Review Article - Interventional Cardiology (2013) Volume 5, Issue 4
Hybrid coronary revascularization: a mainstream revascularization strategy in the future?
- Corresponding Author:
- Leif Thuesen
Department of Medicine, Region Hospital, Herning, University of Aarhus, Skejby, Denmark
Tel: +45 2617 5575
Fax: +45 2617 5566
E-mail: leif.thuesen@ki.au.dk
Abstract
In stable patients with multivessel coronary artery disease (CAD), coronary bypass operation (coronary artery bypass grafting [CABG]) has been found to be superior to percutaneous coronary intervention (PCI) using drug-eluting stents (DES). The finding is based on wellpowered randomized studies and large-scale registries. The superiority of CABG is demonstrated by lower short- and long-term rates of repeat revascularization, myocardial infarction (MI) and death, which were pronounced in patients with complex coronary artery lesions. With equal consistency, short-term stroke rates have been found to be lower in PCI- than in CABG-treated patient.
Keywords
drug-eluting stent, Heart Team, hybrid coronary revascularization, hybrid revascularization, minimally invasive direct coronary artery bypass, minimally invasive surgery, off-pump coronary artery bypass surgery, percutaneous coronary intervention
In stable patients with multivessel coronary artery disease (CAD), coronary bypass operation (coronary artery bypass grafting [CABG]) has been found to be superior to percutaneous coronary intervention (PCI) using drug-eluting stents (DES) [1-3]. The finding is based on wellpowered randomized studies [4,5] and large-scale registries [6,7]. The superiority of CABG is demonstrated by lower short- and long-term rates of repeat revascularization, myocardial infarction (MI) and death, which were pronounced in patients with complex coronary artery lesions. With equal consistency, short-term stroke rates have been found to be lower in PCI- than in CABG-treated patients [4,5,8].
Coronary revascularization is a moving target. Coronary stents are undergoing continuous improvements resulting in enhanced deliverability and long-term safety as compared with the first-generation sirolimus-eluting Cypher™ (Cordis, FL, USA) and paclitaxel-eluting Taxus™ (Boston Scientific, MA, USA) stents used in the SYNTAX [5] and the FREEDOM [4] trials, respectively. Similarly, up-to-date antithrombotic treatment is likely to improve the short-term outcome of catheter-based revascularization [3].
On the surgical side, the combination of off-pump techniques and total arterial grafting promises a strategy to improve long-term outcome and reduce neurologic complications by avoidance of aortic manipulation [9-11]. In addition, minimally invasive techniques diminish the surgical trauma and bleeding [12,13]. These changes are not likely to change the overall results of the abovementioned landmark trials.
Substantial evidence indicates that left internal mammary artery (LIMA) grafting of the left anterior descending coronary artery (LAD) is the main determinant of the beneficial survival effect of CABG [14,15]. Therefore, current revascularization guidelines recommend CABG as the preferred treatment in patients with CAD with the exception of patients with one- or two-vessel disease without proximal LAD involvement [1-3]. The benefit of nonmammary artery conduits to non-LAD vessels is less clear, and the poor longevity, especially of saphenous vein grafts (SVG), may favor the use of PCI using DES in non-LAD territories [16,17]. The possible superiority of DES treatment as compared with grafting of non-LAD lesions using SVGs or arterial conduits remains to be addressed in randomized clinical trials.
The fundamental rationale of hybrid coronary revascularization (HCR) is to combine the prognostic benefits of the LIMA-to-LAD graft with minimal invasiveness and reduction of stroke risk. The concept of HCR has been assessed in a number of case reports and registry studies [18-30]. To date, HCR has mainly been used in patient subsets with a specific indication for a combined procedure, such as challenges including limited conduit availability and predicted reduced healing after sternotomy or following primary PCI of a non-LAD culprit lesion. Consecutive series with well-defined inclusion criteria are scarce, and randomized studies are nonexistent. This review (concurring with other recent scientific reports) advocates dedicated assessment of HCR procedures in prospective registries using predefined surgical and interventional techniques and in randomized controlled HCR versus traditional revascularization trials that are powered for clinical end points to prove the HCR concept [31-36].
The SY NTAX trial data and HCR
The SYNTAX trial is a unique comprehensive comparison of modern surgical and catheterbased revascularization using DES, incorporating coronary disease complexity into the evaluation of the clinical results [5,37]. The study offers a unique possibility to describe the characteristics and results of surgical and catheterbased revascularizations, and the likely results of combined procedures [38].
The SYNTAX trial demonstrated, for the first time, a dramatic negative effect of the complexity of CAD on PCI results using the SYNTAX score stratification [37]. After 5 years, compared with CABG, mortality was significantly increased in PCI patients with a high SYNTAX score [38]. Medium- and low-score patients had similar all-cause mortality in the PCI and CABG groups. PCI results were heavily dependent on the complexity of the CAD. In HCR, the LAD lesion can probably be omitted in the SYNTAX score calculation. In our own registry, including 100 consecutive patients treated with staged HCR, the SYNTAX score was reduced by half after omitting LAD lesions [33]. Therefore, even a highly complex general coronary pathology may be treated with a hybrid strategy with, in theory, low risk and favorable results. The surgical part of the revascularization, LIMA-to-LAD, is not influenced by lesion complexity and the stenting of non-LAD lesions may be performed in a low-SYNTAX score setting.
In the CABG treated patients, 5-year repeat revascularization rates were similar across the SYNTAX score groups, in contrast to the PCI group, where repeat revascularization increased from 23.0 in low to 30.9% in high SYNTAX score patients [38]. In the setting of HCR, the rate of repeat revascularization is likely to be acceptably low, owing to the lower SYNTAX score of the PCI-treated lesions. Furthermore, repeat revascularization using modern DES in non-LAD vessels is likely to remain stable at a low rate, including beyond 5–10 years, when SVG failure results in new revascularizations and other cardiac events [39].
