Case Report - International Journal of Clinical Rheumatology (2019) Volume 14, Issue 6
Diffuse alveolar hemorrhage as the presenting feature of an IgA vasculitis: An unusual presentation
- Corresponding Author:
- Aniqa Malik
Department of Internal Medicine
Easton Hospital, Easton, PA, USA
E-mail: aniqamalik@gmail.com
Abstract
IgA vasculitis is the most common form of systemic vasculitis in children, but only 10% of the cases occur in adults. It typically presents with symptoms of palpable purpura, arthralgia, abdominal pain and renal disease. Diffuse alveolar hemorrhage is a rare feature of IgA vasculitis, with only a small number of cases reported to date. We report the case of a 47-year-old female who presented with hemoptysis, shortness of breath, and fever, but without any abdominal or joint symptoms, and no purpura on physical examination. She also had hematuria and proteinuria, but normal kidney function otherwise. Chest imaging revealed patchy nodular consolidations in bilateral lungs, which raised concern for pneumonia or vasculitis. A bronchoscopy was subsequently done, revealing diffuse alveolar hemorrhage. Renal biopsy was then performed, with pathology yielding focal segmental and crescentic glomerulonephritis, consistent with IgA vasculitis. The patient was treated with intravenous methylprednisolone 1 g per a day for three days followed by tapering dose of oral prednisone, with complete improvement of her respiratory symptoms.
Keywords
IgA vasculitis • diffuse alveolar hemorrhage • hematuria
Introduction
IgA vasculitis, formerly called Henoch-Schönlein purpura, is an immune-mediated vasculitis characterized by deposition of IgA immune complexes in small vessels of affected organs. Clinically, the disease is classically characterized by a tetrad of arthritis/arthralgia, abdominal pain, renal disease, and palpable purpura in the absence of thrombocytopenia or coagulopathy. Rarely, patients may present with a paucity of symptoms or unusual features, which can make the diagnosis challenging [1-3].
Despite being significantly more common among children, the disease can also affect adults. When it affects adults, it usually tends to be more aggressive, and overtime it can progress to complications such as end stage renal failure in about a third of patients. Other significant finding that can be rarely observed is diffuse alveolar hemorrhage, which can lead to respiratory failure and potentially death [4-7].
We report the case of a patient with biopsy proven IgA vasculitis who presented with hemoptysis due to diffuse alveolar hemorrhage and hematuria, but no other classic clinical features such as purpura, arthritis, or gastrointestinal symptoms.
Case report
A 47-year-old Moroccan female presented to the Emergency Department with cough, shortness of breath, fever and malaise for 2 days. She also reported hemoptysis. She never smoked in her life and reported no history of chronic cough, weight loss or night sweats. She did not notice any rash or joint pain. Her husband had a mild episode of sore throat and cough a few days ago. She traveled to Morocco 1 year earlier, but denied any other recent traveling. She cleaned her attic at home 5 days prior to presentation and may have been exposed to dust at that time, but otherwise denied any exposure of environmental or industrial agents with known pulmonary toxicity. Her vital signs consisted of a blood pressure of 110/67 mmHg, heart rate of 126 beats/min, temperature of 100.1 F and respiratory rate of 20 rpm. Oxygen saturation was 97% on room air. Lung auscultation revealed bilateral diffuse crackles in all lung fields. Cardiac examination showed regular tachycardia with normal S1 and S2, and no murmurs. No JVD or pedal edema was appreciated.
Laboratory investigations at presentation showed no leukocytosis with white blood cell count of 8,900 with 78.1% neutrophils, 15.3% lymphocytes and 6.8% monocytes; acute anemia with hemoglobin 5.5 g/dL, and hematocrit of 19.7% was noted (baseline hemoglobin was around 8 g/dL 3 months before); Reticulocyte count 0.07; Platelet count 363,000 and MCV 64.4 fL. Basic metabolic panel yielded normal kidney functions with serum creatinine 0.7 mg/ dL, BUN11 mg/dL, BUN/creatinine ratio of 14.9 and normal serum electrolytes. Hepatic panel was normal. TSH 3.39 mcIU/mL which is within normal limit. Anemia work up displayed: Serum Iron 307 mcg/dL; Total Iron Binding Capacity 364 mcg/dL with 80% saturation; Transferrin 306 mcg/dL; Ferritin of 155 ng/dL; consistent with anemia of chronic disease, mildly elevated LDH 338 unit/L; normal Haptoglobin level of 98 mg/dL and low Vitamin B12 of 131 pg/ml. ABG revealed normal pH and PaO2. Urinalysis revealed proteinuria (1+), microscopic hematuria (3+) and red blood cells 16-30/high power field. Urine Random Protein was 180.4 mg/dL and Urine protein creatinine ratio was 1.79 from spot urine.
