Mini Review - Archives of Nursing and Care (2022) Volume 5, Issue 7
Diagnostic Significance of Quality Markers and Death Predictors for Older Patients with Home Health Pneumonia: A Meta Analysis
Rachael Martin*
Carolina Population Center, University of North Carolina at Chapel Hill, 104 CPC South, Chapel Hill, NC 27516, USA
Carolina Population Center, University of North Carolina at Chapel Hill, 104 CPC South, Chapel Hill, NC 27516, USA
E-mail: Rachaelm@unisa.edu.au
Received: 02- August 2022, Manuscript No. OANC-22-73628; Editor assigned: 04- August -2022, PreQC No. OANC-22-73628 (PQ); Reviewed: 18-August-2022, QC No. OANC-22-73628; Revised: 23-August -2022, Manuscript No. OANC-22- 73628 (R); Published: 30-August-2022 DOI: 10.37532/oanc.2022.5(7).79-83
Abstract
Background
Current risk stratification tools, primarily used for CAP, are suboptimal in predicting home acquired pneumonia (NHAP) outcome and mortality. We conducted a scientific review to evaluate current evidence on the usefulness of proposed predictors of NHAP mortality.
Methods
PubMed (MEDLINE), EMBASE, and CINAHL databases were looked for articles published in English between January 1978 and January 2014. The literature search elicited a complete of 666 references; 580 were excluded and 20 articles met the inclusion criteria for the final analysis.
Results
More studies supported the Pneumonia Severity Index (PSI) as a superior predictor of NHAP severity. Fewer studies suggested CURB-65 and SOAR (especially for the necessity of ICU care) as useful predictors for NHAP mortality. there's weak evidence for biomarkers like C-reactive protein and copeptin as prognostic tools.
Conclusion
The evidence supports the utilization of PSI as the best available indicator while CURB-65 may be an alternative prognostic indicator for NHAP mortality. Overall, thanks to the paucity of information, biomarkers might not be as effective in this role. Larger prospective studies are needed to determine the most effective predictor(s) or combination scheme to help clinicians in decision-making related to NHAP mortality
Keywords
Pneumonia • Malnourishment • Multi-drug-resistant • Prognostic
Introduction
The rate of growth in the elderly population around the world has led to the estimate that 40% of adults around the world will reside in a long-term care (LTC) facility for some time before death, over the subsequent 30 years. Nursing home-acquired pneumonia (NHAP) is currently the second commonest type of infection among patients in LTC facilities in the USA. NHAP is additionally responsible for a majority of emergency department transfers [1]. Several patient characteristics predispose home patients to pneumonia, including chronic diseases, impaired functional abilities, malnourishment, diminished cough reflex, lack of connective tissue , and decreased immunoglobulin A . Additionally, attributes of the home setting including the lack of immunizations, presence of multi-drug-resistant organisms, and widespread use of antibiotics also contribute to a greater risk of pneumonia. Thus, pneumonia represents 13–48% of all infections in home settings. Importantly, NHAP has the very best rates of morbidity and mortality among all the infections that occur in nursing homes, with rates of mortality reported to succeed in 55% [2]. In some countries like South Korea, NHAP is that the leading cause of mortality in longterm residents. The incidence of pneumonia is estimated to be 10 times greater in nursing homes compared to individuals living within the community. The hospitalization rates of NHAP, however, are estimated to be almost 30 times that of CAP. The importance of NHAP mortality is illustrated by the fact that NHAP mortality rates are higher than those related to community-acquired pneumonia (CAP), starting from 5 to 40% according to some accounts. While traditionally the surplus mortality of NHAP was thought to be due to multi-drug-resistant (MDR) organisms, current research has pointed to the presence of comorbidities within the nursing home setting as a major reason for the higher mortality than CAP [3].
