Research Article - Clinical Practice (2021) Volume 18, Issue 4
Irritable bowel syndrome, urolithiasis and role of microbiota in their comorbidity
- Corresponding Author:
- OА Kyrian Department of Family Medicine and Therapy Ukrainian Medical Stomatological Academy, Ukraine E-mail: hel_kirjan@i.ua
Abstract
Urolithiasis (UL) is a polyetiological disease that depends on climate, age, diet, infections, and the presence of concomitant diseases. The major risk factors for UL include inflammatory and functional bowel disease. The aim was analysis of changes in the bowel microbiota in patients with UL combined with Irritable Bowel Syndrome (IBS), as well as the effect of microbiome correction on the recurrence rates of oxalate UL in these patients. Material and Methods: We selected 320 patients with UL with oxalate stones and concomitant IBS. Small Intestinal Bacterial Overgrowth (SIBO) was assessed in all patients and microbiome analisis was performed. Patients has 3 year observation period. A breath test for SIBO was performed every 6 months. The determination of various taxa of fecal microbiota was carried out. Patients with UL+IBS were randomly divided into 2 groups. Group I involved 120 patients who were prescribed with rifaximin. Group II-control, involved 200 patients. Results: Initially, in patients with UL+IBS, the incidence of SIBO detection was 65%. The study of microbiome phylotypes has found the significant decrease in Firmicutes as well as Akkermansia muciniphila in patients with IBS-related oxalate UL. After 6 months SIBO in patients of Group I was positive in 54 (46.6%) patients, but following 3 years 15 (12.9%) patients. In Group II, following 6 months there were 123 (63.7%) patients with SIBO, following 3 years 149 (77.2%) patients. And after 3 years we found a significant decrease in the relative risk of recurrence of UL to 0.608 in Group I. Conclusions: Patients with UL have symptoms of IBS in 19.5% of cases. SIBO was diagnosed by 5.2 times more often in UL combined with IBS. Repeated courses of rifaximin, every 6 months, in patients with SIBO and persistent symptoms of IBS were accompanied by a significant decrease in recurrences of UL
Keywords
irritable bowel syndrome, urolithiasis, bowel microbiota, rifaximin, comorbidity
Introduction
Urolithiasis, also known as Kidney Stone Disease (KSD), along with other metabolic diseases, affects more and more people worldwide. Currently, almost 15% of the adult population has kidney stones, and over the past 50 years, the number of such patients has quadrupled [1]. Urolithiasis is a chronic disease with a 50% risk for relapse within 5 years after the first attack [2]. Our country is no exception, and about 60,000 people are diagnosed with KSD annually. In Ukraine, as in most other countries, kidney stones are most often formed from oxalate (up to 80%). It is well known that urolithiasis is a polyetiological disease that depends on climate, age, gender, genetic predisposition, diet, infections, and the presence of concomitant diseases (diabetes mellitus, obesity, arterial hypertension). Moreover, the chemical composition of kidney stones depends on the combination of risk factors [1,2].
The major risk factors for KSD include inflammatory and functional bowel disease [3]. One-third of patients with urolithiasis are diagnosed with Irritable Bowel Syndrome (IBS), which is almost three-fold higher than in the general population [4,5]. We have found that Post-Infectious Irritable Bowel Syndrome (PIIBS) is associated with KSD in more than 40% of cases. In PI-IBS, altered composition of the microflora in the small and large intestine is observed, and the use of rifaximin reduces the severity of dysbiosis and intestinal symptoms [6]. Currently, much attention is paid to the study of the role of the microflora in the pathogenesis of KSD, and the intestinal microbiota is more important than that of the urinary tract [7]. One of the first microorganisms found to reduce the risk for KSD development was Oxalobacter formigene, which is able to destroy oxalates in the intestinal lumen and reduce their absorption [8]. However, further studies have not confirmed the outstanding significance of this bacterium in the pathogenesis and treatment of urolithiasis [9,10]. Therefore, more attention is now being paid to the study of changes in the number of other species of the intestinal microbiota. In KSD patients, an increase in Bacteroides was found with a decrease in Prevotella, Enterobacter, Dorea, Faecalibacterium, Lactobacillus, Akkermansia muciniphila and Faecalibacterium prausnitzii, i.e. there is a decrease in the microorganisms capable of destroying oxalates and an increase in those that cause inflammation [7,8,10,11]. At the same time, the Indian study has found an increase in the number of Firmicutes and a decrease in Bacteroides in patients with recurrent oxalate urolithiasis, which may be related to the specifics of the Indian diet [12,13].
If the treatment of clinically manifested KSD is primarily a minimally invasive urological intervention, then the problem of preventing recurrences requires further development and differentiated approach. Currently, dietary correction of nutrition is crucial in prevention of urolithiasis [14]. However, any modification of the diet leads to altered composition of the intestinal microbiota [13]. In case of KSD, the use of probiotics as a method of changing the composition of the intestinal microflora is also being studied, though they have not been proven to be effective to date. The use of fecal microbiota transplantation from healthy donors in order to prevent recurrence of KSD seems to be promising [7]. At the same time, the use of conventional antibiotics increases the risk of urolithiasis [15]. At the same time, the nonabsorbable intestinal antibiotic rifaximin reduces the severity of dysbiosis, has a probiotic effect on the intestinal microbiota and eliminates the IBS symptoms [6,16]. Potentially, such an effect on the microflora can also have an impact on the course of urolithiasis, but no data on the effect of rifaximin on the recurrence rates of KSD in patients with IBS has been found in the literature. Based on our positive experience with the use of rifaximin in the treatment of IBS, we decided to evaluate its effect on the recurrence rates of KSD in patients with concomitant bowel pathology.
Aim
The present paper was aimed at the study of changes in the intestinal microbiota in patients with KSD combined with IBS, as well as the effect of bowel microbiome correction on the recurrence rates of oxalate urolithiasis in these patients.
Material and Methods
1951 out of 9986 patients with KSD in the Urology Unit showed symptoms of IBS. The patients were initially admitted to the Endourology Unit with the episodes of renal colic. The diagnosis of KSD was made on the basis of the plain excretory urography and sonography, and, if necessary, was confirmed by the spiral computed tomography. Different approaches have been used for the treatment of urolithiasis, depending on the localization of concrements. When the concrements were detected in the kidney and/or the upper third of the ureter, percutaneous nephrolithotripsy with antegrade ureterolithotripsy was used, and if localized in its middle or lower third, retrograde contact ureterolithotripsy or ureterolithotomy was used. In the Unit, in addition to surgical treatment, patients received analgesics (diclofenac, dexketoprofen) and uroseptics (nitrofurans). Patients with active urinary tract infection, kidney and urinary tract abnormalities, severe chronic renal failure (IIIIV) and a single kidney were not involved in the study. The chemical composition of urinary stones was studied spectrophotometrically in all patients. IBS was diagnosed based on the Rome IV criteria [17]. Oxalate stones were found in 54% of patients with KSD combined with IBS.
We selected 320 patients with unilateral solitary oxalate stones and concomitant IBS, who were treated during the period of 2015-2017. Among them were 131 men and 189 women, average age 47.4 ± 2.1 years. According to the chemical composition, the stones were distributed as follows: oxalate stones in 158 patients, and mixed oxalate-phosphate stones (oxalates more than 50%) in 162 patients. Initially (before discharge from the urological hospital), SIBO was assessed in all patients and feces were taken for subsequent PCR. Throughout the observation period, in the event of renal colic, the patients were advised to contact the Unit or inform the physician by phone. Within the first year, every 3 months, and then every 6 months, during control visits, all patients underwent kidney and urinary tract ultrasound to assess stone formation and contrast radiography, if necessary. A breath test for SIBO was performed every 6 months. Following 3 years, all patients underwent sonography to detect stone recurrence and the hydrogen breath test for SIBO. The recurrence rates of KSD was assessed on the basis of the findings of sonography, as well as the discharges from the hospital for the period of 3 years with confirmed urolithiasis or complaints of the episodes of renal colic with discharge of concrements. To determine the major types of fecal microbiota, Polymerase Chain Reaction (PCR) was initially performed on 108 randomly selected patients. At discharge from the hospital, all patients were advised to adhere to a diet that included adequate hydration of at least 2 L/day, calcium intake >1 g/day, and limiting intake oxalates, salt and proteins. At each visit, the patients were reminded of the importance of keeping to a diet. as the control group, to assess the intestinal microbiota, 40 healthy representatives of the Ukrainian population have been examined.