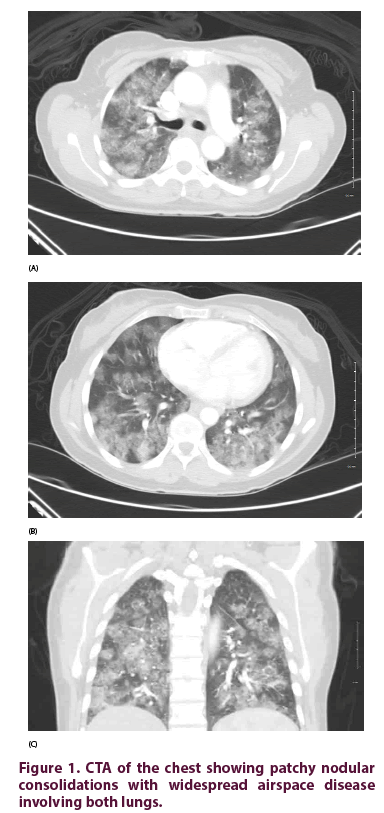
CTA of the chest (Figure 1) showed patchy nodular consolidations with widespread airspace disease involving both lungs, which raised the concern for pneumonia or vasculitis. There was no mediastinal adenopathy. Given initial concern with pneumonia, the patient was started on IV vancomycin and piperacillin-tazobactam empirically and was given 2 units of PRBCs along with Vitamin B12 IM daily for 7 days and ferrous sulfate 325 mg daily. A bronchoscopy was performed and repeated Broncho Alveolar Lavage (BAL) samples indicated alveolar hemorrhage. In the light of suspected vasculitis, she was started on intravenous methylprednisolone 1 g daily.
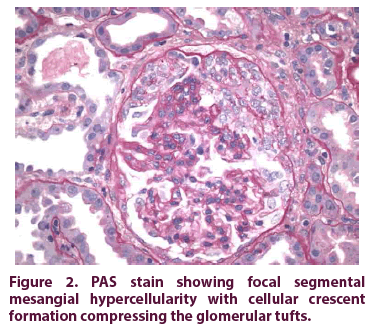
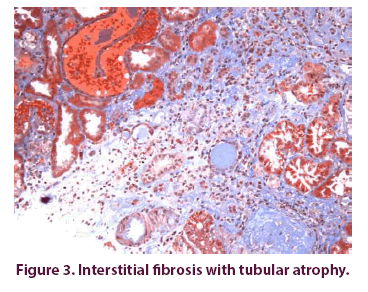
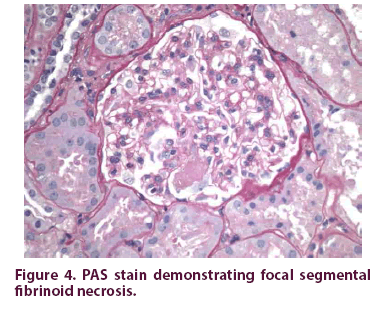
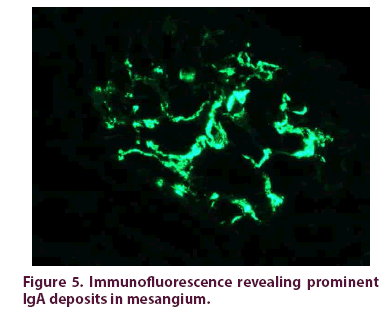
Serology for Anti Neutrophil Cytoplasmic Antibodies (ANCA), Antinuclear Antibodies (ANA), rheumatoid factor, glomerular basement membrane antibody (Anti-GBM), Myeloperoxidase antibody, proteinase 3 antibody, P Jirovecci DNA on bronchial wash, Histoplasma antigen, Aspergillus antibody, HIV, Lyme, Hepatitis B, Hepatitis C and Mycoplasma IgM antibody were all negative. Anticardiolipin IgM and beta-2 glycoprotein antibodies are negative. Babesia and Ehrlichia smear turned out to be negative. Respiratory viral panel was also negative. Serum complement C3 was mildly low (83) and C4 was normal. Serum protein Electrophoresis revealed elevated Free kappa light chains (21.5), normal lambda light chain (16.8 and normal free kappa/lambda ratio. No monoclonal peak identified on Urine Protein Electrophoresis. Given diffuse alveolar hemorrhage of unclear cause and hematuria with proteinuria, renal biopsy was performed. Pathological analysis demonstrated focal segmental and crescentic glomerulonephritis with interstitial fibrosis, and fibrinoid necrosis on PSA staining (Figures 2-4), immunofluorescence staining revealed IgA deposits (Figure 5), consistent with IgA vasculitis, with mild activity and mild chronicity. After completing three days of IV steroids, patients’ respiratory symptoms improved significantly. Given improvement of her symptoms, she was discharged and advised to continue tapering dose of oral prednisone and follow up in the office. Later on, it was planned to infuse Cyclophosphamide 500 mg every 2 weeks for total 6 doses. She has received 2 infusions so far and has no recurrence of hemoptysis.