The home setting poses several diagnostic challenges for identifying NHAP. While a causative agent is identified but 50% of the time in elderly pneumonia patients, in nursing homes the share is even less; sputum production from patients for samples is challenging due to delirium, dementia, impaired cough reflex, and dehydration. Other obstacles in obtaining essential respiratory samples include the very fact that many patients are treated with empirical antibiotics or steroids prior to specimen collection. The interpretation of signs and symptoms is usually confounded by several factors. Chest radiography is usually challenging to conduct in the elderly due to numerous factors: the relative suboptimal quality of portable radiographs used in nursing homes and the difficulty for frail patients to cooperate and stay upright for X-rays. Additionally, elderly patients present with atypical presentations and with less symptoms than younger patients, complicating the popularity of NHAP. home patients typically are afflicted with several comorbidities, including depression, declining functional status, chronic coronary failure , impaired cognition, and respiratory ailments; thus clinical symptomology and laboratory results often lack sensitivity and specificity for NHAP. Thus, there's often a delay in the diagnosis of pneumonia, thereby contributing to increased mortality in elderly patients. This warrants the necessity for validating optimal clinical biomarkers and clinical tools to diagnose and assess the severity of NHAP. Yet, clinicians lack a definitive prognostic tool or risk stratification scheme that distinguishes which home residents may be more prone to mortality due to NHAP. In recent years, a growing area of interest has been identifying the foremost optimal biomarkers in the management and prognosis of NHAP. the very fact that guidelines among infectious disease societies differ with antimicrobial approach (as some focus on empirical treatment covering drug resistant pathogens) underscores the importance of a severity assessment scheme that can influence medication decisions [4]. Recognition of disease severity and identification of patient subtypes which will be at a greater risk of mortality can influence decisions on antibiotic administration.
An important issue that has been raised is whether it is necessary to hospitalize all NHAP patients. there's a clear need for a clinical tool that can predict mortality and functional deterioration due to hospitalization in NHAP patients. Such a tool would enhance patient outcomes and enable better allocation of healthcare resources. Additionally, a predictive tool may influence decisions for ICU admission for NHAP patients presenting to the emergency department setting. This systematic review sought to explore the present literature on NHAP risk stratification and specific predictors for disease severity that may serve as a clinical judgment tool for clinicians and inform decisions of prioritizing care, hospitalization, ICU admissions, and administering prophylactic antibiotics.
Methods
The authors investigated NHAP with the goal of identifying predictors of mortality from this disease. The study methodology conformed to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement for systematic reviews.
Eligibility Criteria
Studies were selected supported preset inclusion and exclusion criteria. Inclusion criteria are comprised of studies on NHAP with patients 65 years old or older, assessing risk factors, and predictors of prognosis. Many studies have included younger individuals who have a special prognosis. it's thus been argued that the attributes of NHAP can be best determined by comparing patients who are at 65 years of age or older.
Information Sources and Search
A literature search utilized several databases: PubMed, EMBASE, and CINAHL. Studies were selected supported preset inclusion and exclusion criteria. Systematic search was restricted to studies including humans and published in English, from January 1978 to January 2014. An experienced librarian in electronic search methods performed the literature search. The search strategy and keywords employed during this study are summarized in Table 1.
Database |
Database | Keywords/query |
|---|---|---|
| PubMed | 1 | Nursing home acquired pneumonia risk factors |
| 2 | Nursing home acquired pneumonia predictors | |
| 3 | Nursing home acquired pneumonia United States epidemiology | |
| EMBASE | 1 | Nursing and home and acquired and pneumonia and risk and factors |
| 2 | Nursing and home and acquired and pneumonia and outcome | |
| 3 | Nursing and home and acquired and pneumonia and United and States and epidemiology | |
| CINAHL | 1 | Nursing home acquired pneumonia |
Table 1. Search strategy and keywords employed for the systematic literature search.
Study Selection and Data Collection Process. All abstracts were read and articles of potential interest were reviewed intimately by authors Michael Khalili and Naveen Dhawan to decide on inclusion or exclusion from this systematic review [5]. In cases of disagreement, both authors reviewed and discussed the study and a final judgment was made through consensus.
Data Extraction
Michael Khalili extracted information regarding NHAP from all included studies employing a predetermined template comprising of type of study, number of patients, risk factors for NHAP, and predictors of NHAP severity. Given the heterogeneity of the characteristics studied within the included papers, a metaanalysis wasn't performed.
Results
The literature search elicited a complete of 666 references, from which 491 were duplicates and another 89 were excluded. A complete of 86 articles was reviewed in full text; 20 articles met the inclusion criteria for the current systematic review.
