Brief Report - International Journal of Clinical Rheumatology (2021) Volume 16, Issue 4
Depression in adults with idiopathic inflammatory myopathy during the COVID-19 pandemic: A prospective cohort study
- *Corresponding Author:
- Ting Li
Department of Rheumatology, Shanghai Jiao Tong University School of Medicine, Affiliated Renji Hospital, Shanghai, China
E-mail: leeting007@163.com
Chunhua Ye
Department of Rheumatology, Shanghai Jiao Tong University School of Medicine, Affiliated Renji Hospital, Shanghai, China
Abstract
Purpose The COVID-19 outbreak has profoundly changed daily life and how patients access medical care. Idiopathic inflammatory myopathy (IIM) patients, who frequently develop chronic interstitial lung disease (ILD), are at high risk for respiratory infection and are also susceptible to psychological disorders. This study explored depression, anxiety, and compliance among IIM-ILD patients and the association of these factors with disease status during the COVID-19 outbreak in China.
Methods A total of 94 IIM-ILD patients were included in the analysis. Baseline demographic and disease-related information was collected using the medical records system. The following questionnaires were used: Beck Depression Inventory-II (BDI-II), Compliance-Questionnaire- Rheumatology (CQR), Multidimensional Scale of Perceived Social Support (MSPSS), and the State-Trait Anxiety Inventory (STAI). The questionnaires were administered before, during, and after the COVID-19 outbreak in China by a rheumatology nurse through We-Chat.
Results: During the COVID-19 outbreak, a significantly deteriorated depression status and reduced treatment compliance were found among these patients. Female gender and a dosage of greater than 15 mg of glucocorticoid per day were independently associated with depression, while social support was found to be negatively correlated with depression. Clinical follow-up revealed an overall disease flare rate of 17% (16/94). Patients with depression during the COVID-19 outbreak had a significantly higher disease flare rate than those without depression.
Conclusion: Because depression negatively impacts patient quality of life and recovery from primary disease, patients with rheumatic disease should receive an early evaluation, appropriate treatment, and long-term monitoring for depression.
Keywords
COVID-19 • depression • social support • idiopathic inflammatory myopathy • interstitial lung disease
Introduction
Background
An outbreak of COVID-19, the disease caused by SARS-CoV-2, occurred in December 2019 in Wuhan [1]. Clinical manifestations of COVID-19 consist of fever, cough, and fatigue; however, 15% to 20% of patients progress to a severe or critical form of the disease, which can be complicated by acute respiratory distress syndrome and has a high mortality rate [2]. Since the initial outbreak, the COVID-19 pandemic has rapidly become a global emergency. On January 23, 2020, the city of Wuhan shut down in response to the quickly evolving epidemic. On January 30, 2020, the World Health Organization declared the COVID-19 outbreak in China to be a public health emergency of international concern.
As in all cities in China, Shanghai implemented strict social distancing measures, contact tracing, and quarantine protocols in late January 2020. These measures affected many aspects of everyday life and had health, psychological, social, and economic consequences. Studies have revealed a wide range of psychosocial distress manifestations at the individual and community levels, such as panic disorder, anxiety, and depression, that are attributed to the pandemic [3-5].
Idiopathic Inflammatory Myopathy (IIM), commonly termed myositis, refers to a group of rare heterogeneous connective tissue diseases that affect the skeletal muscles and other organ systems. The origin of IIM is unclear, but immunoregulatory abnormalities have been proposed as pathogenic mechanisms [6]. Common manifestations of IIM include skin rashes, proximal muscle weakness, polyarthritis, pulmonary involvement, and dysphagia. The lungs are frequently affected in patients with IIM, who can develop chronic Interstitial Lung Disease (ILD), and ILD may share some Computed Tomography (CT) features with COVID-19 pneumonia [7,8]. Furthermore, high rates of depression and anxiety are common among patients with chronic medical conditions and are typically several times higher than in the general population [9-11]. IIM-ILD patients are at high risk for developing respiratory infection and disease progression, and they may be more susceptible to psychological disorders. Relatedly, the management of IIM-ILD patients has become more complex with the advent of the COVID-19 pandemic.