Discussion
IgA Vasculitis, previously known as Henoch- Schonlein Purpura (HSP), is an immune complex vasculitis affecting small vessels. It occurs primarily in young children, being the most common systemic vasculitis in childhood, having an incidence of 3 to 26/100.000 individuals, with peak age of incidence between 4 to 7 years [8]. Conversely, it is a rare condition in adults, with an annual incidence of 0.1 to 1.8/100.000 [9]. Previous studies showed that IgA Vasculitis is benign and self-limited in children but more severe in adults [4].
In regards to its clinical presentation, adults with IgA vasculitis have a higher frequency of joint symptoms at disease onset, and lower frequency of abdominal pain and fever. it has been reported that up to 96% experience purpura, 61% arthralgias, and approximately 58% have some degree of gastrointestinal involvement, usually characterized by abdominal pain. Hypertension is noted in a third of cases. Renal involvement occurs with a prevalence ranging from 45 to 85%. Microscopic hematuria is the most sensitive and earliest finding suggestive of nephropathy during IgA vasculitis, and it is often associated with variable degrees of proteinuria, at times on the nephrotic range [1]. Renal failure can be found in about a third of patients, ranging from variable degrees of GFR reduction to end stage renal disease. Up to 40% of adult cases may present with renal failure at the time of diagnosis. Conversely, renal failure at the time of diagnosis is rare in children [10,11]. Such finding is likely due to the slow progression of the disease. The clinical progression of the renal disease is variable but, generally speaking, up to 30% of patients may require renal replacement therapy within 20 to 25 years of disease onset [12]. Therefore, early detection of IgA nephropathy is essential in order to prevent long term renal complications.
Diffuse Alveolar Hemorrhage (DAH) is a distinctly rare complication of IgA vasculitis, with incidence ranging from 1.6 to 5% according to different reports [5,13]. It is an acute and often life-threatening condition that may present with different pathological forms such as pulmonary capillaritis, bland pulmonary hemorrhage (without vasculitis or capillaritis), diffuse alveolar damage, or miscellaneous histology. The most common pathological finding is pulmonary capillaritis [14,15]. Most cases of IgA vasculitis with DAH have concomitant purpura on presentation [16]. Patients with IgA vasculitis that present with pulmonary hemorrhage may have variable respiratory symptoms ranging from mild respiratory distress to profound respiratory failure requiring mechanical ventilation (about 50% of the cases), which can lead to death in up to a third of these patients [5,16].
Our case was unique in that it involved an adult patient who had an atypical presentation of IgA Vasculitis with DAH but no significant respiratory failure, joint symptoms, gastrointestinal symptoms, or purpura. Moreover, the mean age of onset of DAH is 16.5 years [16], and our patient was 47 years old. Because of the atypical features, IgA vasculitis was not considered as a major differential diagnosis initially. Furthermore, up to a third of patients with IgA vasculitis may have some degree of kidney dysfunction evident by GFR reduction [17], our patient had hematuria and proteinuria, but normal GFR.
A variety of regimens have been tried for the treatment of IgA vasculitis. The combination of pulse dose of steroids and cyclophosphamide has been commonly used in many of the previously reported cases [13,16,18,19]. Plasmapheresis has also been used in addition to steroids for the severe forms of the disease [20]. In our experience, the patient was treated with intravenous pulse dose of methylprednisolone of 1 g intravenously daily for 3 days and maintenance dose of 60 mg oral daily thereafter, with improvement of her respiratory symptoms. Cyclophosphamide was added after the biopsy results.