Discussion
NHAP typically affects the elderly patient population that has multiple comorbidities. Several studies that have investigated NHAP in hospitalized patients show mean ages to be 74–82 years, while the 30-day mortality is reported to range from 16.8% to 24.7%. A study in Germany by Klapdor et al. utilizing prospective multicenter data examined 618 patients and compared an older subset (65 years or older) to those but 65 years. during this study, 16% (100 patients) were aged 65 or older and therefore the younger patients below 65 years of age had a mean age of 54 years. While multi-drug-resistant (MDR) pathogens are a therapeutic challenge in NHAP overall incidence was low within the both groups. The younger subject group (less than 65 years of age) showed twice lower mortality than those 65 or over. Importantly, Klapdor et al. showed that patient age was a big determinant in presentation and prognosis of NHAP patients. In older patients, typical symptoms of pneumonia like sputum production, cough, and fever are often absent. They also found that the younger patients mostly presented with fever. Importantly, roughly two-thirds of these with NHAP display temperatures over 100.4 degrees Fahrenheit; home patients have lower baseline temperatures and lower peak temperatures resulting from infection. The diagnosis of pneumonia is usually complicated due to delayed recognition stemming from preexisting and chronic conditions and comorbidities (i.e., stroke and dementia); thus, there's a higher rate of mortality in elderly patients [6]. Further, it's been shown that the prognosis for NHAP is worse for men than women.
Infective Etiology
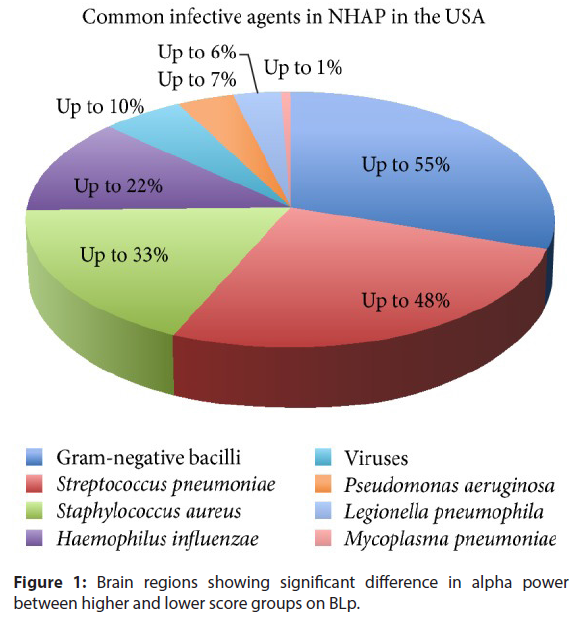
The microbial infective etiology of NHAP remains controversial. a specific challenge in determining microbial etiology lies in obtaining adequate sputum samples, since only as estimated 50–70% of home patients are unable to produce decent sputum samples [7]. While antigen testing of respiratory secretions is beneficial in diagnosing viruses such as RSV and influenza, urinary antigen testing for Legionella pneumophila serotype 1 and Streptococcus pneumonia remains challenging thanks to limited knowledge regarding the susceptibility to antibiotics. The infective agents in NHAP also vary throughout the planet . as an example, during a recent prospective cohort study of 488 nursing home resident patients hospitalized for pneumonia, over half (55.9%) of NHAP cases were thanks to a viral infection. Yet, during a recent prospective study of 217 nursing home residents, 56.3% of NHAP cases were thanks to Enterobacteriaceae. within the USA, NHAP most ordinarily stems from bacteria yet the specific cause is often unknown. While Streptococcus pneumoniae has been identified because the most common infective agent, in additional severe NHAP resulting in hospitalization Staphylococcus aureus and the enteric Gram-negative agents appear more commonly than Streptococcus pneumonia [8]. During a recent study, Staphylococcus aureus was reported to account for the very best mortality. consistent with one study, Staphylococcus spp. were the foremost common agent in the USA comprising 52% of cases, while Streptococcus pneumoniae was the foremost prominent in Europe and Latin America (it was found in 46% of cases in Europe and 25% in Latin America). the massive presence of multi-drug-resistant agents in NHAP patients in the USA has been documented. Typical bacterial agents in NHAP within the USA include Staphylococcus aureus, Pseudomonas, Klebsiella, Proteus mirabilis, and E coli. Typical community-acquired organisms that cause pneumonia include Streptococcus pneumoniae, Haemophilus influenzae, Mycoplasma, Legionella, and Chlamydia. The antibiotics utilized in CAP include azithromycin, macrolides, fluoroquinolones (i.e., levofloxacin), and a mixture of a beta-lactam and a cephalosporin. Common causative organisms of NHAP within the USA are shown in Figure 1. The infective etiology differs, however, in countries like Poland. during a recent prospective study of 217 patients age 65 or above, 56.3% of microorganisms are comprised of Enterobacteriaceae [9], 25% Pseudomonas aeruginosa, and Staphylococcus aureus 12.5%, and Candida albicans is comprised of 6.3%. Thus, NHAP and CAP share many features in their microbial infective etiology including the emergence of drug resistant bacteria. Ma et al. suggested that NHAP shouldn't be treated as healthcare-associated pneumonia instead of community-acquired pneumonia (CAP). The researchers found that, in both NHAP and CAP, multi-drug-resistant bacteria weren't common. Importantly, NHAP also can be caused by a viral etiology. Respiratory syncytial virus (RSV) and influenza remain the foremost common sources of respiratory disease and fatality in nursing homes [10].