The chemical composition of the removed stones was studied using a UR-20 apparatus (Carl Zeiss, Jena, Germany) in the KBr matrix (potassium, bromine) in the frequency range 4000 cm-1-400 cm-1 by determining the number, position and intensity of absorption bands in the infrared spectra of the studied samples. Changes in the small intestinal microbiota (bacterial overgrowth syndrome-SIBO) were determined using a hydrogen breath test by the “Micro H2” apparatus (Micro, UK). Lactulose was used as a substrate. The quantitative determination of various taxa of fecal microbiota by the qPCR method was carried out using primers targeting the 16S rRNA gene specific for Firmicutes, Actinobacteria, Bacteroidetes Akkermansia muciniphila, and Faecalibacterium prausnitzi, as well as universal primers. The quantity and quality of DNA was measured with NanoDrop ND-8000 (Thermo Scientific, USA). Each patient placed the sample of fresh faeces a special container. Within 10 min after defecation, an aliquot of feces was taken, which was immediately frozen and stored at -20ºC prior the DNA extraction using the phenol-chloroform method according to the protocol. DNA was eluted in 200 μl of elution buffer. Genotyping was performed using polymerase chain reaction using the primer structure and temperature cycle parameters. Statistical analysis was carried out using the Office Excel 2016 (Microsoft Corporation, USA).
Patients with KSD combined with IBS were randomly divided into 2 groups. Group I involved 120 patients who were prescribed with rifaximin. A repeated course of rifaximin was prescribed after 6 months, and if SIBO and/or IBS symptoms persisted, then once the 6 months. The dose of rifaximin was 1200 mg/day for 14 days.
Group II involved 200 patients. The study was completed by 309 patients, who were selected for the final analysis. 4 and 7 patients had dropped out of Group I and Group II, respectively. The characteristics of patients are presented in TABLE 1.
TABLE 1. The characteristics of groups of patients.
| Group I (rifaximin) | Group II | p value | |||
|---|---|---|---|---|---|
| (controls) | |||||
| N=116 | % | N=193 | % | ||
| m/f | 45/71 | 39/61 | 91/102 | 47/53 | >0.05 |
| Age (years) | 45.2 | ± 2.9 | 49.8 | ± 2.7 | >0.05 |
| Oxalate | 61 | 52.6 | 88 | 45.6 | >0.05 |
| Oxalate-phosphate | 55 | 47.4 | 105 | 54.4 | >0.05 |
| Percutaneous nephrolitoripsia+antegrade ureterolithotripsy | 68 | 58.6 | 124 | 64.2 | >0.05 |
| Retrograde ureterolithotripsy/ureterolithotomy | 48 | 41.4 | 69 | 35.8 | >0.05 |
| IBS-D | 45 | 39.0 | 83 | 43.0 | >0.05 |
| IBS-C | 41 | 35.3 | 61 | 31.6 | >0.05 |
| IBS-M | 30 | 25.7 | 49 | 25.4 | >0.05 |
| SIBO (+) | 74 | 63.7 | 127 | 65.8 | >0.05 |
The resulting data show that, initially, the groups of patients did not differ significantly from each other. There were more women among the patients, which is more typical for IBS than for KSD. In terms of chemical composition, oxalate and mixed oxalate-phosphate stones were represented approximately equally. Among the methods of stone treatment, percutaneous nephrolithotripsy was used more often, which was associated with a large number of patients with concrements of the kidneys and the upper third of ureters. IBS-D was the most common variation of IBS in patients with urolithiasis.