As compared with PCI, there was a higher risk of periprocedural stroke in patients undergoing CABG. At 1‑year, 0.6% of PCI and 2.2% of CABG patients (p = 0.003) had suffered a stroke [5]. The risk converged over time and the difference was nonsignificant after 5 years (PCI 2.4 vs CABG 3.7%; p = 0.09) [38]. Of the patients who developed stroke, 68% in the CABG group and 47% in the PCI group had residual deficits [40]. Thus, stroke is a significant event often associated with severe disability. The increased risk of stroke after CABG is a major reason for considering surgical techniques that avoid any manipulation of the aorta [9].
Angiographic complete revascularization was achieved in 52.8% of the PCI patients and in 66.9% of patients treated with CABG [5]. Incomplete revascularization was associated with significantly increased 4‑year mortality in both groups. In the PCI group, the presence of a total occlusion was the strongest predictor of incomplete revascularization. It is likely that incomplete revascularization is a marker of greater coronary complexity and comorbidity that may explain some of the poor outcomes in incompletely revascularized patients [6,41]. A HCR procedure encompassing the options of both surgical and PCI may reduce the rates of incomplete revascularization, compared with conventional CABG and PCI.
LIMA versus DES
Long-term outcome is closely related to patency of grafts and PCI-treated lesions. In this respect, the LIMA is a unique conduit. After 10 years, >85% of LIMA grafts are patent and only 1% have developed atherosclerotic lesions with significant stenosis [42,43]. The superior patency of the LIMA graft versus PCI using bare-metal stents in the treatment of proximal LAD lesions has been demonstrated in two small randomized trials with 1-year follow-up [44,45]. There are no well-powered randomized comparisons of LIMA versus DES-PCI in the treatment of proximal LAD lesions. However, it is unlikely that catheter- based treatment will be able to match the long-term LIMA-to-LAD results in the proximal LAD. Following DES treatment of LAD lesions, a 5‑year rate of target vessel revascularization of 10–20% may be expected [46].
After the BARI trial comparing CABG and balloon angioplasty, it has been generally accepted that the survival advantage offered by CABG, compared with PCI was related to the presence of a patent LIMA-to-LAD graft [47]. Both the SYNTAX [5] and the FREEDOM [4] trials concur with these results, and the presence of a proximal LAD lesion in patients with multivessel disease strongly indicates a surgical revascularization. Accordingly, current revascularization guidelines recommend CABG as the primary treatment option in patients with CAD, with the exception of one- and two-vessel disease without proximal LAD involvement [1-3].
Non-LIMA grafting versus DES
The degeneration over time of the SVG is a major problem for the CABG patient. At 10 years, more than 50% of SVGs will be occluded [16]. Moreover, the revascularization of a SVG lesion or recanalization of its proximal coronary artery, which is often chronically occluded, may be challenging. Treatment of the degenerated SVG conveys a high risk of distal embolization and an increased risk of occlusion, restenosis and development of new lesions [41,48]. Aggressive statin treatment has been shown to reduce new revascularizations, and SVG disease progression can be assessed by angiography and intracoronary ultrasound [49,50]. The first-generation Cypher and Taxus stents have been used for almost 10 years, and the 5–10- year rates of target lesion revascularization seem to be approximately 10–20% [51,52]. Thus, it is likely that the long-term performance of the DES is superior to SVG. Ideally, this should be confirmed in a randomized study [30-39,46,53-55].
Bilateral internal mammary artery grafting
There are no long-term randomized comparisons of bilateral internal mammary artery (BIMA) versus CABG using SVG [56]. Large multivariate analyses and propensity score analyses document reduced mortality after BIMA, as compared with patients treated with LIMA and SVG grafting [56-58]. Despite the large number of patients in these studies and controlling for confounders, it must be taken into account that a large number of patients will never compensate for a stable, but unknown, selection bias. Using the BIMA, infection and instability have been of concern, especially in diabetic patients; the subgroup of patients that may need an arterial revascularization the most. The major reasons for not using BIMA grafts are the technical difficulty, the concern of higher periprocedural morbidity, including sternal infection, and the lack of definitive evidence of benefits [59].
Other arterial conduits
Owing to the frequently occurring degeneration of SVGs, arterial conduits are increasingly being used to improve long-term surgical revascularization results [60-63]. Radial, gastroepiploic and inferior epigastric arteries have been used. The problems faced using these arterial grafts include spasm and atrophy in the grafting of lesions that are not highly stenotic. Thus, the long-term patency of noninternal mammary arterial conduits may not be better than those of SVGs.
HCV procedure
▪ Surgical techniques
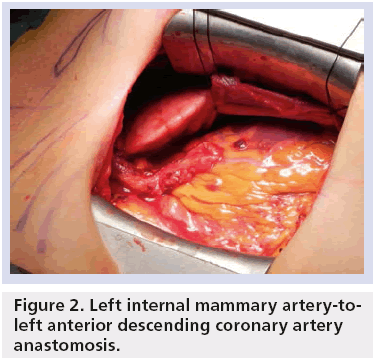
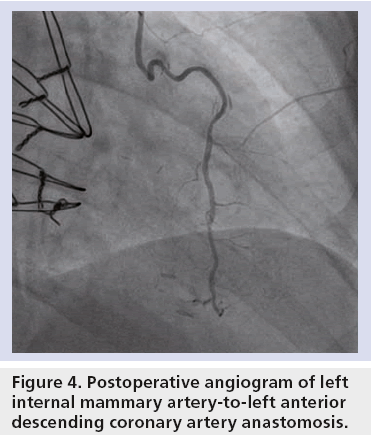
A number of minimally invasive techniques have been developed to anastomose the LIMA to the LAD. Minimally invasive direct CABG (MIDCAB) refers to LIMA harvest, with or without robotic assistance, and off-pump anastomosis under direct vision through a left-sided minithoracotomy [64,65]. In totally endoscopic coronary artery bypass surgery, both LIMA harvest and off-pump anastomosis are robotically assisted [66,67]. Finally, LIMA harvest and off-pump CABG (OPCAB) can be performed through an inferior left J-hemisternotomy under direct vision (a JOPCAB procedure) [25,33,68]. Figures 1–4 illustrate the minimally invasive character of the JOPCAB procedure. In a number of registries, with [12,69-77] or without [18-24,26-30] ad hoc control groups, these procedures have been demonstrated to be safe and efficient in dedicated centers.