Figure 1: Brain regions showing significant difference in alpha power between higher and lower score groups on BLp.
Conclusion
NHAP remains a crucial medical issue in the elderly, particularly thanks to the rise in the nursing home patient population. there's a need for prognostication guidelines for NHAP as severity prediction tools can aid in the allocation of medical resources and translate to improve clinical outcomes. Clinical assessment tools like CURB-65, PSI, and SOAR used for predicting severity in CAP are applied to NHAP. However, they're often intricate in their application and may be marred by inaccuracies due to the frequent lack of presenting symptoms in NHAP patients.
Our study showed that the present evidence points to PSI as having superior predictive value compared to other clinical tools in determining NHAP mortality, with CURB-65 also validated as another very useful gizmo. The subsequent best tool supported by evidence is SOAR, which can have particular benefit in identifying patients in need of ICU admissions. The evidence in support of biomarkers for predicting NHAP mortality isn't completely conclusive, but CRP appears to be the biomarker with the foremost concrete support. Additionally, copeptin may function a reliable predictor of 30-day mortality in NHAP, but more studies are needed to validate its effects and use. No single set of clinical characteristics, prognostic scoring tools, or biomarkers have overwhelming support in their use with NHAP; further prospective studies are warranted in large samples which will delineate the most effective predictor or combination scheme of predictors to ultimately aid clinicians in determining relative likelihood of NHAP mortality.
Conflict of Interest
The authors report no conflict of interest.
References
- Furman CD, Rayner AV, Tobin EP. Pneumonia in older residents of long-term care facilities. American Family Physician. 70, 1495–1500(2004).
- El-Solh AA, Niederman MS, Drinka P.Nursing home acquired pneumonia: a review of risk factors and therapeutic approaches. Current Medical Research and Opinion. 26, 2707–2714(2010).
- Mills K, Nelson AC, Winslow BT et al. Treatment of nursing home-acquired pneumonia. American Family Physician. 79, 976–982(2009).
- Sarin J, Balasubramaniam R, Corcoran AM et al. Reducing the risk of aspiration pneumonia among elderly patients in long-term care facilities through oral health interventions. Journal of the American Medical Directors Association. Current Medical Research and Opinion. 9, 128–135(2008).
- Marik PE, Kaplan D. Aspiration pneumonia and dysphagia in the elderly. 124, 328–336(2003).
- Wojkowska-Mach J, Gryglewska B, Romaniszyn D et al. Age and other risk factors of pneumonia among residents of Polish long-term care facilities. International Journal of Infectious Diseases. 17, 37–43(2013).
- Richards C. Infections in residents of long-term care facilities: an agenda for research. Report of an expert panel. Journal of the American Geriatrics Society. 50, 570–576(2002).
- Mehr DR, Zweig SC, Kruse RL et al. Mortality from lower respiratory infection in nursing home residents: a pilot prospective community-based study. Journal of Family Practice. 47, 298–304(1998).
- Norman D. C. Pneumonia in the elderly: empiric antimicrobial therapy.Geriatrics.46, 26–32(1991).
- Lee JC, Hwang HJ, Park YH et al. Comparison of severity predictive rules for hospitalised nursing home-acquired pneumonia in korea: a retrospective observational study. Primary Care Respiratory Journal. 22, 149–154(2013).
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref