Research Article - International Journal of Clinical Rheumatology (2018) Volume , Issue
Knee OA management: A cost-effectiveness analysis of platelet-rich-plasma versus hyaluronic acid for the intra-articular treatment of knee OA in France
- *Corresponding Author:
- Stefano Landi
Department of Management
University “Ca’ Foscari” Venice
Venice, Italy
E-mail: stefano.landi@unive.it
Abstract
Objectives: The aim of this work is to carry out an economic evaluation of the intra-articular (i.a.) use of the platelet-rich plasma (PRP) therapy in the short period treatment for knee osteoarthritis (OA). Recently the scientific literature has shown the effectiveness of this treatment. The comparator adopted is the Hyaluronic acid (HA) which represents the standard i.a. therapy.
Methods: A cost-effectiveness analysis was performed using a decision tree model. The effectiveness outcomes are reported in terms of Quality Adjusted Life Year (QALY). The costs are reported in Euro (€) currency evaluated in 2016. Deterministic and probabilistic sensibility analyses are reported in order to evaluate the robustness of the results and account for the different sources of uncertainty.
Results: The PRP therapy results more costly but also more effective than HA. Using a Willingness to pay thresholds of € 10,000/QALY, the PRP is cost-effective with respect to HA, for patient with moderate to severe knee OA, presenting an Incremental Cost Effectiveness Ratio (ICER) of €760 per QALY.
Keywords
Platelet-rich plasma, hyaluronic acid, cost effectiveness, cost-utility, knee osteoarthritis, knee osteoarthritis management
Introduction
Osteoarthritis (OA) is a chronic and degenerative pathology that affects joints in particular hands, knee, hip and lower back resulting in joint inflammation with associated pain, stiffness and loss of movement. Its incidence turns out to be higher in the population older than 60-years-old, for whom prevalence is estimated 10% worldwide [1-5]. As shown in Global Health Observatory data repository musculoskeletal diseases are the 8th in the whole world and the 4th in western countries for disability adjusted life years (DALYs) [6,7]. OA results to be the 11th out of 291 pathologies for burden of disability (YLDs) and 38th per DALYs [8,9].
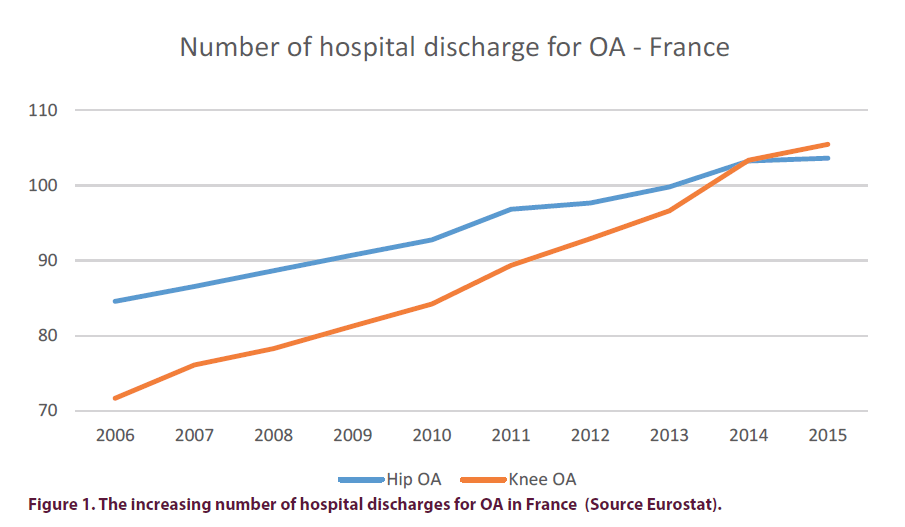
In France Knee OA prevalence was estimated in a range from 2.1% to 10.1% for men and from 1.6% to 14.9% for women (in a population of 40-75 years old). The knee standardized prevalence was 4.7% for men and 6.6% for women, respectively [10].According to data on Hospital discharges by diagnosis, provided by Eurostat, OA has an important impact on health care activity.
In France hospital discharges for OA were around 206,000 (103,236 related to hip and 103,334 related to knee), that were the 2% of the discharges with an average hospital stay of 7.5 days in 2014. These numbers are increasing steadily every year (Figure 1 and Table 1). In France hospital discharges for OA were around 156,000 (84,583 hip and 71,703 knee) in 2006 and 190,000 (97,654 hip and 92,902 knee) in 2012.
| Hip OA | Knee OA | Total Hospital discharges for OA | |
|---|---|---|---|
| 2006 | 84,583 | 71,703 | 156,286 |
| 2007 | 86,562 | 76,127 | 162,689 |
| 2008 | 88,656 | 78,304 | 166,960 |
| 2009 | 90,735 | 81,288 | 172,023 |
| 2010 | 92,759 | 84,22 | 176,979 |
| 2011 | 96,831 | 89,354 | 186,185 |
| 2012 | 97,654 | 92,902 | 190,556 |
| 2013 | 99,791 | 96,619 | 196,410 |
| 2014 | 103,236 | 103,334 | 206,570 |
Table 1. Number of hospital discharges for OA-France (Source Eurostat).
In western countries the rise of OA prevalence is leading to an increase in the number of total joint arthroplasty, which can be considered as the final stage of OA (knee and hip OA) [11,12]. In a study on Total Knee Replacement (TKR) incidence, the annual growth varies by country, from the 17% and 14% of Portugal and Switzerland to the 7% of Germany. In France the compound annual growth of TKR was estimated around 5.3% [13].The burden of OA is correlated to a high economic impact in terms of both direct health-related costs and indirect [14-21]. A systematic review concludes that the social cost of OA could be between 0.25% and 0.50% of a country’s GDP [15,16]. In France, the study by Le Pen et al. estimated that healthcare costs (doctor visits, medicines, and hospitalizations) for patients with osteoarthritis account for around 1.7% of France’s total healthcare expenditure in 2002 [20].
Bertin et al. [21] provide a health economic update of the patient costs associated with hip or knee OA treated in the community and in Medical, Surgical and Obstetric care (MSO) and Post-Acute Care and rehabilitation (PAC) hospitals in France in 2010. The annual costs per community patient were € 715 and € 764 for hip and knee OA, respectively, including a cost to the healthcare system of € 425 and € 454, that is, an estimated € 3.5 billion (€ 2 billion to the healthcare system) for 4.6 million patients. Hospitalization engendered annual costs of € 9,797 per patient with hip OA and € 11,644 per patient with knee OA, that is, a total cost of € 1.955 billion for patients hospitalized for hip or knee OA in 2010 [21].
The main direct health-related cost driver is the total joint arthroplasty [22]. The steady increasing, year after year, of surgery incidence leads costs to grow [22,23] in the future [11,12] . A possible strategy to adopt consists in slowing down the progression of the pathology in order to delay (or to avoid) the surgery [24-28].
Intra-articular therapies: Platelet-rich-plasma and hyaluronic acid
Intra-articular (IA) infiltration therapies are used after the failure of conservative treatments, between the pharmacological therapies and the surgery, in order to delay or to avoid the surgery [24-28]. Recently the scientific literature has shown the effectiveness of two IA therapies as Hyaluronic Acid (HA) and PRP.
It has been shown that an infiltration of HA in the joint can restore temporarily the patient’s health, giving him relief. Several clinical studies show the HA efficacy in knee OA treatment [29-32]. HA, compared to corticosteroids infiltrations, has a longer effect on pain, rigidity and movement in patient with knee OA [33].
HA has been used for several years and it is considered a standard intra-articular therapy in the treatment of knee OA. Hatoum et al. showed the cost-effectiveness of HA compared to oral NSAIDs (non-steroidal anti-inflammatory drugs), physical therapy and assistive device [34].
On the other side PRP is a non-transfusion use blood component, collected from the patient’s blood and used on the same patient [35,36]. The PRP treatment efficacy is shown in several studies [36-42]. PRP injections seem more effective in the treatment of knee OA over HA, in terms of pain relief and self-reported function improvement at 3, 6 and 12 months [36,43- 50]. The results are confirmed by several meta-analyses [51-58].
The method to produce PRP needs a medical device leading the therapy to be more costly than the comparator (HA). It is a typical situation where a technology has better effectiveness but on the other hand higher costs. In these cases it is important to run an economic evaluation to understand the relative cost-effectiveness. Health economic evaluation can be defined as a comparative analysis of alternative courses of actions in terms of both their costs and consequences in order to support policy decisions. The goal of economic evaluation is to inform decision makers to choose activities where benefits outweigh opportunity costs.
The objective of the present study is to assess the cost-effectiveness of the i.a. PRP therapy with respect to HA, in France, for patients with mild-moderate to severe knee pain due to OA and who failed to respond to conventional therapy, usually represented by corticosteroids.
Materials and methods
Study design
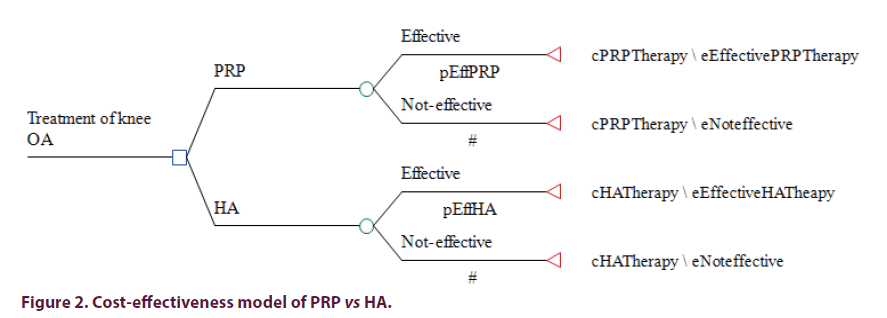
A decision tree model that evaluates the choice between PRP and HA for OA knee disease has been developed, considering costs and clinical benefits of both therapies. The decision tree is one of the models used in decisional analysis to perform economic evaluations. In the model are represented two or more strategic choices, defined by the initial branches which depart from the main node. Each branch represents one of the possible paths that could be undertaken while following a certain strategy. Each branch leads to a node, in which you find another event from which other branches depart up to a final outcome, represented by the leaf or terminal node. For each leaf node are associated the costs to bear during the path from root to leaf nodes and its outcome.
In this model the root node of the tree represents the choice between the two therapies (PRP and HA) for the knee OA treatment. From this choice depart several paths and treatments that the patient could be submitted at. For both the therapies the first node splits the path in two, according to the positive or negative response to the therapy. The development of the tree is represented in Figure 2.
Figure 2. Cost-effectiveness model of PRP vs HA.
The results are reported in terms of Incremental Cost-Effectiveness Ratio (ICER). The incremental cost-effectiveness ratio (ICER) is used to summarize the cost-effectiveness of a health care intervention. It is defined by the difference in cost between two possible interventions, divided by the difference in their effect. It represents the average incremental cost associated with one additional unit of the measure of effect. The outcomes values express the additional costs implied by the adoption of PRP to gain an additional life year in perfect health status. The French health system perspective was adopted to evaluate resources consumption. Only direct costs of the therapies were included. The time horizon considered in the model is one year. There are no robust clinic evidences considering a longer period.
Cost-effectiveness and willingness to pay threshold
The ICER is a value that reports the incremental cost for a gained point of a QALY gained, that it represents one year in perfect health. In Figure 3 are represented in a Cartesian plane all the possible results. In quadrant II the new technology dominates the standard of care, meaning that the new technology is more effective and more expensive. In quadrant III the new technology is dominated and not adopted. The quadrant I is the most common situation, where new technology is more effective and more costly, in this situation the adoption of the Incremental Cost Effectiveness Ratio and the use of WTP threshold will help to choose the best strategy. In France does not exist an official cost-effectiveness threshold to evaluate the costeffectiveness of a therapy. In this study we refer to two WTP levels, the standard one (30,000 €/ QALY) and the conservative (10,000€/QALY), but at the same time we report sensitivity analysis on different WTP thresholds.
Parameters of the model
Resources use and costs
The cost for the two i.a. therapies is affected both by the cost of the product/device used and by cost of the process with the medical professionals involved. In the analyses we inserted the cost of the product/device, the cost to perform the injections and the number of injections applied (Table 2).
| Direct costs (€) | ||||||
|---|---|---|---|---|---|---|
| Parameters | Base case value (€) | Range | Distrib. | Data source | ||
| Min | Max | |||||
| Medical Doctor/minute (€) | 0.74 | 0.5 | 1.3 | Log Normal | 30 juin 2016 JOURNAL OFFICIEL DE LA RÉPUBLIQUE FRANÇAISE (Texte 26 sur 196) - (Data refer to the 12ème échelon of hospital doctor) Min: (4ème echelon of hospital doctor)) Max: MD extra hospital with 80 €/hour tariff |
|
| Knee OA i.a. injection cost | 30.82 | 30.82 | 75.71 | Fractile | CCAM (classification commune des actes médicaux) CODE: NZJB001 Evacuation of the articular collection of the lower limb, by transcutaneous route without guidance o CODE: NZLB001: Therapeutic injection of pharmacological agent into a serous joint or bursa of the lower limb, transcutaneous without guidance Max and Fractile distribution: model the case where both the codes need to be applied. |
|
| PRP process additional costs for single injection (about 9 minutes) | 6.66 | 5.18 (7 minutes) |
9.62(13minutes) | - | Medical doctors opinion in France, Germany and Italy. | |
| RegenKit BCT-1 Cost (Market cost) |
65 | 52 | 78 | Gamma | Market price | |
| Base PRP therapeutic cycle cost (3 i.a. RegenKit BCT-1) |
307 | - | ||||
| HA Hyalgan | 29.59 | 23 | 35 | Gamma | Market price | |
| Base HA Hyalgan therapeutic cycle cost (3 3 i.a.) | 181 | - | ||||
| Effectiveness (QALY-Scenario 2, severe symptoms) | ||||||
| Parameters | Base case (QALY) | Range | Distrib. | References | ||
| Min | Max | |||||
| HA Therapy | 0.158 | 0.097 | 0.23 | Uniform | Duymus et al. 2016 Wailoo et al, 2014 |
|
| PRP Therapy | 0.365 | 0.187 | 0.535 | Uniform | Duymus et al. 2016 Wailoo et al, 2014 |
|
| Therapies not effective | 0.07 | 0.02 | 0.183 | Uniform | Duymus et al. 2016 Wailoo et al, 2014 |
|
| Effectiveness (Womac) | ||||||
| Parameters | Base case (WOMAC) | Range | Distrib. | References | ||
| Min | Max | |||||
| HA Therapy | 32 | 26 | 38 | Uniform | Duymus et al. 2016 | |
| PRP Therapy | 46 | 36 | 56 | Uniform | Duymus et al. 2016 | |
| Therapies not effective | 24 | 14 | 34 | Uniform | Duymus et al. 2016 | |
Table 2. Costs and effectiveness: Input parameters for the base case and ranges of the parameters for sensitivity analysis. Min and max values are the ones used in the deterministic sensitivity analyses. In the table are also reported the distribution used in probabilistic sensitivity analyses.
In particular PRP has a longer process (and higher costs) with respect to HA. Considering HA costs, the market price of Hyalgan product has been adopted to represent the cost of HA.
In addition, given the possible fluctuation of product market prices and also the use of different products a sensitive analyses has been carried out on this parameter.
As said PRP needs a medical device to be ‘produced’; the medical device taken as reference for this work is the Regen kit BCT-1©, manifactured by Regenlab (CH), is a simplified, sterile kit for PRP preparation that permits to separate plasma and platelets from other blood components obtaining a PRP ready to use. The cost of the PRP is calculated using the the market price of the Regenkit BCT-1. costs € 65 per i.a.
Besides the i.a. injection, the production of PRP implies several preparation steps (as previously described) and need longer times for elaboration, 11 minutes for PRP against 2 minutes for HA. These important differences in the delivery of the two therapies has been included in the model. The duration of the PRP preparation process was taken by interview to clinicians from different health structure in different countries. (Local Health Authorities (Unità Locale Socio Sanitaria, ULSS) of transfusional centres in Veneto region, Italy, Rhumatologie, Hopital de Meulan-Les Mureaux, France, and Klinik für Orthopädie und Unfallchirurgie UKSH Lübeck, University, Germany) (Table 2).
PRP preparation starts taking a blood sample from a patient’s vein (8 ml). Than patient’s blood is put in the BCT-1 kit tube that contains an anticoagulant able to prevent the activation of the platelets and a cell selector gel that permits separation of red cells from other blood components. The BCT-1 tube is then submitted to a centrifugation at a speed of 1500 g-force (3400 RPM), which enables to obtain three components: red blood cells trapped under the gel, Platelet-Poor-Plasma (PPP) and PRP settled on the surface of the gel. By gently inverting the BCT-1 tube several times, it is possible to suspend cellular deposit in the supernatant and obtain PRP (about 4 ml). Then PRP is ready for use, collected by a sterile syringe it is injected into the patient’s joint [39,59].