Figure 4: Postoperative angiogram of left internal mammary artery-to-left anterior descending coronary artery anastomosis.
▪ Timing
Logistically, HCR may be performed in three ways. PCI can be performed prior to, or following, surgical intervention in a two-staged approach. Moreover, surgery and PCI can be performed in a single setting using a hybrid surgical suite.
The advantages of surgery prior to a PCI strategy include fewer bleeding problems, as dual antiplatelet therapy may be instituted after the surgical procedure. Furthermore, the operative LIMA result can be assessed angiographically and complex non-LAD lesion stenting may be performed with the LAD protected by the LIMA conduit. It is a disadvantage that surgery is performed in a scenario of significant untreated non-LAD lesions that may result in preoperative ischemia. Most problematic is the fact that a failed PCI may result in an incomplete revascularization. In our series of 100 preplanned staged HCRs, 89% of the procedures were carried out 1–3 days after the JOPCAB. We experienced three cases with ischemia without biomarker release due to untreated non-LAD lesions, and their PCI was performed before scheduled [33].
Advantages of a PCI prior to a surgery strategy include lower risks of ischemia during surgery and the possibility of performing grafting of non-LAD arteries in the case of suboptimal PCI results. In this strategy, bleeding complications constitute a significant problem, as the surgical part of the revascularization is performed during dual antiplatelet treatment. In addition, LIMA patency cannot be assessed routinely. The strategy may be used in lesions with a risk of PCI failure, in other words chronic total occlusions, and in partially revascularized patients after PCI for an acute coronary syndrome. In our series, 11% of patients were treated using this strategy and postoperative bleeding was found to be a concern [33].
Using a hybrid operation suite, surgery and subsequent PCI can be performed in the same setting. This simultaneous procedure is theoretically attractive as it is a single-step complete revascularization with immediate angiographic control of the LIMA-to-LAD revascularization and the option of surgical intervention in the case of PCI failure. The disadvantages include possible bleeding risk with dual antiplatelet therapy at the time of surgery and risk of stent thrombosis due to the general inflammatory response to surgery. Furthermore, there may be logistical issues and the need for a hybrid operation suite [12,69,73-76].
The Heart Team approach
In European and American guidelines for coronary revascularization, the multidisciplinary Heart Team approach has been considered a class I indication in coronary revascularization [1-3,78]. The SYNTAX trial documented the necessity for a preprocedure patient evaluation with participation of at least cardiac surgeons and interventional cardiologists to obtain a balanced and complementary approach to the treatment of the individual cardiac patient [5,37].
The Heart Team interaction is an essential element in the tailoring of a HCR procedure, and is mandatory for implementing a viable HCR program [33,79].
Clinical evaluation of HCR procedures
There have been numerous reports of successful HCR in patients with multivessel disease. The first procedures were described in the late 1990s, where the procedure was performed on special indications. For the surgeon, such scenarios include: patients without suitable conduits; a severely calcified aorta; conditions likely to prevent healing after sternotomy; or a nongraftable coronary vessel, where PCI remains an option. For the interventional cardiologist, severe tortuosity and calcification of the LAD or other complex lesion characteristics may call for a surgical procedure. Furthermore, patients with comorbidities, old age, frailty, poor left ventricular function or renal dysfunction are likely to benefit from a minimally invasive revascularization technique [19,24,26,28 ]. In these clinical situations, the American and European guidelines classify hybrid revascularizations as a class IIa, level of evidence C indication [1,2].
In the bare-metal stents era, the high restenosis rate after PCI was discouraging for the general use of HCR procedures. At present, the interest in HCR seems to be increasing, possibly owing to the proven failure of DES in patients with multivessel disease, and a genuine and relevant interest in minimally invasive revascularization techniques.
There are no randomized clinical trials on HCR versus surgical revascularization or PCI. A number of case reports and registries seem to document the feasibility of the HCR procedure across different HCR strategies (timing of PCI and surgical techniques). A number of the studies included patients over a long time period and, frequently, the HCR procedure was performed in patients who were suboptimal surgical candidates [19,24,25,28]. A recent study by Repossini et al. documented excellent long-term outcome after HCR with an intention-to-treat strategy in 166 patients [80].
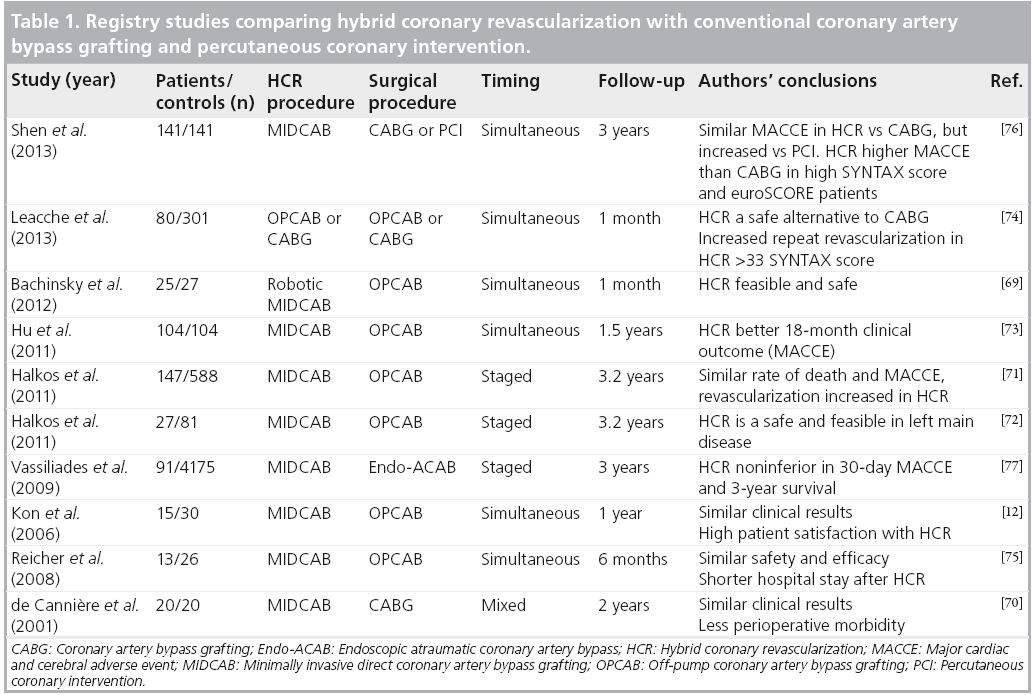
According to a PubMed search (6 May 2013), there are ten studies on HCR including a control group. These papers are mentioned in some detail in Table 1.
