Review Article - International Journal of Clinical Rheumatology (2020) Volume 15, Issue 2
Coventry fast track pathway for managing giant cell arteritis
- Corresponding Author:
- Shirish Dubey
Department of Rheumatology, Nuffield Orthopaedic Centre
Oxford University Hospitals NHS Foundation Trust, UK
E-mail: s.dubey@nhs.net
Abstract
Giant cell arteritis (GCA) is the commonest form of vasculitis seen in United Kingdom (UK). It usually presents with new onset headaches, scalp tenderness, jaw claudication or visual symptoms – acute visual loss is a catastrophic presentation and complication of untreated GCA. Hence, it is treated as a medical emergency. Most units have a protocol for assessing these patients and treating these patients promptly – usually this involves the general practitioner GP) starting steroids and sending the patient to secondary care for further evaluation. Recent utility of vascular Doppler ultrasound (US) has allowed many units to develop a fast track pathway for assessing and managing these patients. Coventry established its walk-in fast track pathway which included clinical assessment with rheumatology and/or ophthalmology along with US in 2013. Patients were normally seen within a few hours of referral and the pathway is unique in not needing GPs to start steroids in advance of their assessment in secondary care. This article describes the rationale for the way the pathway was designed and also describes the results of the initial pilot phase of this pathway.
Introduction
Giant Cell Arteritis (GCA) is the most common type of vasculitis affecting 22 per 100,000 people aged over 50 in the UK. It is characterised by systemic inflammation, arteritis and end-organ ischaemia [1]. Typical presenting clinical features include temporal headache, visual disturbance, jaw claudication, and scalp tenderness. Permanent loss of vision, resulting from anterior ischemic optic neuropathy, is the most feared complication of GCA and can affect up to one fifth of patients [2]. Strokes and aortitis leading to aortic aneurysms are recognised later stage complications, but visual loss tends to occur early making GCA a medical emergency [3].
Clinical challenges in GCA
The diagnosis of GCA is challenging due to lack of specific symptoms and the urgency of recognition. A positive Temporal Artery Biopsy (TAB) remains the diagnostic gold standard. However, performing and analysing biopsies is costly, invasive, and creates diagnostic delay [4]. Patients are typically commenced on high dose corticosteroids whilst awaiting biopsy results in view of the risk of blindness, but this unnecessarily exposes unaffected patients to the adverse effects of this treatment which are experienced by 85% of patients. Further, whilst TAB has high specificity, it lacks sensitivity as skip lesions have been well described and biopsy samples may contain unaffected segments of the temporal artery. Therefore, negative results do not always exclude the diagnosis, adding to diagnostic uncertainty [3].
The utility of colour Doppler ultrasonography (US) in the diagnosis of GCA was first proposed in the 1990s [5]. US can be performed quickly, inexpensively, and non-invasively. Typical findings on US include hypoechoic haloes, noncompressible arteries, stenoses, or occlusions [6]. A number of groups have subsequently investigated the role of ultrasonography with mixed results. Whilst a number of groups have reported positive outcomes [7-9], some studies have been less supportive with lower predictive values [10]. Doubts around the utility of US concern the halo sign, the most diagnostic feature on US, as it can disappear within 48 hours of starting corticosteroids [11,12]. A meta-analysis of the studies on the utility of US in the diagnosis of GCA suggested US has a sensitivity of 68% and a specificity of 91% for unilateral haloes, and pooled diagnostic odds ratio of 33.69 [9]. The sensitivity and specificity of US is similar to other rheumatological diagnostic tests such as Rheumatoid factor, dsDNA antibodies, etc.
The need for a Coventry fast track pathway
University Hospitals Coventry and Warwickshire NHS Trust (UHCW) is a secondary care provider for a population of around 500,000. Previously a traditional GCA pathway, in keeping with accepted practice, was used whereby the General Practitioner (GP) would fax a referral to the on call rheumatology Consultant and an appointment would be arranged within two weeks. The patient would be commenced on corticosteroids by their GP pending this consultation. Once the patient had been assessed by a rheumatologist, a temporal artery biopsy would be requested, where appropriate, which would be performed by the vascular surgeons. However, delays in the system meant that temporal artery biopsies were sometimes performed later than 4 weeks from the initiation of corticosteroids. Whilst delays in diagnosis are recognised and can be due to a variety of reasons, they are associated with worse patient outcomes [13]. This led to the consideration of a new rapid access pathway, and work towards this was accelerated by external pressures such as the vascular surgeon leaving the Trust. Discussions were held with our ophthalmologists who were concerned about possible GCA in patients presenting to Opthalmology with acute visual loss. Together, there was enthusiasm for a patient centric pathway that enabled the right team to see the right patient at the right time enabling us to perform the right assessments and institute the right treatment. Our supportive vascular physiology laboratory helped enormously by offering access to same day US assessments, thereby mitigating our concerns about the utility of US after starting corticosteroids. Thus we were able to establish a GCA pathway in which patients could be seen, assessed, investigated, and treated on the same day.
