Stent vs. Multiple Stents (Figure 7): Single stent patients had higher a mean event-free survival comparable with multiple stents patients [7.96 years (95% CI 6.53-9.39) vs. 4.20 years (95% CI 3.25-5.15), p=0.20]. In single stent patients, 5-year event-free survival rate was 83.3% while in multiple stent patients the respective survival rate was 75.6%, which was not statistically different (p value=0.20).
Discussion
The study presented here is a single-operator, observational study on PCI in patients with disease involving un-protected left main coronal artery. The uniqueness of this study is due to the fact that it was done in a peripherally located town with typical challenges pertaining to infrastructure and socio-economic issues.
Despite the challenges and the sub group of patients with a high risk, the procedural success rate was 99% which is comparable to other similar studies (Meliga et al. JACC 2008) [13]. The in- hospital mortality in this technically challenging cohort group was a low of 4.8% and comparable to larger, multi-centric trials conducted in well-equipped centres. The low mortality in this study was despite the fact that five of these patients were in severe cardiogenic shock while one of the patients had a 100% occlusion of the LMCA (Left Main Coronary Artery) and survived repeated cardiac arrests. Three of them suffered near cardiac arrest.
Thirty-day MACCE (6%) may appear more when compared to the PCI arm of LE MANS study (4.8%) and the study by Boudriot et al. (4%) [14,15]. We are inclined to attribute the lower 30-day mortality in these studies to the fact that high-risk patients were excluded unlike our study. The present study may be compared to DELFT registry consisting of emergent PCI [13]. This study had a higher event rate (11.4%) after 30 days. The event rate in the present study (6%) is comparable to the Indian study by Goel et al. (8%) [11].
The rate of MACCE at one year in our study (13.2%) was lower compared to other studies including the SYNTAX study [9,13-16] This can be attributed either to the smaller number of patients in the present study or the less complex anatomy (mean SYNTAX score 23.61). Nonetheless, the rate of MACCE at three years (18.07%) and five years (20.48%) is comparable to these studies. MACCE in study of Modi et al. was 0% at 1 year [12]. However majority of patients in their study were stable patients unlike our study where ACS was the presenting feature in the majority.
Event free survival
Mean event-free survival was 7.2 years. Actuarial survival rate free of MACCE was overall 79.5%.
Predictors of MACCE: Amongst the different variables to predict MACCE like syntax score, number of stents, stent in LM only or extending to bifurcation stent only in LM was the only predictor in both univariate and multivariate analysis. Other variables were not predictive. In the Indian study by Modi et al. too number of stents and syntax score were not predictive [12].
Neither syntax nor euroscore could predict MACCE at one month vs. MACCE after one month. However euroscore was highly predictive of MACCE at 6 months vs. after 6 months (p=0.008). We could not come across any study utilizing euroscore to predict MACCE in LM PCI.
In a sub analysis with regard to SYNTAX score, a score of less than or equal to 32 had a higher event free survival (7.32 years) compared to score of more than 32 (2.60 years). This is comparable to other studies [9,11,16]. Euro score sub analysis did not reach significance probably because of high baseline score (mean 36.04). In the sub analysis of single versus multiple stents, no statistical difference was found. However, whenever multiple stents were deployed, the rate of MACCE tended to be higher. Similarly, the rate of MACCE had a tendency to be higher in patients with diabetes and hypertension despite the lack of a statistical significance. A larger and a longer extension of this study may perhaps reveal the significance of higher rate of MACCE in these sub groups.
Thus despite unique multiple infrastructural and socioeconomic challenges faced, the results in this study of PCI of unprotected LMPCI are comparable to studies/trials done in near ideal environment. These results assume further significance when one glances at patient demographics with advanced age, high baseline euroscore and majority patients having renal dysfunction and ACS (Acute Coronary Syndrome) at presentation.
Limitations of this study are as below
• Small sample size.
• A single-operator study will not reflect varying skill and expertise of multiple operators. It may also involve individual bias in decision-making.
Uniqueness of the study: Done in a peripheral centre without trained and skilled assistance or high-end equipment in a patient population with limited resources, no other definitive option and facing near certain death.
Conclusion
PCI in an unprotected left main coronary artery is not just feasible but can also be a life-saver in a peripheral centre despite infrastructural challenges in the hands of skilled and experienced operator.
Acknowledgments
With grateful appreciation to Mr. Anil Gaikwad and Mr. Wasim Bennishirur.
References
- Institute of Health Metrics and Evaluation. GBD Compare. (2010).
- Kumar R. Academic institutionalization of community health services: way ahead in medical education reforms. J Family Med Prim Care. 1: 10-9 (2012).
- Harris PJ, Harrell FE Jr, Lee KL, et al. Survival in medically treated coronary artery disease. Circulation. 60: 1259-69 (1979).
- Proudfoot WJ, Bruschke AV, MacMillan JP, et al. Fifteen year survival study of patients with obstructive coronary artery disease. Circulation. 68: 986-97 (1983).
- Yusuf S, Zucker D, Peduzzi P, et al. Effect of coronary artery bypass graft surgery on survival: overview of 10 year results from randomised trials by the coronary artery bypass graft surgery trialists collaboration. Lancet. 344: 563-70 (1994).
- Ludman PF. On behalf of British Cardiovascular Intervention Society. BCIS audit returns: adult interventional procedures. (2015).
- Ramakrishnan S, Mishra S, Chakraborty R, et al. The report on the Indian coronary intervention data for the year 2011--National Interventional Council. Indian Heart J. 65(5): 518-521 (2013).
- Alasnag M, Yaqoub L, Saati A, et al. Left main coronary artery interventions. Interv Cardiol. 14(3): 124-130 (2019).
- Morice MC, Serruys PW, Kappetein AP, et al. Five-year outcomes in patients with left main disease treated with either percutaneous coronary intervention or coronary artery bypass grafting in the synergy between percutaneous coronary intervention with taxus and cardiac surgery trial. Circulation. 129: 2388-94 (2014).
- Ahn JM, Roh JH, Kim YH, et al. Randomized trial of stents versus bypass surgery for left main coronary artery disease: 5-year outcomes of the PRECOMBAT study. J Am Coll Cardiol. 65: 2198-206 (2015).
- Goel PK, Jatain S, Khanna R, et al. Left main PCI: An observational analysis from large single-centre experience. Indian heart journal. 68: 36-42 (2016).
- Modi R, Patted S, Halkati P, et al. Lembe Study: Left Main PCI in Belgaum. J Clin Exp Cardiolog. 8: 547 (2017).
- Meliga E, Garcia-Garcia HM, et al. Longest available clinical outcomes after drug-eluting stent implantation for unprotected left main coronary artery disease, the DELFT (Drug Eluting stent for Left main) Registry. J Am Coll Cardiol. 51: 2212-2219 (2008).
- Buszman PE, Buszman PP, Kiesz RS, et al. Early and long-term results of unprotected left main coronary artery stenting: the LE MANS (Left Main Coronary Artery Stenting) registry. J Am Coll Cardiol. 54: 1500-1511 (2009).
- Boudriot E, Thiele H, Walther T, et al. Randomized comparison of percutaneous coronary intervention with sirolimus-eluting stents versus coronary artery bypass grafting in unprotected left main stem stenosis. J Am Coll Cardiol. 57: 538-545 (2011).
- Morice MC, Serruys PW, Kappetein AP, et al. Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (syntax) trial. Circulation. 121: 2645-2653 (2010).