Table 1: Registry studies comparing hybrid coronary revascularization with conventional coronary artery bypass grafting and percutaneous coronary intervention.
In 2001, de Cannière et al. assessed HCR using bare-metal stents in 20 patients with twovessel coronary disease versus 20 matched (age, sex, comorbidities, coronary anatomy and ejection fraction) CABG patients [70]. The HCR was staged by 1–3 days. The HCR patients had a 2‑year event-free survival rate of 85%, compared with 35% in the CABG group (events included episodes of atrial fibrillation, pericardial effusion, MI, blood transfusion requirement and leg wound dehiscence). Compared with conventional surgery, recovery was more rapid after HCR, and patients returned to work much sooner after HCR than after CABG (22 ± 8 vs 89 ± 22 days; p < 0.005).
Reicher et al. used the propensity scores to match 13 patients undergoing simultaneous HCR with 26 off-pump CABG patients [75]. Overall, the results were similar in the two groups, but the HCR patients had shorter hospital stays (3.6 ± 1.5 vs 6.3 ± 2.3 days; p = 0.0001) and a significantly lower need for blood transfusion.
In 2008, Kon et al. compared a simultaneous approach HCR procedure including MIDCAB in 15 patients with 30 OPCAB controls [12]. The HCR patients received 325 mg of aspirin before the procedure, heparin during surgery and 300 mg of clopidogrel on returning to the intensive care unit. The results were much in favor of the HCR procedure. Thus, HCR patients had better preoperative hemodynamics, needed fewer blood cell transfusions, had shorter intubation times, less postoperative increase of serum creatinine values and reduced postoperative costs. Maximum pain scores were higher after MIDCAB, but the duration of time needed for pain to completely resolve was shorter for HCR. Overall satisfaction scores were significantly higher after the hybrid procedure. At 1 year, there was no mortality in either group. Major cardiac adverse events were noted in 7 of HCR and in 23% of OPCAB patients (p = 0.05). Patients returned to work or normal activities more quickly after HCR. Long-term graft patency was assessed using computed tomography angiography and demonstrated one stent failure in the hybrid group, compared with seven SVG failures in the OPCAB group (p = 0.062).
Vassiliades et al. compared 91 HCR and 4175 OPCAB procedures, adjusting for confounding background variables [77]. Surgery in HCR involved MIDCAB with thoracoscopic LIMA harvest. The authors used a staged treatment strategy; 93.4% had surgery first and PCI on average 2.2 days later. The remaining patients had PCI first and LIMA grafting 2 months later, while still on clopidogrel. The major cardiac and cerebral adverse events (MACCE; death, MI, stroke and need for repeat intervention) rates were similar between the two study groups (1.1 in hybrid vs 3.0% in OPCAB; p = 0.48), and the 3‑year Kaplan–Meier survival estimates at 3 years were also similar.
Halkos et al. assessed a HCR procedure using a robotic technique in 147 patients that were compared with 588 OPCAB controls [71]. The prevailing surgical technique was MIDCAB with thoracoscopic LIMA harvest and, since 2009, totally endoscopic coronary artery bypass surgery. This is, so far, the largest HCR series published. Patients with non-LAD lesions unfavorable for PCI were excluded (long lesions, small vessels, bifurcations and chronic total occlusions). The vast majority of patients were treated with surgery first and stenting after 2–3 days. The few PCIfirst patients underwent surgery on clopidogrel treatment. The in-hospital MACCE rate (death, stroke and MI) were similar in the two groups. After a median 3.2‑year follow-up period, the need for repeat revascularization was increased in HCR patients (12.2 vs 3.7%; p < 0.001). Interestingly, this was primarily due to LIMA and LIMA/LAD problems. The estimated 5‑year survival rates were similar in the two groups (HCR: 86.8% and OPCAB: 84.3%; p = 0.61).
In 2011, the same group published results on HCR versus OPCAB revascularization of patients with left main stenosis [72]. A total of 27 HCR patients were matched with 81 OPCAB controls. Again, after 3.2 years, rates of MACCE were similar between groups, and there were more repeat revascularizations in HCR patients (7.4 vs 1.2%; p = 0.09). In all HCR cases, the LIMA-to-LAD anastomosis was performed first and the left main coronary artery stenting was performed 2–3 days later after angiographical documentation of a patent LIMA-to-LAD.
In a study from 2011, Hu et al. performed simultaneous HCR in 104 patients and compared 18‑month clinical results with a 1:1 matched OPCAB group [73]. HCR procedure implied a JOPCAB procedure in patients pretreated with low-dose aspirin. Unfractionated heparin was given at the beginning of the operation and was reversed after the graft procedure. Clopidogrel was administered via a nasogastric tube before stenting and the patient was reheparinized. The total HCR procedure required longer operation time compared with OPCAB, but the need for blood transfusion was reduced. After 18 months, MACCE-free survival in HCR-treated patients compared favorably with OPCAB (99.0 vs 90.4%; p = 0.03).
Bachinsky et al. prospectively evaluated a same-sitting robotic-assisted HCR in 25 patients and compared the results to 27 consecutive low-to-moderate risk OPCAB patients [69]. The anticoagulation and antithrombotic regimen was similar to that mentioned above. In this short-term study, overall major cardiac adverse event rates were similar between both groups. The postoperative need for blood transfusions was reduced and the length of hospital stay was shorter in the HCR group. However, owing to higher procedural costs, the HCR treatment was more expensive than conventional OPCAB. Importantly, the HCR patients had a faster return to work (5.3 vs 8.2 weeks; p = 0.01).