Conclusion
This case demonstrated that IgA vasculitis can manifest in adults as diffuse alveolar hemorrhage and hematuria without showing other manifestations, such as purpura, abdominal pain, renal failure, neurological manifestations, and arthralgia. In the presence of diffuse alveolar hemorrhage and unexplained hematuria, a renal biopsy may be essential for making an accurate diagnosis of IgA vasculitis, even in the absence of other signs of renal failure. High dose corticosteroid therapy was an effective strategy for the initial acute management of this patient followed by maintenance on cyclophosphamide infusions therapy. Hopefully this report will help to raise awareness about atypical presentations of IgA vasculitis among adults.
References
- Audemard-Verger A, Pillebout E, Guillevin L et al. IgA vasculitis (Henoch-Shonlein purpura) in adults: Diagnostic and therapeutic aspects. Autoimmun. Rev. 14(7), 579–585 (2015).
- Jithpratuck W, Elshenawy Y, Saleh H et al. The clinical implications of adult-onset henoch-schonelin purpura. Clin. Mol. Allergy 9(1), 9 (2011).
- Bernardino V, Mendes-Bastos P, Rodrigues A et al. IgA vasculitis (formerly Henoch-Schönlein purpura) in an adult with systemic lupus erythematosus. BMJ. Case. Rep. 2015, bcr2015210121 (2015).
- Garcia-Porrua C, Calvino MC, Llorca J et al. Henoch-Schonlein purpura in children and adults: clinical differences in a defined population. Semin. Arthritis. Rheum. 32(3), 149–156 (2002).
- Miyoshi S, Nagao T, Kukida M et al. Pulmonary Hemorrhaging as a Fatal Complication of IgA Vasculitis. Intern. Med. 57(21), 3141–3147 (2018).
- Nadrous HF, Yu AC, Specks U et al. Pulmonary Involvement in Henoch-Schönlein Purpura. Mayo. Clin. Proc. 79(9), 1151–1157 (2004).
- Blanco R, Martínez-Taboada VM, Rodríguez-Valverde V et al. Henoch-Schönlein purpura in adulthood and childhood: two different expressions of the same syndrome. Arthritis. Rheum. 40(5), 859–864 (1997).
- Saulsbury FT. Henoch-Schonlein purpura. Curr. Opin. Rheumatol. 13(1), 35–40 (2001).
- Yang YH, Hung CF, Hsu CR et al. A nationwide survey on epidemiological characteristics of childhood Henoch–Schonlein purpura in Taiwan. Rheumatology (Oxford). 44(5), 618–622 (2005).
- Pillebout E, Verine J. Henoch-Schonlein purpura in the adult. La. Revue. De. Medecine. Interne. 35(6), 372–381 (2014).
- Lai KN, Leung JC, Tang SC. Recent advances in the understanding and management of IgA nephropathy. F1000Res. 11, 5 (2016).
- Barratt J, Feehally J. IgA nephropathy. Journal of the American Society of Nephrology: JASN. 16(7), 2088–2097 (2005).
- Oluwole K, Esuzor L, Adebiyi O et al. Pulmonary hemorrhage with hematuria: do not forget IgA nephropathy. Clin. Kidney. J. 5(5), 463–466 (2012).
- Park MS. Diffuse Alveolar Hemorrhage. Tuberc. Respir. Dis (Seoul). 74(4), 151–162 (2013).
- Ioachimescu OC, Stoller JK. Diffuse alveolar hemorrhage: Diagnosing it and finding the cause. Cleve. Clin. J. Med. 75(4), 258–280 (2008).
- Rajagopala S, Shobha V, Devaraj U et al. Pulmonary hemorrhage in Henoch-Schönlein purpura: case report and systematic review of the English literature. Semin. Arthritis. Rheum. 42(4), 391–400 (2013).
- Audemard-Verger A, Terrier B, Dechartres A et al. Characteristics and Management of IgA Vasculitis (Henoch-Schönlein) in Adults: Data From 260 Patients Included in a French Multicenter Retrospective Survey. Arthritis. Rheumatol. 69(9), 1862–1870 (2017).
- Ronkainen J, Koskimies O, Ala-Houhala M et al. Early prednisone therapy in Henoch- Schönlein purpura: A randomized, double-blind, placebo-controlled trial. J. Pediatr. 149, 241–247 (2006).
- Chartapisak W, Opastiraku S, Willis NS et al. Prevention and treatment of renal disease in Henoch-Schönlein purpura: A systematic review. Arch. Dis. Child. 94(2), 132–137 (2009).
- Augusto JF, Sayegh J, Delapierre L et al. Addition of Plasma Exchange to Glucocorticosteroids for the Treatment of Severe Henoch-Schönlein Purpura in Adults: A Case Series. Am. J. Kidney. Dis. 59(5), 663–669 (2012).