Purpose
The purpose of this study was to investigate depression and compliance among IIM-ILD patients during the COVID-19 pandemic and their association with disease prognosis.
Methods
Patients
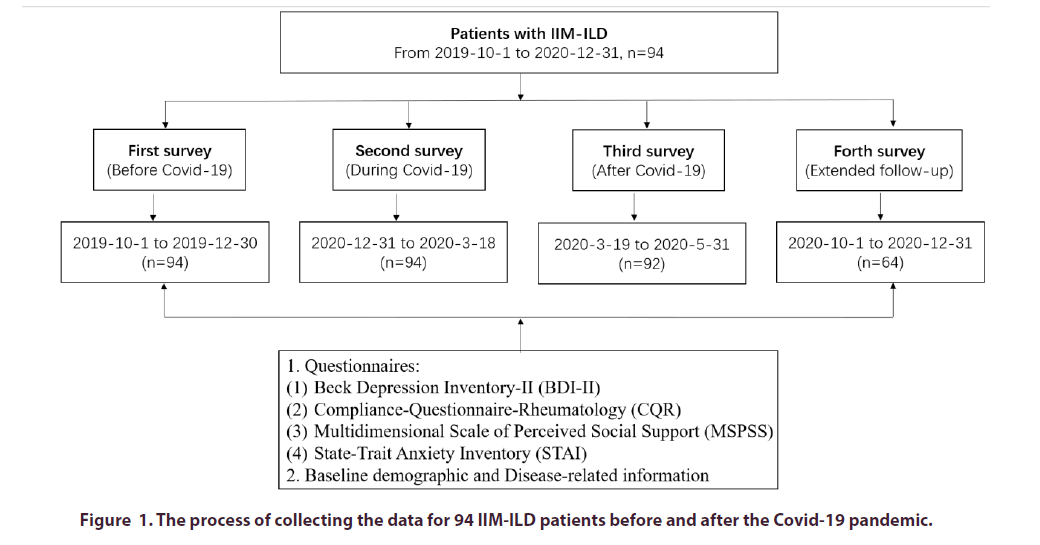
The cohort included in this study consisted of 94 participants who were recruited from the Department of Rheumatology, Renji Hospital South Campus, Shanghai, China. The definition of IIM-ILD was in accordance with a previous report [12]. Patients with malignancy-associated IIM were excluded. The data collection of this prospective cohort study was carried out in four periods: from October 1, 2019 to December 30, 2019 (first survey, before the COVID-19 outbreak in Wuhan); from December 31, 2019 to March 18, 2020 (second survey, during the COVID-19 outbreak); from March 19, 2020 to May 31, 2020 (third survey, after the COVID-19 outbreak); and from October 1, 2020 to December 31, 2020 (forth survey, extended follow-up) (Figure 1). None of the participants had been infected with COVID-19. Written informed consent was obtained from all participants, and the study was carried out in accordance with the Declaration of Helsinki code of ethics.
Measured variables
The following questionnaires were administered by a rheumatology nurse through We-Chat.
The Beck Depression Inventory-II (BDI-II) [13] was used to evaluate depressive symptoms. A score of less than 13 is considered normal, 14–19points indicates mild or probable depression, 20–28 points indicates moderate or definite depression, and greater than 28 points indicates severe depression.
The Compliance-Questionnaire-Rheumatology (CQR) [14] is a rheumatology-specific instrument that measures patient compliance with drug regimens. The total score can vary from 0 (complete noncompliance) to 100 (perfect compliance).
The Multidimensional Scale of Perceived Social Support (MSPSS) [15] is used to assess perceived social support from three areas: family, friends, and significant others. The MSPSS has been applied in several populations, including patients affected by chronic conditions. The scores of each subscale range from 1 to 7, with higher scores indicating higher perceived social support.
The State-Trait Anxiety Inventory (STAI) [16] consists of two 20-item inventories. For each inventory, scores range from 20–80, with higher scores indicating higher levels of anxiety.
In addition, baseline demographic and disease-related information was collected from the medical records system.
Statistical analysis
The independent sample Student’s t-test and the Mann–Whitney U test were conducted, as appropriate. Correlations among the BDI-II, CQR, STAI, and MSPSS results were evaluated by Spearman correlation and linear regression analysis. We compared the proportions between groups using the chi-squared test. Kaplan–Meier survival analysis was conducted to assess when and how frequently a disease flare occurred during the follow-up period. Subsequent comparisons between survival curves were made using a log–rank test. The statistical analyses were performed using GraphPad 5.0 (San Diego, CA, USA). Statistical significance was defined as p<0.05.
Results
We identified 94 patients with IIM-ILD who attended a follow-up visit in our department between October 1 and December 30, 2019. The mean (standard deviation) age was 49.0 years (11.8), and 68 (72.3%) were women.
The median (interquartile range) disease duration of ILD was 12 months (7–19). At the time of enrollment, all patients were on a glucocorticoid medication, and 34 (36.2%) were on an anti-fibrosis medication. A total of 53 (56.3%) patients exhibited anti-MDA5-positive Dermatomyositis (DM), and the majority of these patients were receiving tofacitinib [17]. Azathioprine, mycophenolate mofetil, methotrexate and rituximab were the most frequently used medications among anti- MDA5-negative DM patients. Depressive symptoms were common before the COVID-19 outbreak, with 26 (27.7%) patients classified as currently experiencing depressive symptoms (BDI-II score ≥14), of whom 84.6% (22/26) had mild–moderate symptoms and 15% (4/26) had severe symptoms.
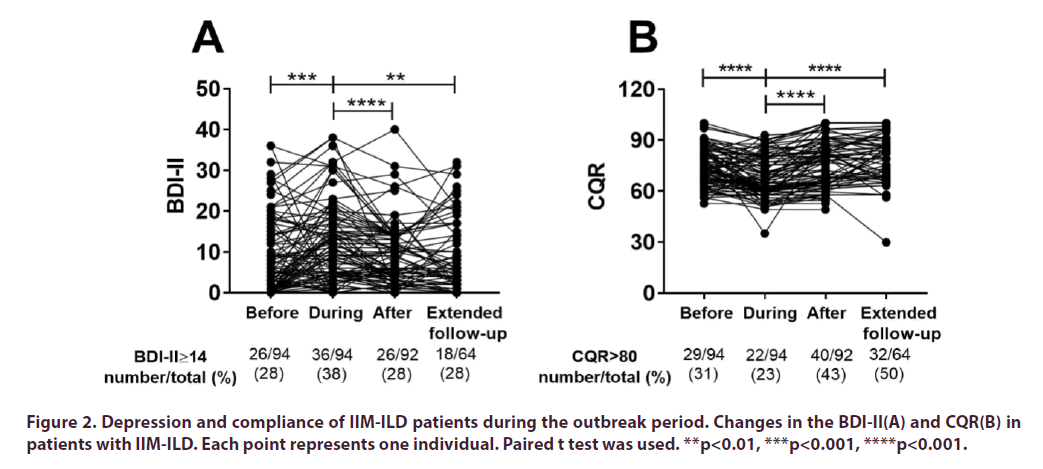
During the COVID-19 outbreak, the outpatient clinic was closed and all non-emergency visits were rescheduled in our hospital, which was a severe disadvantage for patients. As expected, significantly increased BDI-II scores (p<0.001) and reduced CQR scores (p<0.0001) were found in the patient cohort (Figure 2A and Figure 2B). Furthermore, 54 (57.4%) patients were found to have clinically significant anxiety symptoms when applying an STAI cutoff of 40 points (16) (data not shown). An analysis of the association between the STAI score and the BDI-II score revealed a significant positive correlation (r=0.38, p<0.0001) (data not shown).In the univariate analysis, depression was associated with female gender (p=0.005), lower social support (p=0.01), and higher glucocorticoid dosage (p=0.047) (Table 1). Since March 18, 2020, no new domestically acquired COVID-19 cases have been reported in China, and routine outpatient care for chronic diseases has resumed. The number of patients with satisfactory compliance (CQR score >80) increased from 22 (23.4%) during the outbreak to 40 (42.6%) after the outbreak (p=0.004). The number of patients with depression decreased from 36 (38.3%) during the outbreak to 26 (27.6%) after the outbreak (Figure 2A and Figure 2B).