The HA treatment needs only the IA injection time, while the PRP treatment needs two minutes for the plasma withdrawal from the patient, around 7 minutes for the centrifugation and the other operations previously cited and finally 2 minutes for the injection that are in common for both therapies. Finally, the additional time to produce PRP with respect to HA is 9 minutes.
In order to include in the model the extra time due to produce PRP we multiply the cost per minute of a hospital doctor for the additional time. In this way we modeled the higher resource consumed for the PRP production process.
PRP production process costs count around 10% of the total therapeutic cycle cost. The data on the hospital doctor cost per minute was reported on the Journal Official de la Republique Francaise [60]. General costs were not inserted in the analysis because there is no significant difference and they do not change the results. The number of injections included for a PRP therapeutic cycle is 3, as reported in the most recent meta-analysis [51-54].
Clinical data sources and derivation of utility values
Studies on both therapies report effectiveness in terms of WOMAC scale (Western Ontario & Mc Master University Arthritis Index) that represents an illness specific measure of outcome widely adopted for lower extremity symptoms and function. Patients have to answer to a questionnaire assessing their status for three disease related domains: Pain, stiffness and functionality.
The scores are summed for items in each subscale, with possible ranges as follows: pain=0- 20, stiffness=0-8, physical function=0-68. Total scores can range from 0 to 96, with higher scores indicating increased pain and stiffness, and decreased physical function.
Illness specific scales are very sensitive to changes in patients’ conditions and they can be really accurate to evaluate improvement related to a certain treatment. On the other hand they are not useful to make comparison among treatments out of the context of a certain pathology and lacks of standard willingness to pay useful to compare the results of cost effectiveness analyses. The general health status profiles are less sensitive, but allow to analyze and compare results also out of the context of a certain disease. A variety of generic preference-based measures have been developed, the most commonly used questionnaires include the EuroQol (EQ)-5D5L, the Short Form 6D (SF-6D) and the Health Utilities Index (HUI). Once completed, the questionnaires generate a score using an algorithm based on values that have been obtained from a sample of the general public [61]. The values are the health-related quality of life (HRQoL) and measure the utility from living in a specific health state. Health states assume HRQoL values between 0 (dead) and 1 (perfect health), negative value are possible when the health status is considered worse than death. QALYs are assessed by combining the weights calculated for health states alongside the time spent in those health states. QALYs represent the number of years lived in perfect health. The advantage of its use is the possibility to compare results among pathologies and among willingness to pay thresholds for health outcome. Illness specific scales can be transformed in QALYs using mapping techniques. In this work WOMAC scores were transformed in QALYs using the conversion procedure of Wailoo [62] which it has been showed to be the best performer mapping algorithm in literature [63] and uses a mixture model derived from a study where patients states are both expressed in terms of WOMAC and EQ-5D5L. The model predict HRQoL using demographic variable, WOMAC pain, stiffness and function subscales.
In regard to the probability to respond at the two therapies, several studies show a response rate that ranges between 70% and 90% for both treatments [29,30,40,41]. For the base case scenario we chose to set the probability of clinical effectiveness at 80% for both of the therapies.
Sensitivity analysis
Deterministic and probabilistic sensitivity analysis have been conducted to assess the impact of the uncertainty of the parameters used in the model on the results. Deterministic Sensitivity Analysis (DSA) has been run for every min-max scenario of any parameters. In detail one way DSA have been run for every parameter where a min and max scenario is reported. Probabilistic Sensitivity Analysis (PSA) was performed through a Monte Carlo simulation, performing 10,000 scenarios, to assess the uncertainty around the ICER and the probability of the PRP therapy to be cost-effective at different willingness to pay thresholds. At each model input parameter was assigned a probability distribution (Table 2), that describe the different value the parameter can have with different probabilities [64]. For the parameters cited in literature where it was not estimated standard error, it was assumed a general standard error of 25% of the mean value [65].
Results
QALY
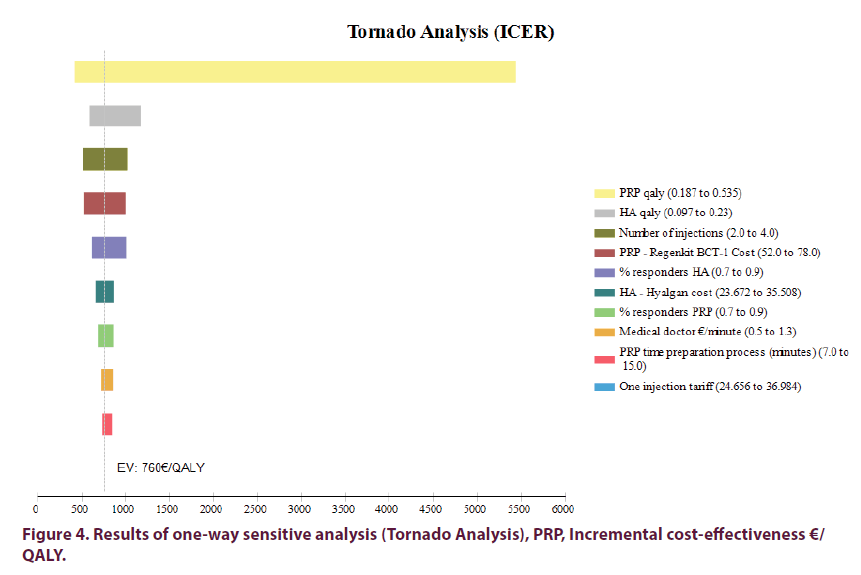
The base case of the scenario with more severe WOMAC scores confirms that none of these therapies dominates the other, but PRP results the cost-effective therapy. The average cost per QALY is respectively around € 761.5 for HA and € 761.7 for PRP. The incremental effectiveness of PRP is 0.166 QALY with an incremental cost of 126.21 €. The ICER of PRP introduction is €760/ QALY. In the tornado diagram (Figure 4) the deterministic sensitivity analysis was summarized. The most sensitive parameter is the effectiveness of the two therapies. In this case the PRP have a greater effectiveness (in fact in the base case the ICER is lower) but also have a greater variability because the clinic study used 49 report a higher standard deviation. However, no sensitivity analysis of the parameters changes the base case scenario result, that looks quite robust (considering the best-worst of the one way sensitivity analysis the ICER range from 500 to 5,500 €/QALY). The PRP does not become a cost saving therapy (dominant), even in the best case scenario, but in every scenarios it is the cost effective therapy (according to a € 10,000 WTP).
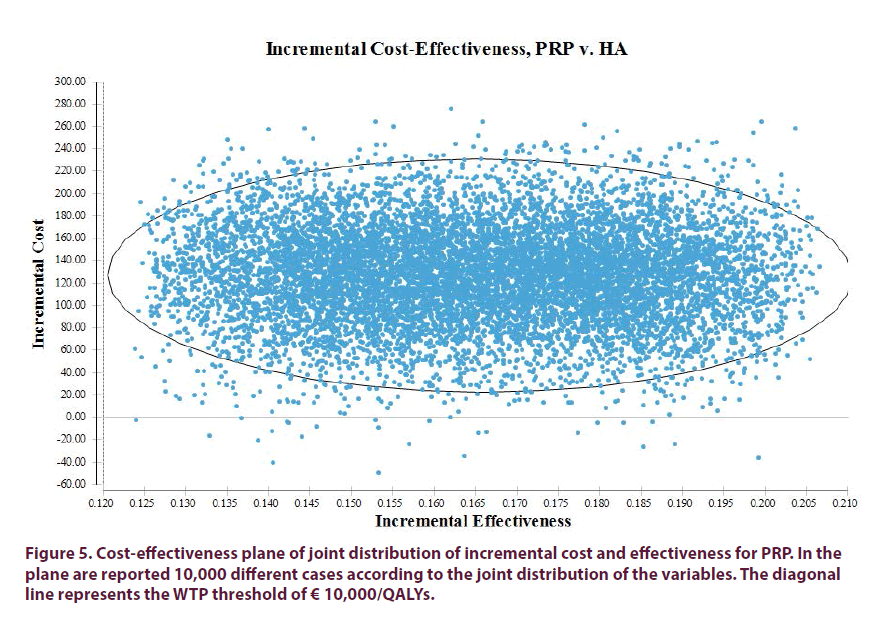
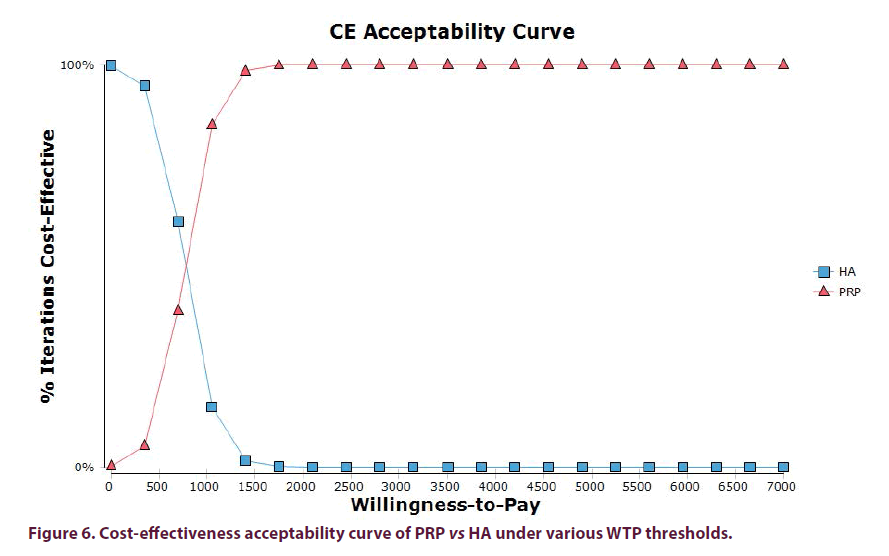
The Probabilistic Sensitivity Analysis (PSA) was performed through a Monte Carlo simulation considering 10,000 scenarios. All the parameters and variables of the model vary according to the assigned distribution. Establishing a WTP of €10,000 per QALY, the PRP is cost-effective in the 99% of the scenarios (Figure 5), while considering a WTP of €30,000 the PRP is costeffective in 100% of the iterations. In Figure 6 is reported the corresponding acceptability curve with the WTP threshold. For every WTP thresholds is indicated the percentage of cases in favor of PRP or HA.
Discussion
HA and PRP are two IA therapies used after the failure of conservative treatments and pharmacological therapies in order to delay or to avoid the surgery [24-26]. Recently the scientific literature has shown the effectiveness of two IA therapies as Hyaluronic Acid (HA) and PRP.
Several studies show that PRP is more effective than HA [36,43-58].
The rapid innovation in medicine leads to an increase in health outcomes, nowadays many incurable diseases are cured and the life expectancy is longer than few years ago. On the other hand new technologies in medicine are costly, impacting the health system sustainability. When deciding, all health care sectors and decision makers (public or private) are constrained by budgets.
Economic evaluation facilitates comparisons between health care programs. Economic evaluation is an important part of the health technology assessment (HTA). Usually a new technology has a better effectiveness but higher cost with respect to the standard of care. The goal of health economic evaluation, through the use of modelling, is to maximize the benefits from health care spending.
The method to produce PRP needs a medical device leading the therapy to be more costly than the comparator (HA). It is a typical situation where a technology has better effectiveness but on the other hand higher costs.
The goal of health economic evaluation, through the use of modelling, is to maximize the benefits from health care spending.
Up to date No economic analysis of PRP in the treatment of knee OA has previously been reported. The present study carried out a first economic evaluation to establish the economic value of this therapy for knee OA, in addition to evidence of safety and effectiveness. The specific objective of the study was to assess the cost-effectiveness of the i.a. PRP therapy with respect to HA, in France, for patients with mild-moderate to severe knee pain due to OA.
Results show that for patient with a mild to severe knee OA, considering a time horizon of 1 year in the French system context, PRP therapy is cost-effective with respect to HA. PRP production process implies additional costs that are outweighted by additional benefits in terms of pain relief. In French does not exist an official cost-effectiveness threshold for evaluating the cost-effectiveness of the therapy. In this study we refer to a conservative 10,000€/QALY WTP but at the same time we developed sensitivity analyses on the WTP thresholds. In fact we showed the cost effectiveness acceptability curves for every scenarios. In this way the decision makers can have a complete view. However even considering a conservative WTP threshold (€ 10,000.00/ QALY) PRP is cost-effective.
Some limitations of the present study should be taken into account. First the reported cost-effectiveness ratio may be influenced in relation with the method used to convert WOMAC scores in QALYs and for this reason we mapped the QALY from two different studies. Second a chronic disease should be evaluated in a longer period of time. The lack of clinical evidences on longer-term follow up, than one year, does not allow to use a a long term model able to take into account the surgical intervention in the analysis. The economic impact of TKR in NHS is an important variable to take into account for the economic evaluation for the introduction of new therapies for knee OA. A more effective therapy can delay of some years TKR and this delay could lead to reduce the total OA economic impact on Healthcare Systems. Yet the definition of the structure of this study will be useful to extent the evaluation when data on longer follow ups will be collected.
Conclusion
In conclusion, despite the limits explained above, it is possible to state that the IA PRP-based therapy is cost-effective with regard to the IA HA considering a one year horizon. Future research should evaluates PRP effectiveness for a longer period, in particular with reference to the delay of TKR. The major effectiveness of PRP, in addition to quality-of-life improvement, could delay TKR and therefore reduce the total costs of the knee OA and the economic burden on Healthcare Systems.
Acknowledgement
This research was supported by University Cà Foscari, Venice (Italy).
References
- Litwic A, Dennison E, Cooper C. Epidemiology and burden of osteoarthritis. Br. Med. Bull. 105, 185–199 (2013).
- Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin. Geriatr. Med. 26(3), 355–369 (2010).
- Neogi T, Zhang Y. Epidemiology of osteoarthritis. Rheum. Dis. Clin. North. Am. 39(1), 1–19 (2013).
- Leskinen J, Eskelinen A, Huhtala H et al. The incidence of knee arthroplasty for primary osteoarthritis grows rapidly among baby boomers: a population-based study in Finland. Arthritis. Rheum. 64(2), 423–428 (2012).
- Pereira D, Peleteiro B, Araujo J et al. The effect of osteoarthritis definition on prevalence and incidence estimates: A systematic review. Osteoarthr. Cartil. 19, 1270–1285 (2011).
- Vos T, Flaxman AD, Naghavi M et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 380(9859), 2163–2196 (2012).
- http://apps.who.int/gho/data/node.main.DALYRATE?lang=en
- Murray CJ, Vos T, Lozano R et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 380(9859), 2197–223 (2012).
- Cross M, Smith E, Hoy D et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 73(7), 1323–1330 (2014).
- Guillemin F, Rat AC, Mazieres B et al. 3000 Osteoarthritis group, prevalence of symptomatic hip and knee osteoarthritis: a two-phase population-based survey. Osteoarthr. Cartil. 19(11), 1314–1322 (2011).
- Hiligsmann M, Cooper C, Arden N et al. Health economics in the field of osteoarthritis: an expert's consensus paper from the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). Semin. Arthritis. Rheum. 43(3), 303–313 (2013).
- Culliford D, Maskell J, Judge A et al. Future projections of total hip and knee arthroplasty in the UK: results from the UK Clinical Practice Research Datalink. Osteoarthr. Cartil. 23(4), 594–600 (2015).
- Kurtz SM, Ong KL, Lau E et al. International survey of primary and revision total knee replacement. Int. Orthop. 35(12), 1783–1789 (2011).
- March LM, Bachmeier CJ. Economics of osteoarthritis: A global perspective. Baillière's. Clin. Rheumatol. 11(4), 817–834 (1997).
- Puig-Junoy J, Ruiz Zamora A. Socio-economic costs of osteoarthritis: A systematic review of cost-of-illness studies. Semin. Arthritis. Rheum. 44(5), 531–541 (2015).
- Salmon JH, Rat AC, Sellam J et al. Economic impact of lower-limb osteoarthritis worldwide: A systematic review of cost-of-illness studies. Osteoarthr. Cartil. (2016).
- Tarride JE, Haq M, Nakhai-Pour HR et al. The excess burden of rheumatoid arthritis in Ontario, Canada. Clin. Exp. Rheumatol. 31(1), 18–24 (2013).