Results
Initially, in patients with KSD+IBS, the incidence of SIBO detection was 65%, which is significantly higher compared to healthy people in the Ukrainian population (12.5% (p<0.001)): 74 patients (63.7%) from Group I, and 127 patients (65.8%) from Group II. The study of phylotypes of fecal microorganisms in patients with combined pathology has found the following features (TABLE 2).
TABLE 2. Phylotypes of fecal microorganisms in patients with KSD+IBS.
| Type of bacteria | Healthy subjects | KSD+IBS |
|---|---|---|
| (n=40) | (n=108) | |
| Firmicutes | 37.2 (29.0-43.5) | 28.8 (23.1-35.9)* |
| including Faecalibacterium prausnitzii | 8.4 (5.3-10.2) | 4.1 (2.4-7.9)* |
| Bacteroidetes | 40.5 (30.2-46.7) | 42.6 (34.1-52.8) |
| Actinobacteria | 13.7 (8.8-17.1) | 19.5 (12.4-26.7)* |
| Akkermansia muciniphila | 1.9 (1.37-2.39) | 1.2 (0.8-2.0)* |
| Other | 6.7 (4.1-10.5) | 7.9 (3.9-11.8) |
| F/B | 0.9 (0.7-1.3) | 0.7 (0.5-0.9)* |
Note: medians and interquartile intervals are presented; *p <0.05 compared to healthy subjects.
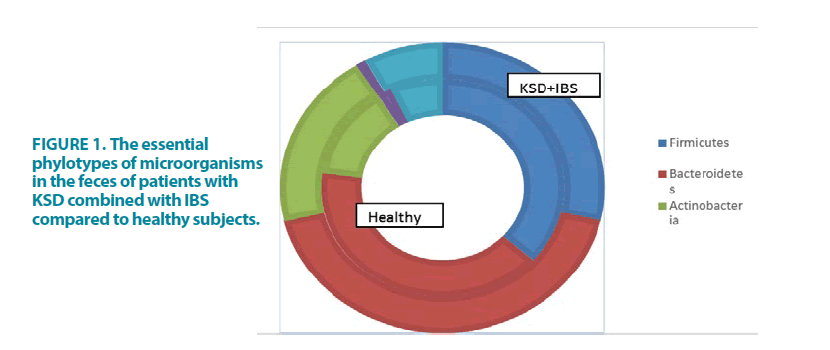
Notably, a significant decrease in Firmicutes and its representative Faecalibacterium prausnitzii, as well as one of the most significant protective microorganisms of the Verrucomicrobia-Akkermansia muciniphila phylotype and the Firmicutes/Bacteroidetes ratio was detected in patients with IBS-related oxalate urolithiasis, compared to otherwise healthy residents of Ukraine. At the same time, a significant increase in Actinobacteria and insignificant increase in Bacteroidetes and other non-differentiated microorganisms was observed. The resulting data are shown in FIGURE 1.
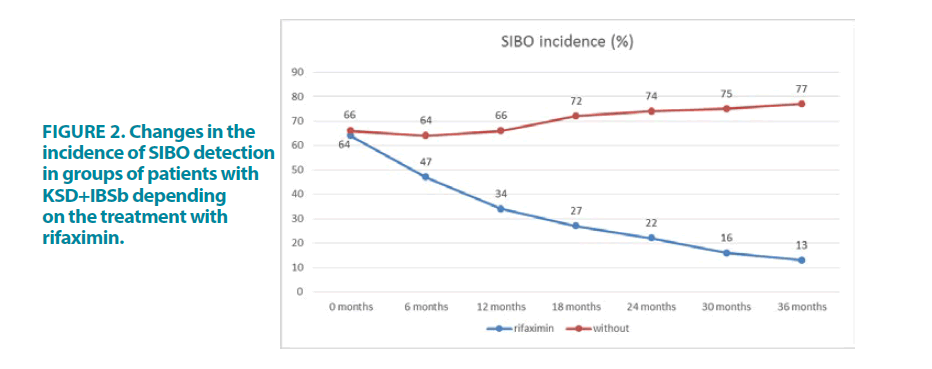
The analysis of the dynamics of SIBO in patients of Group I has shown that following 6 months after rifaximin therapy, the lactulose breath test was positive in 54 patients (46.6%). All patients with a positive SIBO test and persisting IBS symptoms received a repeated course of rifaximin. Following 12 months from the beginning of observation, a positive SIBO test was determined in 39 patients (33.6%). Following 18 months there were 31 patients (26.7%), following 24 months there were 25 patients (21.6%), following 30 months 19 patients (16.4%), and following 3 years 15 patients (12.9%). In a total of 348 patient-years of the follow-up period, patients in this group received 368 courses of rifaximin therapy (242 with a positive SIBO and 126 in connection with persisting IBS symptoms). On the average, the patient received 1.07 course of rifaximin therapy within a year.