Leacche et al. retrospectively analyzed the 30‑day outcome of 381 consecutive CABG patients versus 80 HCR patients (simultaneous PCI and OPCAB/CABG) [74]. The procedure was not preplanned in 25% of the HCR patients. The authors stratified the patients in a 2 × 2 matrix according to low/high SYNTAX score and low/high euroSCORE. The main challenging finding of the study was that the composite end point (death from any cause, stroke, MI and low cardiac output syndrome) was marked as increased in the HCR group with high SYNTAX score and high euroSCORE owing to high mortality in the HCR patients.
Recently, Shen et al. published the most comprehensive evaluation of HCR to date [76]. The authors performed simultaneous HCR using the JOPCAB technique with an inferior partial sternotomy in 141 patients. The outcome was compared with 141 matched PCI and 141 CABG controls. The three patient groups were stratified by euroSCORE and SYNTAX score. The algorithm for anticoagulation and antithrombotic treatment was similar to that described by Hu et al. [73]. At 3‑year follow-up, actuarial survival in the HCR, CABG and PCI groups was 99.3, 97.2 and 96.5%, respectively (p = 0.344). Six patients in the HCR group, three patients in the CABG group and 18 patients in the PCI group underwent repeat revascularization (p = 0.001). There were two, nine and three neurologic events in the HCR, CABG and PCI patients, respectively (p = 0.083). The cumulative MACCE rate in the hybrid group (6.4%) was significantly lower than in the PCI group (22.7%; p < 0.001), but similar to the CABG group. In patients with a high euroSCORE, HCR was associated with a lower MACCE rate than CABG (p = 0.030) and PCI (p = 0.006). High SYNTAX score was associated with improved results in HCR versus PCI (p = 0.002), while the results were similar in the HCR and CABG groups (p = 0.362).
▪ Comments on the existing clinical evaluation of HCR
There are considerable scientific weaknesses in the abovementioned registries, and the results should be considered hypothesis-generating. Even the studies with the highest numbers of patients are likely to be grossly underpowered to detect differences in clinical events. In addition, the patient selection cannot always be considered consecutive and the inclusion criteria were not always well defined. Futhermore, the matched controls are unlikely to be sufficiently adjusted for selection bias. In short, HCR seems to be less traumatic than conventional CABG and the MACCE results are as good as CABG, at least at medium-term follow-up.
A number of questions need to be assessed in prospective registries with well-defined inclusion criteria. The long-term safety and efficacy issues of HCR versus CABG/PCI need to be addressed in larger scale randomized clinical trials, as already proposed by other groups [31,32,35,36,81]. In this context, the design and conduct of the trials will be difficult owing to the complex nature of the problem and the multitude of techniques used. Another practical problem is the need for long-term follow-up; 5–10 years to obtain a definitive evaluation.
Finally, HCR necessitates an extensive synergy between interventional cardiologists and cardiac surgeons and a general acceptance of MIDCAB/JOPCAB procedures in the surgical environment. Such cultural changes may be challenging.
Conclusion and future perspective
HCR is a promising treatment strategy that combines the survival benefits of a LIMA conduit to the LAD with DES treatment of non- LAD lesions in a minimally invasive procedure. Today, HCR is a treatment option in patient and lesion subsets not suitable for CABG and PCI [1,2].
Well-defined prospective registry studies and randomized clinical trials will be necessary to complement our understanding on the role of HCR coronary revascularization. HCR is likely to become an important element in a revascularization scenario encompassing PCI, conventional surgery and HCR procedures, taking coronary revascularization and the Heart Team approach to another level.
Financial and competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Executive summary
Background for hybrid coronary revascularization
▪ There are prognostic benefits of left internal mammary artery (LIMA)-to-anterior descending coronary artery (LAD):
– The risk of stroke will be reduce.
– The surgical treatments are minimally invasive procedures.
The SYNTAX trial data and hybrid coronary revascularization
▪ In hybrid coronary revascularization (HCR), LIMA-to-LAD is not influenced by lesion complexity.
▪ Stenting of non-LAD lesions may be performed in a low-SYNTAX score setting.
LIMA vs drug-eluting stents
▪ The long-term LIMA-to-LAD grafting results are probably superior to drug-eluting stent treatment.
Non-LIMA grafting versus DES
▪ The long-term performance of drug-eluting stent is probably superior to saphenous vein grafts.
The Heart Team approach
▪ The Heart Team interaction is an essential element in the tailoring of a HCR procedure, and is mandatory for implementing a viable HCR program.
Clinical evaluation of HCR procedures
▪ In registry studies, the procedure has been associated with faster recovery and clinical results that are comparable to conventional revascularization.
Future perspective
▪ HCR is a treatment option in patient and lesion subsets that are not suitable for coronary artery bypass grafting and percutaneous coronary intervention.
▪ Well-defined prospective registry studies and randomized clinical trials will be necessary to define the role of HCR coronary revascularization.
▪ HCR is likely to become an important option in coronary revascularization.
References
Papers of special note have been highlighted as:
▪ of interest
▪▪ of considerable interest
- Hillis LD, Smith PK, Anderson JL et al. 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery. A report of the American College of Cardiology Foundation/ American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, Society of Cardiovascular Anesthesiologists, and Society of Thoracic Surgeons. J. Am. Coll. Cardiol. 58(24), e123–e210 (2011).
- Kolh P, Wijns W, Danchin N et al. Guidelines on myocardial revascularization. Eur. J. Cardiothorac. Surg. 38(Suppl.), S1–S52 (2010).
- Wijns W, Kolh P, Danchin N et al. Guidelines on myocardial revascularization. Eur. Heart J. 31(20), 2501–2555 (2010).
- Farkouh ME, Domanski M, Sleeper LA et al. Strategies for multivessel revascularization in patients with diabetes. N. Engl. J. Med. 367(25), 2375–2384 (2012).
- Serruys PW, Morice MC, Kappetein AP et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N. Engl. J. Med. 360(10), 961–972 (2009).
- Hannan EL, Wu C, Walford G et al. Drug-eluting stents vs. coronary-artery bypass grafting in multivessel coronary disease. N. Engl. J. Med. 358(4), 331–341 (2008).
- Weintraub WS, Grau-Sepulveda MV, Weiss JM et al. Comparative effectiveness of revascularization strategies. N. Engl. J. Med. 366(16), 1467–1476 (2012).
- Lee MS, Bokhoor P, Park SJ et al. Unprotected left main coronary disease and ST-segment elevation myocardial infarction: a contemporary review and argument for percutaneous coronary intervention. JACC Cardiovasc. Interv. 3(8), 791–795 (2010).
- Emmert MY, Seifert B, Wilhelm M, Grunenfelder J, Falk V, Salzberg SP. Aortic no-touch technique makes the difference in off-pump coronary artery bypass grafting. J. Thorac. Cardiovasc. Surg. 142(6), 1499–1506 (2011).
- Lattouf OM, Thourani VH, Kilgo PD et al. Influence of on-pump versus off-pump techniques and completeness of revascularization on long-term survival after coronary artery bypass. Ann. Thorac. Surg. 86(3), 797–805 (2008).
- Puskas JD, Kilgo PD, Lattouf OM et al. Off-pump coronary bypass provides reduced mortality and morbidity and equivalent 10-year survival. Ann. Thorac. Surg. 86(4), 1139–1146 (2008).
- Kon ZN, Kwon MH, Collins MJ et al. Off-Pump coronary artery bypass leads to a regional hypercoagulable state not detectable using systemic markers. Innovations (Phila.) 1(5), 232–238 (2006).
- Vallely MP, Bannon PG, Bayfield MS, Hughes CF, Kritharides L. Quantitative and temporal differences in coagulation, fibrinolysis and platelet activation after on-pump and off-pump coronary artery bypass surgery. Heart Lung Circ. 18(2), 123–130 (2009).
- Cameron A, Davis KB, Green G, Schaff HV. Coronary bypass surgery with internalthoracic- artery grafts – effects on survival over a 15-year period. N. Engl. J. Med. 334(4), 216–219 (1996).
- Loop FD, Lytle BW, Cosgrove DM et al. Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N. Engl. J. Med. 314(1), 1–6 (1986).
- Goldman S, Zadina K, Moritz T et al. Long-term patency of saphenous vein and left internal mammary artery grafts after coronary artery bypass surgery: results from a Department of Veterans Affairs Cooperative Study. J. Am. Coll. Cardiol. 44(11), 2149–2156 (2004).
- Nwasokwa ON. Coronary artery bypass graft disease. Ann. Intern. Med. 123(7), 528–545 (1995).
- Davidavicius G, Van Praet F, Mansour S et al. Hybrid revascularization strategy: a pilot study on the association of robotically enhanced minimally invasive direct coronary artery bypass surgery and fractional-flowreserve- guided percutaneous coronary intervention. Circulation 112(9 Suppl.), I317–I322 (2005).
- Fedakar A, Tasar M, Rabus MB, Alsalehi S, Toker ME, Balkanay M. Hybrid coronary revascularization for the treatment of left main coronary artery disease in high-risk patients. Heart Surg. Forum 15(1), E51–E55 (2012).
- Gilard M, Bezon E, Cornily JC et al. Same-day combined percutaneous coronary intervention and coronary artery surgery. Cardiology 108(4), 363–367 (2007).
- Katz MR, Van Praet F, de Cannière D et al. Integrated coronary revascularization: percutaneous coronary intervention plus robotic totally endoscopic coronary artery bypass. Circulation 114(1 Suppl.), I473–I476 (2006).
- Kiaii B, McClure RS, Kostuk WJ et al. Concurrent robotic hybrid revascularization using an enhanced operative suite. Chest 128(6), 4046–4048 (2005).
- Lewis BS, Porat E, Halon DA et al. Same-day combined coronary angioplasty and minimally invasive coronary surgery. Am. J. Cardiol. 84(10), 1246–1247 (1999).
- Presbitero P, Nicolini F, Maiello L et al. ‘Hybrid’ percutaneous and surgical coronary revascularization: selection criteria from a single-center experience. Ital. Heart J. 2(5), 363–368 (2001).
- Riess FC, Schofer J, Kremer P et al. Beating heart operations including hybrid revascularization: initial experiences. Ann. Thorac. Surg. 66(3), 1076–1081 (1998).
- Riess FC, Bader R, Kremer P et al. Coronary hybrid revascularization from January 1997 to January 2001: a clinical follow-up. Ann. Thorac. Surg. 73(6), 1849–1855 (2002).
- Stahl KD, Boyd WD, Vassiliades TA, Karamanoukian HL. Hybrid robotic coronary artery surgery and angioplasty in multivessel coronary artery disease. Ann. Thorac. Surg. 74(4), S1358–S1362 (2002).
- Wittwer T, Cremer J, Klima U, Wahlers T, Haverich A. Myocardial ‘hybrid’ revascularization: intermediate results of an alternative approach to multivessel coronary artery disease. J. Thorac. Cardiovasc. Surg. 118(4), 766–767 (1999).
- Zenati M, Cohen HA, Griffith BP. Alternative approach to multivessel coronary disease with integrated coronary revascularization. J. Thorac. Cardiovasc. Surg. 117(3), 439–444 (1999).
- Zhao DX, Leacche M, Balaguer JM et al. Routine intraoperative completion angiography after coronary artery bypass grafting and 1-stop hybrid revascularization results from a fully integrated hybrid catheterization laboratory/operating room. J. Am. Coll. Cardiol. 53(3), 232–241 (2009).
- Friedrich GJ, Bonatti J. Hybrid coronary artery revascularization – review and update 2007. Heart Surg. Forum 10(4), E292–E296 (2007).
- Green KD, Lynch DR Jr, Chen TP, Zhao D. Combining PCI and CABG: the role of hybrid revascularization. Curr. Cardiol. Rep. 15(4), 351 (2013).
- Modrau IS, Nielsen PH, Bøtker HE et al. Procedural feasibility and early safety of hybrid coronary revascularization combining off-pump coronary surgery through J-hemisternotomy with percutaneous coronary intervention. EuroIntervention (2013) (In Press).
- Murphy GJ, Bryan AJ, Angelini GD. Hybrid coronary revascularization in the era of drug-eluting stents. Ann. Thorac. Surg. 78(5), 1861–1867 (2004).
- Umakanthan R, Leacche M, Gallion AH, Byrne JG. A comparison of hybrid coronary revascularization and off-pump coronary revascularization. Expert Rev. Cardiovasc. Ther. 11(4), 395–397 (2013).
- Wrigley BJ, Dubey G, Spyt T, Gershlick AH. Hybrid revascularisation in multivessel coronary artery disease: could a combination of CABG and PCI be the best option in selected patients? EuroIntervention 8(11), 1335–1341 (2013).
- Sianos G, Morel MA, Kappetein AP et al. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention 1(2), 219–227 (2005).
- Mohr FW, Morice MC, Kappetein AP et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet 381(9867), 629–638 (2013).
- Sarno G, Lagerqvist B, Frobert O et al. Lower risk of stent thrombosis and restenosis with unrestricted use of ‘new-generation’ drug-eluting stents: a report from the nationwide Swedish Coronary Angiography and Angioplasty Registry (SCAAR). Eur. Heart J. 33(5), 606–613 (2012).
- Mack MJ, Head SJ, Holmes DR Jr et al. Analysis of stroke occurring in the SYNTAX Trial comparing coronary arterybypass surgery and percutaneous coronary intervention in the treatment of complex coronary artery disease. JACC Cardiovasc. Interv. 6(4), 344–354 (2013).
- Bell MR, Gersh BJ, Schaff HV et al. Effect of completeness of revascularization on long-term outcome of patients with three-vessel disease undergoing coronary artery bypass surgery. A report from the Coronary Artery Surgery Study (CASS) Registry. Circulation 86(2), 446–457 (1992).
- Fitzgibbon GM, Kafka HP, Leach AJ, Keon WJ, Hooper GD, Burton JR. Coronary bypass graft fate and patient outcome: angiographic follow-up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. J. Am. Coll. Cardiol. 28(3), 616–626 (1996).
- Sabik JF 3rd, Lytle BW, Blackstone EH, Houghtaling PL, Cosgrove DM. Comparison of saphenous vein and internal thoracic artery graft patency by coronary system. Ann. Thorac. Surg. 79(2), 544–551 (2005).
- Diegeler A, Thiele H, Falk V et al. Comparison of stenting with minimally invasive bypass surgery for stenosis of the left anterior descending coronary artery. N. Engl. J. Med. 347(8), 561–566 (2002).
- Drenth DJ, Winter JB, Veeger NJ et al. Minimally invasive coronary artery bypass grafting versus percutaneous transluminal coronary angioplasty with stenting in isolated high-grade stenosis of the proximal left anterior descending coronary artery: six months’ angiographic and clinical followup of a prospective randomized study. J. Thorac. Cardiovasc. Surg. 124(1), 130–135 (2002).
- Stefanini GG, Kalesan B, Serruys PW et al. Long-term clinical outcomes of biodegradable polymer biolimus-eluting stents versus durable polymer sirolimus-eluting stents in patients with coronary artery disease (LEADERS): 4 year follow-up of a randomised non-inferiority trial. Lancet 378(9807), 1940–1948 (2011).
- BARI Investigators. The final 10-year follow-up results from the BARI randomized trial. J. Am. Coll. Cardiol. 49(15), 1600–1606 (2007).
- Keeley EC, Velez CA, O’Neill WW, Safian RD. Long-term clinical outcome and predictors of major adverse cardiac events after percutaneous interventions on saphenous vein grafts. J. Am. Coll. Cardiol. 38(3), 659–665 (2001).
- The effect of aggressive lowering of lowdensity lipoprotein cholesterol levels and lowdose anticoagulation on obstructive changes in saphevenous coronary-artery bypass grafts. The Post Coronary Artery Bypass Graft Trial Investigators. N. Engl. J. Med. 336, 153–162 (1997).
- Jensen LO, Thayssen P, Pedersen KE et al. Regression of coronary atherosclerosis by simvastatin: a serial intravascular ultrasound study. Circulation. 110(3), 265–270 (2004).
- Kimura T, Morimoto T, Nakagawa Y et al. Very late stent thrombosis and late target lesion revascularization after sirolimus-eluting stent implantation: five-year outcome of the j-Cypher Registry. Circulation 125(4), 584–591 (2012).
- Sousa JE, Costa JR Jr, Abizaid A. 10-year follow-up of the first Cypher stent implanted in human: an invasive evaluation with angiography, intravascular ultrasound, and optical coherence tomography. JACC Cardiovasc. Interv. 3(5), 556–558 (2010).
- Jensen LO, Thayssen P, Hansen HS et al. Randomized comparison of everolimuseluting and sirolimus-eluting stents in patients treated with percutaneous coronary intervention: the Scandinavian Organization for Randomized Trials with Clinical Outcome IV (SORT OUT IV). Circulation 125(10), 1246–1255 (2012).
- Capodanno D, Tamburino C. Unraveling the EXCEL: promises and challenges of the next trial of left main percutaneous coronary intervention. Int. J. Cardiol. 156(1), 1–3 (2012).
- Lagerqvist B, James SK, Stenestrand U, Lindback J, Nilsson T, Wallentin L. Long-term outcomes with drug-eluting stents versus bare-metal stents in Sweden. N. Engl. J. Med. 356(10), 1009–1019 (2007).
- Taggart DP, Altman DG, Gray AM et al. Randomized trial to compare bilateral vs. single internal mammary coronary artery bypass grafting: 1-year results of the Arterial Revascularisation Trial (ART). Eur. Heart J. 31(20), 2470–2481 (2010).
- Buxton BF, Ruengsakulrach P, Fuller J, Rosalion A, Reid CM, Tatoulis J. The right internal thoracic artery graft – benefits of grafting the left coronary system and native vessels with a high grade stenosis. Eur. J. Cardiothorac. Surg. 18(3), 255–261 (2000).
- Ioannidis JP, Galanos O, Katritsis D et al. Early mortality and morbidity of bilateral versus single internal thoracic artery revascularization: propensity and risk modeling. J. Am. Coll. Cardiol. 37(2), 521–528 (2001).
- Catarino PA, Black E, Taggart DP. Why do UK cardiac surgeons not perform their first choice operation for coronary artery bypass graft? Heart 88(6), 643–644 (2002).
- Acar C, Ramsheyi A, Pagny JY et al. The radial artery for coronary artery bypass grafting: clinical and angiographic results at five years. J. Thorac. Cardiovasc. Surg. 116(6), 981–989 (1998).
- Glineur D, D’hoore W, El Khoury G et al. Angiographic predictors of 6-month patency of bypass grafts implanted to the right coronary artery a prospective randomized comparison of gastroepiploic artery and saphenous vein grafts. J. Am. Coll. Cardiol. 51(2), 120–125 (2008).
- Moran SV, Baeza R, Guarda E et al. Predictors of radial artery patency for coronary bypass operations. Ann. Thorac. Surg. 72(5), 1552–1556 (2001).
- Suma H, Isomura T, Horii T, Sato T. Late angiographic result of using the right gastroepiploic artery as a graft. J. Thorac. Cardiovasc. Surg. 120(3), 496–498 (2000).
- Angelini GD, Wilde P, Salerno TA, Bosco G, Calafiore AM. Integrated left small thoracotomy and angioplasty for multivessel coronary artery revascularisation. Lancet 347(9003), 757–758 (1996).
- Repossini A, Moriggia S, Cianci V et al. The LAST operation is safe and effective: MIDCABG clinical and angiographic evaluation. Ann. Thorac. Surg. 70(1), 74–78 (2000).
- Bonaros N, Schachner T, Lehr E et al. Five hundred cases of robotic totally endoscopic coronary artery bypass grafting: predictors of success and safety. Ann. Thorac. Surg. 95(3), 803–812 (2013).
- Lee JD, Bonaros N, Hong PT et al. Factors influencing hospital length of stay after robotic totally endoscopic coronary artery bypass grafting. Ann. Thorac. Surg. 95(3), 813–818 (2013).
- Trehan N, Malhotra R, Mishra Y, Shrivastva S, Kohli V, Mehta Y. Comparison of ministernotomy with minithoracotomy regarding postoperative pain and internal mammary artery characteristics. Heart Surg. Forum 3(4), 300–306 (2000).
- Bachinsky WB, Abdelsalam M, Boga G, Kiljanek L, Mumtaz M, McCarty C. Comparative study of same sitting hybrid coronary artery revascularization versus off-pump coronary artery bypass in multivessel coronary artery disease. J. Interv. Cardiol. 25(5), 460–468 (2012).
- de Cannière D, Jansens JL, Goldschmidt- Clermont P, Barvais L, Decroly P, Stoupel E. Combination of minimally invasive coronary bypass and percutaneous transluminal coronary angioplasty in the treatment of double-vessel coronary disease: two-year follow-up of a new hybrid procedure compared with ‘on-pump’ double bypass grafting. Am. Heart J. 142(4), 563–570 (2001).
- Halkos ME, Vassiliades TA, Douglas JS et al. Hybrid coronary revascularization versus off-pump coronary artery bypass grafting for the treatment of multivessel coronary artery disease. Ann. Thorac. Surg. 92(5), 1695–1701 (2011).
- Halkos ME, Rab ST, Vassiliades TA et al. Hybrid coronary revascularization versus off-pump coronary artery bypass for the treatment of left main coronary stenosis. Ann. Thorac. Surg. 92(6), 2155–2160 (2011).
- Hu S, Li Q, Gao P et al. Simultaneous hybrid revascularization versus off-pump coronary artery bypass for multivessel coronary artery disease. Ann. Thorac. Surg. 91(2), 432–438 (2011).
- Leacche M, Byrne JG, Solenkova NS et al. Comparison of 30-day outcomes of coronary artery bypass grafting surgery verus hybrid coronary revascularization stratified by SYNTAX and euroSCORE. J. Thorac. Cardiovasc. Surg. 145(4), 1004–1012 (2013).
- Reicher B, Poston RS, Mehra MR et al. Simultaneous ‘hybrid’ percutaneous coronary intervention and minimally invasive surgical bypass grafting: feasibility, safety, and clinical outcomes. Am. Heart J. 155(4), 661–667 (2008).
- Shen L, Hu S, Wang H et al. One-Stop Hybrid coronary revascularization versus coronary artery bypass graft and percutaneous coronary intervention for the treatment of multivessel coronary artery disease: three-year follow-up results from a single institution. J. Am. Coll. Cardiol. 61(25), 2525–2533 (2013).
- Vassiliades TA, Kilgo PD, Douglas JS et al. Clinical outcomes after hybrid coronary revascularization versus off-pump coronary artery bypass: a prospective evaluation. Innovations (Phila) 4(6), 299–306 (2009).
- Patel MR, Dehmer GJ, Hirshfeld JW et al. ACCF/SCAI/STS/AATS/AHA/ASNC/HFSA/SCCT 2012 appropriate use criteria for coronary revascularization focused update: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, American Society of Nuclear Cardiology, and the Society of Cardiovascular Computed Tomography. J. Thorac. Cardiovasc. Surg. 143(4), 780–803 (2012).
- Holmes DR Jr, Rich JB, Zoghbi WA, Mack MJ. The heart team of cardiovascular care. J. Am. Coll. Cardiol. 61(9), 903–907 (2013).
- Repossini A, Tespili M, Saino A et al. Hybrid revascularization in multivessel coronary artery disease. Eur. J. Cardiothorac. Surg. doi:10.1093/ejcts/ezt016 (2013) (Epub ahead of print).
- Popma JJ, Nathan S, Hagberg RC, Khabbaz KR. Hybrid myocardial revascularization: an integrated approach to coronary revascularization. Catheter Cardiovasc. Interv. 1(75 Suppl. 1), S28–S34 (2010).
▪▪ The SYNTAX study, a comprehensive comparison of drug-eluting stent percutaneous coronary intervention versus coronary bypass operation.
▪ Description of the SYNTAX score.
▪▪ Nonrandomized comparison of hybrid coronary revascularization, coronary bypass operation and percutaneous coronary intervention.
▪▪ Description of the Heart Team approach.
▪▪ Registry of 166 patients treated with an intention-to-treat hybrid coronary revascularization strategy.