- Hermans J, Koopmanschap MA, Bierma-Zeinstra SM et al. Productivity costs and medical costs among working patients with knee osteoarthritis. Arthritis. Care. Res. 64(6), 853–861 (2012).
- Leardini G, Salaffi F, Caporali R et al. Italian group for study of the costs of arthritis, direct and indirect costs of osteoarthritis of the knee. Clin. Exp. Rheumatol. 22(6), 699–706 (2004).
- Le Pen C, Reygrobellet C, Gérentes I. Financial cost of osteoarthritis in France. The “COART” Francestudy. Joint. Bone. Spine. 72, 567–570 (2005).
- Bertin P, Rannou F, Grange L et al. Annual cost of patients with osteoarthritis of the hip and knee in France. J. Musculoskelet. Pain. 22(4), 356e64 (2014).
- Chen A, Gupte C, Akhtar K et al. The global economic cost of osteoarthritis: how the UK compares. Arthiritis. 2012, 698–709 (2012).
- Piscitelli P, Iolascon G, Di tanna G et al. Socioeconomic burden of total joint arthroplasty for symptomatic hip and knee osteoarthritis in the Italian population: A 5-year analysis based on hospitalization records. Arthritis. Care. Res. 64(9), 1320–1327 (2012).
- Abbott T, Altman RD, Dimef R et al. Do hyaluronic acid injections delay total knee replacement surgery? Arthritis. Rheumatol. 65, S910–S911 (2013).
- Altman R, Lim S, Grant Steen R et al. Hyaluronic acid injections are associated with delay of total knee replacement surgery in patients with knee osteoarthritis: Evdence from a large U.S. Health claims database. (2015).
- Ong KL, Anderson AF, Niazi F et al. Hyaluronic acid injections in medicare knee osteoarthritis patients are associated with longer time to knee arthroplasty. J. Arthroplasty. 31(8), 1667–1673 (2016).
- Bruyere O, Cooper C, Pelletier JP et al. An algorithm recommendation for the management of knee osteoarthritis in Europe and internationally: A report from a task force of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). Semin. Arthritis. Rheum. 44(3), 253–263 (2014).
- Posnett J, Dixit S, Oppenheimer B et al. Patient preference and willingness to pay for knee osteoarthritis treatments. Patient. Prefer. Adherence. 9, 733–744 (2015).
- Conrozier T, Jerosch J, Beks P et al. Prospective, multi-centre, randomised evaluation of the safety and efficacy of five dosing regimens of viscosupplementation with hylan G-F 20 in patients with symptomatic tibio-femoral osteoarthritis: a pilot study. Arch. Orthop. Trauma. Surg. 129, 417–423 (2009).
- Navarro-Sarabia F, Collantes E, Navarro FJ et al. A 40-month multicenter, randomized placebo-controlled study to assess the efficacy and carry-over effect of repeated intra-articular injections of hyaluronic acid in knee osteoarthritis: The AMELIA project. Ann. Rheum. Dis. 70, 1957–1962 (2011).
- Altman RD, Rosen JE, Bloch DA et al. Safety and efficacy of retreatment with a bioengineered hyaluronate for painful osteoarthritis of the knee: results of the open-label Extension Study of the FLEXX Trial. Osteoarthr. Cartil. 19(10), 1169–1175 (2011).
- Pal S, Bansal H, Thuppal S et al. Long-term (1-year) safety and efficacy of a single 6-ml injection of hylgan G-F 20 in Indian Patients with symptomatic knee osteoarthritis. Open. Rheumatol. J. 8, 54–68 (2014).
- Askari A, Gholami T, NaghiZadeh MM et al. Hyaluronic acid compared with corticosteroid injections for the treatment of osteoarthritis of the knee: a randomized control trail. Springerplus. 12(5), 442 (2016).
- Hatoum HT, Fierlinger AL, Lin SJ et al. Cost-effectiveness analysis of intra-articular injections of high molecular weight bioengineered hyaluronic acid for the treatment of osteoarthritis knee pain. J. Med. Econ. 17(5), 326–337 (2014).
- Kon E, Filardo G, Delcogliano M et al. Platelet autologous growth factors decrease the osteochondral regeneration capability of acollagen- hydroxyapatite scaffold in a sheep model. BMC. Musculoskel. Dis. 11, 220 (2010).
- Sánchez M, Fiz N, Azofra J et al. Randomized clinical trial evaluating plasma rich in growth factors (PRGF-Endoret) versus hyaluronic acid in the short-term treatment of symptomatic knee osteoarthritis, Arthroscopy. J. Arthroscopic. Related. Surgery. 28(8), 1070–1078 (2012).
- Kon E, Buda R, Filardo G et al. Platelet-rich plasma: Intra-articular knee injections produced favorable results on degenerative cartilage lesions. Knee. Surg. Sports. Traumatol. Arthrosc. 18(4), 472–479 (2010).
- Sampson S, Reed M, Silvers H et al. Injection of platelet-rich-plasma in patients with primary and secondary knee osteoarthritis: A pilot study. Am. J. Phys. Med. Rehabil. 89(12), 961–969 (2010).
- Saad Setta H, Elshahat A, Elsherbiny K et al. Platelet-rich plasma versus platelet-poor plasma in the management of chronic diabetic foot ulcers: A comparative study. Int. Wound. J. 8(3), 307–312 (2011).
- Filardo G, Kon E, Buda R et al. Platelet-rich plasma intra-articular knee injections for the treatment of degenerative cartilage lesions and osteoarthritis, Knee Surgery, Sports Traumatology, Arthroscopy, 2011, 19(4):528-35.
- Wang-Saegusa A. Infiltration of plasma rich in growth factors for osteoarthritis of the knee short-term effects on function and quality of life. Arch. Orthop. Trauma. Surg. 131(3), 311–317 (2011).