| Item number and description | Total N=94 |
Subjects without depressive symptoms N=58 |
Subjects with depressive symptoms N=36 |
p |
|---|---|---|---|---|
| Socio-demographic variables | ||||
| Age, mean (SD) | 49.0 (11.8) | 48.3 (12.9) | 49.5 (11.7) | 0.463 |
| Female, number (%) | 68 (72.3) | 36 (62.0) | 32 (88.9) | 0.005 |
| Anti-MDA5-positive DM (%) | 53 (56.3) | 35 (60.3) | 18 (50.0) | 0.326 |
| Duration of ILD, months, median (IQR) | 12 (7, 19) | 13 (7, 19) | 12 (8, 19) | 0.718 |
| Marital Status, Married, number (%) | 89 (94.7) | 54 (93.1) | 35 (97.2) | 0.387 |
| Education, ≥High School, number (%) | 46 (48.9) | 28 (48.3) | 18 (50.0) | 0.871 |
| Annual income, ≥15,000$, number (%) | 22 (23.4) | 14 (24.1) | 8 (22.2) | 0.831 |
| Questionnaires | ||||
| BDI-II, mean (SD) | 12.0 (9.6) | 5.6 (4.1) | 21.3 (7.5) | <0.0001 |
| STAI, mean (SD) | 41.4 (10.1) | 37.8 (9.4) | 47.3 (8.2) | <0.0001 |
| STAI>40, number (%) | 54 (57.4) | 25 (43.1) | 29 (80.6) | 0.0004 |
| CQR, mean (SD) | 67.9 (12.2) | 69.1 (13.0) | 66.1 (10.5) | 0.275 |
| CQR>80, number (%) | 22 (23.4) | 15 (25.8) | 7 (19.4) | 0.475 |
| MSPSS, mean (SD) | 63.7 (12.0) | 66.1 (11.1) | 59.8 (12.7) | 0.01 |
| MSPSS>60, number (%) | 55 (58.5) | 40 (68.9) | 15 (41.7) | 0.009 |
| Treatment | ||||
| Glucocorticoid, mg/day, mean (SD) | 16.8 (12.8) | 14.9 (11.3) | 20.4 (14.8) | 0.047 |
| Glucocorticoid>15mg, number (%) | 41 (43.6) | 20 (34.5) | 21 (58.3) | 0.023 |
| Antifibrosis therapy, number (%) | 34 (36.2) | 23 (39.6) | 11 (30.6) | 0.372 |
| Immunosuppressant, number (%) | ||||
| Tofacitinib | 44 (46.8) | 30(51.7) | 14 (38.9) | 0.225 |
| Azathioprine | 10 (10.6) | 5 (8.6) | 5 (13.9) | 0.421 |
| Mycophenolatemofetil | 9 (9.6) | 5 (8.6) | 4 (11.1) | 0.69 |
| Methotrexate | 10 (10.6) | 4 (6.9) | 6 (16.7) | 0.135 |
| Rituximab | 8 (8.5) | 3 (5.2) | 5 (13.9) | 0.141 |
SD: Standard Deviation; DM: Dermatomyositis; ILD: Interstitial Lung Disease; IQR:Inter Quartile Range; BDI-II: Beck Depression Inventory-II; CQR: Compliance-Questionnaire-Rheumatology; MSPSS: Multidimensional Scale of Perceived Social Support; STAI: State-Trait Anxiety Inventory
Table 1. Examination of covariates of depression during the COVID-19 outbreak.
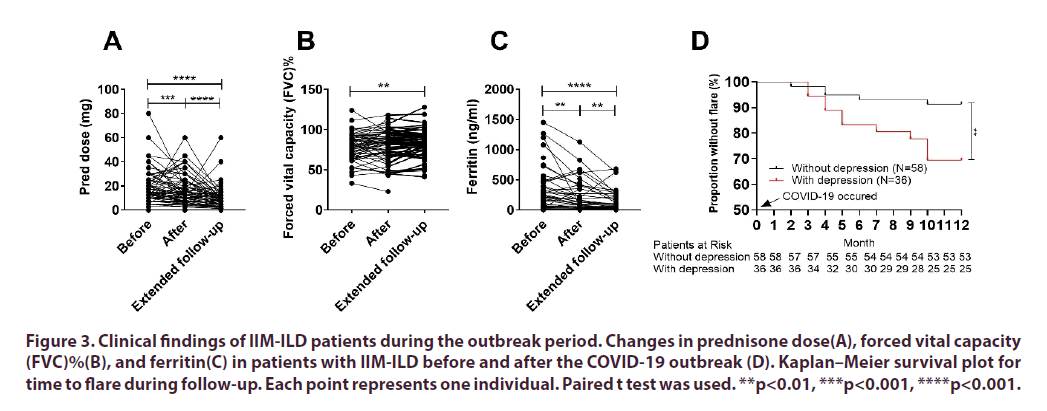
To obtain adequate clinical data, a 1-year follow-up survey was also conducted. The results showed that 78 (83.0%) patients maintained stable disease and had a reduced prednisone dosage (Figure 3A). The extended follow-up also found that the patients had significantly decreased ferritin levels (a useful biomarker for monitoring the activity and severity of ILD (8) and a significantly elevated Forced Vital Capacity (FVC) percentage (Figure 3B and Figure 3C). Overall, 16 (17.0%) patients exhibited disease exacerbation, defined as a worsening of the high-resolution CT results and/ or deteriorated pulmonary function. Among the 16 patients with disease exacerbation, three required intensive care for respiratory failure and died within 4 d.
**p<0.01, ***p<0.001, ****p<0.001.
Figure 3. Clinical findings of IIM-ILD patients during the outbreak period. Changes in prednisone dose(A), forced vital capacity (FVC)%(B), and ferritin(C) in patients with IIM-ILD before and after the COVID-19 outbreak (D). Kaplan–Meier survival plot for time to flare during follow-up. Each point represents one individual. Paired t test was used.
To investigate whether the deteriorated depression status that occurred during the outbreak period in the investigated IIM-ILD patients was associated with disease exacerbation, the patients were divided into two groups: those without depression during the COVID-19 outbreak and those with depression during the COVID-19 outbreak. The disease flare rates were 8.6% (5/58) and 30.6% (11/36) in the two groups, respectively, and the overall flare rate was 17.0% (16/94) (Figure 3D). Thus, in our cohort, patients with depression during the COVID-19 outbreak had a significantly higher flare rate than those without depression (p=0.0064, hazard ratio=3.86, 95% confidence interval 1.39–10.68).
Discussion
Mood symptoms are seldom reported by patients with IIM-ILD. This study shows that IIM patients with ILD experienced worse psychosocial health after the onset of the COVID-19 outbreak. Female gender, having lower social support, and taking a higher dosage of glucocorticoid medication were associated with a higher risk for depression.
Overall, 27.7% (26/94) of the investigated patients had depression before the COVID-19 outbreak, which is in line with a previous study showing that 26.8% (11/41) of people with dermatomyositis experience depression in the course of the disease [18]. During the COVID-19 outbreak, depression was present in 36 (38.3%) of the patients. Depression could have arisen from worries about being infected or difficulties in accessing professional medical treatment. Furthermore, social distancing measures can result in changes to daily routines and disrupt one’s social support. Our findings suggest that higher levels of perceived social support were associated with reduced depressive symptoms during the COVID-19 outbreak. Social support may directly protect against depression, or it may act by mitigating the impact of stressful life events. Therefore, it is important to evaluate social support among this patient populationand strengthening patients’ social support would be a reasonable intervention to improve the psychological well-being of patients with rheumatic disease. We also found that female patients were at higher risk of depression than male patients. This finding is consistent with previous studies showing that women are more likely than men to develop stress-related mental illnesses, including depression [19]. Therefore, medical professionals should particularly consider the mental health of their female patients.
Although people may not think of depression as having a significant health impact, research has shown that depression is associated with immune system dysregulation [20,21]. People with depression have increased levels of circulating inflammatory markers such as C-reactive protein and pro-inflammatory cytokines (including interleukin-6 and tumor necrosis factor-α) [22,23]. Similar results were found in a dermatomyositis case where, during the course of the disease, elevated inflammatory markers were correlated with worsening depression [24]. In the current study, the deterioration of depression status that occurred during the outbreak period was accompanied by disease exacerbation in the IIM-ILD cohort.
To the best of our knowledge, this is the first study to investigate the impact of the COVID-19 outbreak on depression and disease status among IIM patients with ILD. The study utilized pre- and peri-COVID-19 datasets, along with a follow-up dataset. However, there were several limitations to this study. First, although we conducted assessments before, during, and after the COVID-19 outbreak, we cannot exclude other potential confounding effects that are not attributable to the impact of COVID-19, including the natural history of deteriorating mental health over time and the effects of other unmeasured confounders. Second, the size of the study population was small, and a potential selection bias for more severe cases was possible, which could limit the conclusiveness of the results. In the fourth survey, we only got 64 questionnaires from the 91 patients through we-chat. Since it was an investigator-initiated project and patients were not paid for answering the questionnaires. That’s why we could not get enough questionnaires in fourth survey. Third, the pandemic has accelerated changes in health care delivery; however, there are no recommendations for assessing IIM and the associated functional status in telehealth settings. Future studies should continue to explore the validity of measures adapted for IIM treatment and develop strategies to support patients and physicians in the virtual assessment of IIM status.
In summary, depression was found to be highly prevalent in IIM-ILD patients during the COVID-19 outbreak. Because depression negatively impacts patient quality of life and recovery from primary disease, patients with rheumatic disease should receive an early evaluation, appropriate treatment, and long-term monitoring for depression.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial, or not-forprofit sectors.
Competing interests
None declared.
Author contribution
Study Design: TL and CY; Data Collection and Analysis: JC, HW, LQ and WW; Manuscript Writing: HW.
Acknowledgments
None.
References
- Zhu N, Zhang D, Wang W et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 382(8), 727–33 (2020).
- Jiang F, Deng L, Zhang L et al. Review of the Clinical Characteristics of Coronavirus Disease 2019 (COVID-19). J. Gen. Intern. Med. 35(5), 1545–1549 (2020).
- Seyahi E, Poyraz BC, Sut N et al.The psychological state and changes in the routine of the patients with rheumatic diseases during the coronavirus disease (COVID-19) outbreak in Turkey: a web-based cross-sectional survey. Rheumatol. Int. 40(8), 1229–1238 (2020).
- Zhang J, Yang Z, Wang X et al. The relationship between resilience, anxiety and depression among patients with mild symptoms of COVID-19 in China: A cross-sectional study. J. Clin. Nurs (2020).
- Ma YF, Li W, Deng HB et al. Prevalence of depression and its association with quality of life in clinically stable patients with COVID-19. J. Affect. Disord. 275, 145–148 (2020).
- Saketkoo LA, Ascherman DP, Cottin V et al. Interstitial Lung Disease in Idiopathic Inflammatory Myopathy. Curr. Rheumatol. Rev. 6(2), 108–119 (2010).
- Ai T, Yang Z, Hou H et al. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 296(2), E32–E40 (2020).
- Mimori T, Nakashima R, Hosono Y et al. Interstitial lung disease in myositis: clinical subsets, biomarkers, and treatment. Curr. Rheumatol. Rep. 14(3), 264–274 (2012).
- Evans DL, Charney DS, Lewis L et al. Mood disorders in the medically ill: scientific review and recommendations. Biol. Psychiatry. 58(3), 175–189 (2005).
- Bhatia A, Kc M, Gupta L et al .Increased risk of mental health disorders in patients with RA during the COVID-19 pandemic: a possible surge and solutions. Rheumatol. Int. 41(5), 843–850 (2021).
- Ahmed S, Gasparyan AY, Zimba O et al. Comorbidities in rheumatic diseases need special consideration during the COVID-19 pandemic. Rheumatol. Int. 41(2), 243–256 (2021).
- Wang K, Zhao J, Chen Z et al. CD4+CXCR4+ T cells as a novel prognostic biomarker in patients with idiopathic inflammatory myopathy-associated interstitial lung disease. Rheumatology (Oxford). 58(3), 511–521 (2019).
- Wang YP, Gorenstein C. Assessment of depression in medical patients: a systematic review of the utility of the Beck Depression Inventory-II. Clinics. (Sao Paulo).68(9), 1274–1287 (2013).
- de Klerk E, van der Heijde D, Landewe R et al. The compliance-questionnaire-rheumatology compared with electronic medication event monitoring: a validation study. J. Rheumatol. 30(11), 2469–2475 (2003).
- Dambi JM, Corten L, Chiwaridzo M et al. A systematic review of the psychometric properties of the cross-cultural translations and adaptations of the Multidimensional Perceived Social Support Scale (MSPSS). Health. Qual. Life. Outcomes. 16(1), 80 (2018).
- Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis. Care. Res. (Hoboken).63(Suppl11), S467–S472 (2011).
- Chen Z, Wang X, Ye S et al. Tofacitinib in Amyopathic Dermatomyositis-Associated Interstitial Lung Disease. N. Engl. J. Med. 381(3), 291–293 (2019).
- Achtman J, Kling MA, Feng R et al. A cross-sectional study of untreated depression and anxiety in cutaneous lupus erythematosus and dermatomyositis. J. Am. Acad. Dermatol. 74(2), 377–379 (2016).
- Albert PR. Why is depression more prevalent in women? J. Psychiatry. Neurosci. 40(4), 219–221 (2015).
- Rudzki L, Pawlak D, Pawlak K et al. Immune suppression of IgG response against dairy proteins in major depression. BMC. Psychiatry. 17(1), 268 (2017).
- Blume J, Douglas SD, Evans DL et al. Immune suppression and immune activation in depression. Brain. Behav. Immun. 25(2), 221–229 (2011).
- Dahl J, Ormstad H, Aass HC et al. The plasma levels of various cytokines are increased during ongoing depression and are reduced to normal levels after recovery. Psychoneuroendocrinology. 45, 77–86 (2014).
- Raison CL, Capuron L, Miller AHet al.Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends. Immunol. 27(1), 24–31 (2006).
- Reddy A, Birur B, Shelton RC et al. Major Depressive Disorder Following Dermatomyositis: A Case Linking Depression with Inflammation. Psychopharmacol. Bull. 48(3), 22–28 (2018).