In Group II, following 6 months there were 123 patients (63.7%) with a positive lactulose test, following 12 months 127 patients (65.8%), following 18 months 138 patients (71.5%), following 24 months 142 patients (73.6%), following 30 months 144 patients (74.6%), following 3 years 149 patients (77.2%).
The comparison of the dynamics of SIBO detection in two groups of patients with KSD+IBS are presented in FIGURE 2. The data show that following 6 months, in the group of patients taking rifaximin, a significantly lower incidence of SIBO is observed (p=0.005), which persisted for throughout the entire follow-up period.
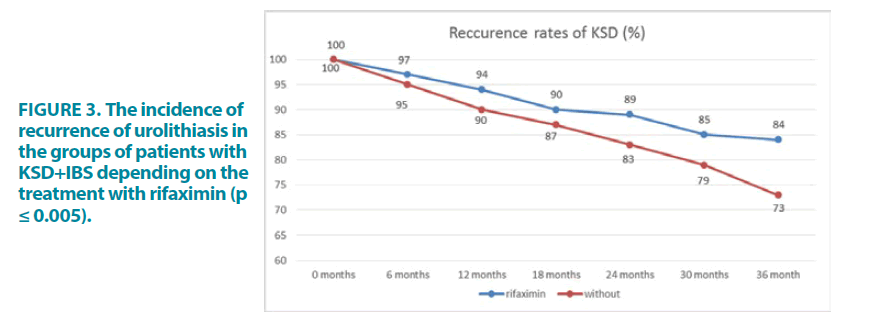
We also analyzed the recurrence rates of KSD in patients of the studied groups during the follow-up 3 years. In patients of Group I, 4 recurrences were observed following 6 months, 7 recurrences following 12 months, 11 recurrences following 18 months, 13 recurrences following 24 months, 17 recurrences following 30 months and 19 recurrences following 3 years. In patients of Group II, 9 recurrences were observed after 6 months, 19 recurrences after 12 months, 25 recurrences after 18 months, 33 recurrences after 24 months, 41 recurrences after 30 months and 52 recurrences after 3 years.
The dynamics of the increase in patients with recurrences of urolithiasis in the groups of patients is shown in Figure 3. Obviously, starting from the 6th month, the growth rate of patients with recurrences of KSD in the main group was lower. And after 3 years, in the rifaximin group, we found a significant decrease in the Relative Risk (RR) of recurrence of urolithiasis compared to patients who did not take rifaximin to 0.608 (CI 0.379-0.975, p=0.033). The Relative Risk Reduction (RRR) was 0.392, the number needed to treat (NNT)=9.466.
Discussion
The findings of our study have shown that in the Ukrainian population, almost 20% of KSD patients have symptoms of IBS, which is twice as often as in people without urolithiasis, and, admittedly, more than half of the stones consisted of oxalates. This can be explained by the general pathogenetic mechanisms that we previously considered [3,6]. In the studied population of IBS patients, the subjects more often complained of diarrhea, which, obviously, can lead to dehydration and changes in the volume and pH of urine. Another cause of stone formation in IBS may be an altered intestinal microbiota. Indicatively, in this category of patients SIBO was found in 65% of cases, that is by 5 times more often than in healthy people. However, altering the microbiota is not limited to the small intestine alone. The study of the fecal microflora by sequencing the 16S ribosomal RNA gene has found a change in the ratio of the essential phylotypes of microorganisms. Compared to healthy subjects, a significant decrease in Firmicutes, Faecalibacterium prausnitzii, Akkermansia muciniphila, and the Firmicutes/Bacteroidetes ratio was noted in the group of patients. These microorganisms have a protective effect on the intestine, are able to normalize the metabolic processes of the macroorganism and reduce the level of oxalates [7]. Moreover, in one of the recently published studies of intestinal microbiota in oxalate urolithiasis [11], a greater decrease in the content of Faecalibacterium prausnitzii and Akkermansia muciniphila, that are protective microorganisms in the formation of stones from calcium oxalate dihydrate, has been reported that is consistent with the findings of our study. We also found an increase in the number of microorganisms of the Actinobacteria phylotype, and its representative Bifidobacterium was considered as a potential destroyer of oxalates, while some other microorganisms of this phylotype are capable of provoking the formation of concrements [18,19]. The changes found in the small and large intestinal microflora in patients with KSD combined with IBS can be associated with both direct changes in the intestine that are typical of IBS, and with the more frequent use of uroseptics/antibiotics in this category of patients [20].
Since probiotics were not effective enough in the prevention of oxalate urolithiasis, we decided to study the effect of another method for modifying the composition of the intestinal microbiota and to use the nonabsorbable intestinal antibiotic rifaximin. In addition, unlike conventional antibiotics, which damage the intestinal microbiota and increase the risk for recurrence of KSD, rifaximin is eubiotic, which may reduce the risk of recurrence of urinary stones. The choice of the effective method was based on our experience of the positive effect of rifaximin on SIBO and the composition of the colonic microbiota in patients with IBS [6]. In addition to the positive effect on the intestinal microbiota (primarily a decrease in the members of the Clostridiaceae family), rifaximin reduces intestinal permeability and the level of proinflammatory cytokines [16]. Currently, rifaximin is mainly used for the treatment of IBS-D, however, in IBS-C, a decrease in symptoms is shown due to the normalization of the intestinal microbiota [21]. Therefore, we used rifaximin in all IBS patients, regardless of the subtype. The positive effect of rifaximin on SIBO in the studied group of patients was significant after the first course. The conduct of subsequent repeated courses, if necessary, in treatment with rifaximin enabled, after 3 years from the start of observation, to reduce the incidence of SIBO to 12.9% in the main group, compared to 77.2% in the comparison group.
No less significant was the effect of rifaximin on the recurrence rates of urolithiasis. Following 3 years, in the rifaximin group, 16.4% of patients experienced recurrence of KSD, compared to 26.9% of patients of the comparison group. The relative risk of recurrence of urolithiasis was 0.608; NNT=9.466. Apparently, such a positive effect of the nonabsorbable intestinal antibiotic rifaximin on the course of KSD is associated with its normalizing effect on the small intestinal microflora (elimination of SIBO shown by us) and altered colonic microbiota. Also, the normalization of intestinal permeability and a decrease in the production of the pro-inflammatory cytokines, described when taking rifaximin, may be important. It is known that these two factors also play a role in stone formation [1,6].
Conclusions
KSD patients have symptoms of IBS in 19.5% of cases. SIBO is diagnosed by 5.2 times more often in KSD combined with IBS, compared to healthy subjects. In the fecal microbiota of these patients, the amount of Actinobacteria is significantly increased and the amount of Firmicutes, Faecalibacterium prausnitzii, Akkermansia muciniphila and the Firmicutes/Bacteroidetes ratio is decreased, which can reduce the destruction of oxalates and increase the risk for KSD. The use of rifaximin at a dose of 1200 mg/day for 14 days led to a significant decrease in SIBO after the first course. Repeated courses of rifaximin, every 6 months, in patients with SIBO and persistent symptoms of IBS (on the average of 1.07 per year) were accompanied by a significant decrease in recurrences of KSD. Relative risk=0.608 (p=0.033); NNT=9.466.
References
- Khan SR, Pearle MS, Robertson WG, et al. Kidney stones. Nat Rev Dis Primers. 2: 16008 (2016).
- Ferraro PM, Taylor EN, Gambaro G, et al. Dietary and lifestyle risk factors associated with incident kidney stones in men and women. J Urol. 198: 858-863 (2017).
- Dorofeyev АЕ, Rudenko NN, Derkach IA, et al. Bowel and kidney diseases. Gastroenterologiya. 57: 101-105 (2015).
- Erdem E, Akbay E, Sezgin O, et al. Is there a relation between irritable bowel syndrome and urinary stone disease? Dig Dis Sci. 50: 605-608 (2005).
- Lei WY, Chang CY, Wu JH, et al. An initial attack of urinary stone disease is associated with an increased risk of developing new-onset irritable bowel syndrome: nationwide population-based study. PLoS One. 11: e0157701 (2016).
- Dorofeyev АЕ, Rudenko NN, Konovalova-Kushnir TA, et al. The role of rifaximin in the treatment of post-infectious irritable bowel syndrome. Suchasna hastroenterolohiia. 87: 105-109 (2016).
- Lee JA, Stern JM. Understanding the link between gut microbiome and urinary stone disease. Curr Urol Rep. 20: 19 (2019).
- Sadaf H, Raza SI, Hassan SW. Role of gut microbiota against calcium oxalate. Microb Pathog. 109: 287-291 (2017).
- Milliner D, Hoppe B, Groothoff J. A randomised Phase II/III study to evaluate the efficacy and safety of orally administered Oxalobacter formigenes to treat primary hyperoxaluria. Urolithiasis. 46: 313-323 (2018).
- Ticinesi A, Milani C, Guerra A, et al. Understanding the gut-kidney axis in nephrolithiasis: an analysis of the gut microbiota composition and functionality of stone formers. Gut. 67: 2097-2106 (2018).
- Millan Rodriguez F, Sabiote Rubio L, Giron Nanne I, et al. The relationship between calcium oxalate lithiasis and chronic proinflammatory intestinal dysbiosis pattern: a prospective study. Urolithiasis. 48: 321-328 (2020).
- Suryavanshi MV, Bhute SS, Jadhav SD, et al. Hyperoxaluria leads to dysbiosis and drives selective enrichment of oxalate metabolizing bacterial species in recurrent kidney stone endures. Sci Rep. 6: 34712 (2016).
- Ticinesi A, Nouvenne A, Chiussi G, et al. Calcium oxalate nephrolithiasis and gut microbiota: not just a gut-kidney axis-A nutritional perspective. Nutrients. 12: 548 (2020).
- Prezioso D, Strazzullo P, Lotti T, et al. Dietary treatment of urinary risk factors for renal stone formation. A review of CLU Working Group. Arch Ital Urol Androl. 87: 105-120 (2015).
- Ferraro PM, Curhan GC, Gambaro G, et al. Antibiotic use and risk of incident kidney stones in female nurses. Am J Kidney Dis. 74: 736-741 (2019).
- Chey WD, Shah ED, DuPont HL. Mechanism of action and therapeutic benefit of rifaximin in patients with irritable bowel syndrome: a narrative review. Therap Adv Gastroenterol. 13: 1756284819897531 (2020).
- Lacy BE, Mearin F, Chang L, et al. Bowel disorders. Gastroenterology. 18: S0016-5085 (2016).
- Ferraz RR, Marques NC, Froeder L, et al. Effects of lactobacillus casei and bifidobacterium breve on urinary oxalate excretion in nephrolithiasis patients. Urol Res. 37: 95-100 (2009).
- Bank S, Hansen TM, Soby KM, et al. Actinobaculum schaalii in urological patients, screened with real-time polymerase chain reaction. Scand J Urol Nephrol. 45: 406-410 (2011).
- Zampini A, Nguyen AH, Rose E, et al. Defining Dysbiosis in Patients with Urolithiasis. Sci Rep. 9: 5425 (2019).
- Ghoshal UC, Srivastava D, Misra A. A randomized double-blind placebo-controlled trial showing rifaximin to improve constipation by reducing methane production and accelerating colon transit: A pilot study. Indian J Gastroenterol. 37: 416-423 (2018).