- Mascarenhas R, Saltzman BM, Fortier LA et al. Role of platelet-rich plasma in articular cartilage injury and disease. J. Knee. Surg. 28, 3-10 (2015).
- Kon E, Mandelbaum B, Buda R et al. Platelet-rich plasma intra-articular injection versus hyaluronic acid viscosupplementation as treatments for cartilage pathology: From early degeneration to osteoarthritis, Arthroscopy. J. Arthroscopic. Related. Surgery. 27(11), 1490–1501 (2011).
- Filardo G, Kon E, Di Martino A et al. Platelet-rich plasma vs hyaluronic acid to treat knee degenerative pathology: Study design and preliminary results of a randomized controlled trial. BMC. Musculoskel. Dis. 13, 229 (2012).
- Spaková T, Rosocha J, Lacko M et al. Treatment of knee joint osteoarthritis with autologous platelet-rich plasma in comparison with hyaluronic acid. Am. J. Phys. Med. Rehabil. 91(5), 411–417 (2012).
- Cerza F, Carnì S, Carcangiu A et al. Comparison between hyaluronic acid and platelet-rich plasma, intra-articular infiltration in the treatment of gonarthrosis. Am. J. Sports. Med. 40(12), 2822–2827 (2012).
- Raeissadat SA, Rayegani SM, Hassanabadi H et al. Knee osteoarthritis injection choices: Platelet-rich plasma (prp) versus hyaluronic acid (a one-year randomized clinical trial). Clin. Med. Insights. Arthritis. Musculoskelet. Disord. 7(8), 1-8 (2015).
- Vaquerizo V, Placencia MA, Arribas I et al. Comparison of intra-articular injectionsof plasma rich in growth factors versus Durolane hyaluronic acid in the treatment of patients with symptomatic osteoarthritis: A randomized controlled trail. Arthroscopy. 29, 1635–1643 (2013).
- Duymus TM, Mutlu S, Dernek B et al. Choice of intra-articular injection in treatment of knee osteoarthritis: Platelet-rich plasma, hyaluronic acid or ozone options. Knee. Surg. Sports. Traumatol. Arthrosc. 25(2), 485–492 (2017).
- Cole BJ, Karas V, Hussey K et al. Hyaluronic acid versus platelet-rich plasma: A prospective, double-blind randomized controlled trial comparing clinical outcomes and effects on intra-articular biology for the treatment of knee osteoarthritis. Am. J. Sports. Med. 45(2), 339–346 (2017).
- Khoshbin A, Leroux T, Wasserstein D et al. The efficacy of platelet-rich plasma in the treatment of symptomatic knee osteoarthritis: a systematic review with quantitative synthesis. Arthroscopy. 29(12), 2037–2048 (2013).
- Chang KV, Hung CY, Aliwarga F et al. Comparative effectiveness of platelet-rich plasma injections for treating knee joint cartilage degenerative pathology: A systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 95(3), 562–575 (2014).
- Laudy ABM, Bakker EWP, Rekers M et al. Efficacy of platelet-rich plasma injections in osteoarthritis of the knee: a systematic review and meta-analysis. Br. J. Sports. Med. 49(10), 657–672 (2015).
- Campbell KA, Saltzman BM, Mascarenhas R et al. Does intra-articular platelet-rich plasma injection provide clinically superior outcomes compared with other therapies in the treatment of knee osteoarthritis? A systematic review of overlapping meta-analyses. Arthroscopy. 31(11), 2213–2221 (2015).
- Meheux CJ, McCulloch PC, Lintner DM et al. Efficacy of intra-articular platelet-rich plasma injections in knee osteoarthritis: A systematic review. Arthroscopy. 32(3), 495–505 (2016).
- Kanchanatawan W, Arirachakaran A, Chaijenkij K et al. Short-term outcomes of platelet-rich plasma injection for treatment of osteoarthritis of the knee. Knee. Surg. Sports. Traumatol. Arthrosc. 24(5), 1665–1677 (2016).
- Dai WL, Zhou AG, Zhang H et al. Efficacy of platelet-rich plasma in the treatment of knee osteoarthritis: A meta-analysis of randomized controlled trials. Arthroscopy. 33(3), 659–670 (2017).
- Shen L, Yuan T, Chen S et al. The temporal effect of platelet-rich plasma on pain and physical function in the treatment of knee osteoarthritis: systematic review and meta-analysis of randomized controlled trials. J. Orthop. Surg. Res. 12, 16 (2017).
- Sommeling CE, Heyneman A, Hoeksema H et al. The use of platelet-rich plasma in plastic surgery: A systematic review. J. Plast. Reconstr. Aesthet. Surg. 66(3), 301–311 (2013).
- https://catalogue.bnf.fr/ark:/12148/cb328020909.public
- Whitehead SJ, Ali S. Health outcomes in economic evaluation: The QALY and utilities. Br. Med. Bull. 96, 5–21 (2010).
- Wailoo A, Alava MA, Martinez AE. Modelling the relationship between the WOMAC osteoarthritis index and EQ-5D. Health. Qual. Life. Outcomes. 12, 37 (2014).
- Kiadaliri A, Englund M. Assessing the external validity of algorithms to estimate EQ-5D-3L from the WOMAC. Health. Qual. Life. Outcomes. 14, 141 (2016).
- Briggs AH, Goeree R, Blackhouse G et al. Probabilistic analysis of cost-effectiveness models: Choosing between treatment strategies for gastroesophageal reflux disease. Med. Decis. Making. 22(4), 290–308 (2002).
- Briggs AH, Sculpher MJ, Claxton K. Decision modelling for health economic evaluation. Oxford: Oxford University Press. (2006).