The Coventry fast track pathway
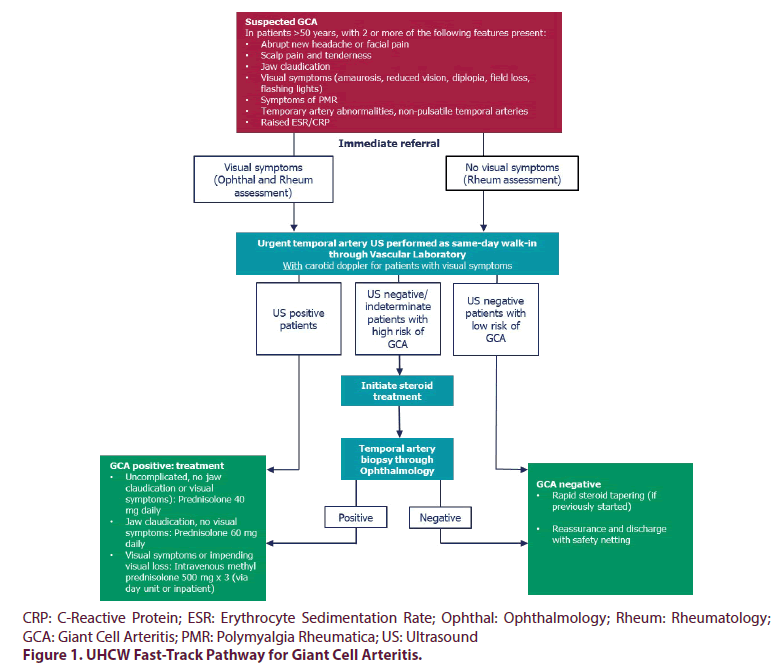
The Coventry fast track pathway was established in 2013 and was the first GCA service in the world to provide immediate assessment and investigations, during working hours, for patients with suspected GCA without the need for initiation of steroids in primary care. The pathway is summarised in Figure 1. Its core aims are:
• To prevent avoidable GCA related vision loss by assessing and treating affected patients promptly
• To avoid unnecessarily exposing unaffected patients to corticosteroids
• To minimise delays and anxiety for patients.
This was achieved through the collaborative efforts of the Rheumatology, Ophthalmology and Vascular Physiology teams.
Description of the pathway
The Rheumatology team receive most of the referrals to the fast track pathway, which are accepted if the patient is aged over 50 and has appropriate clinical features (Figure 1). Referrals predominantly originate from general practitioners but may arise from any source. Telephone referrals are required to minimise delays. Patients referred to Rheumatology are seen on the same day as the referral, or the next working day if they are referred out of hours. For out of hour’s referrals, we usually recommend starting corticosteroids immediately to avoid treatment delays. Comprehensive clinical assessments (including ophthalmology assessment in the eye casualty if required) are performed, relevant blood tests are sent, and US is performed. Patients are reviewed with their results and a management plan is instituted on the same day from the same clinician. In uncertain cases, TAB is performed by the Ophthalmologists on the request of the Rheumatology team, usually within 2 weeks. Patients with low clinical suspicion of GCA and a negative US are reassured and discharged. They undergo rapid steroid tapering if they had been started. Patients with positive US are immediately commenced on oral corticosteroids, or IV methylprednisolone if there is a risk of vision loss. IV methylprednisolone is delivered on an outpatient basis in the Rheumatology Day Unit, but rarely patients are admitted for inpatient treatment. In uncertain cases, corticosteroids are continued until more data are available to inform decision making.
The Ophthalmology team receive referrals for any patient with suspected GCA and visual symptoms. They also identify suspected GCA patients through their unselected take in the Eye Casualty. Patients receive the same assessments and investigations (in addition to ophthalmological assessments) as those attending Rheumatology. Where GCA is suspected or confirmed their care is shared with the Rheumatology team for on-going assessment and management. Where GCA is excluded, alternative causes of visual symptoms are sought. Trained and experienced Ophthalmologists perform TAB in accordance with BSR guidelines when this is required. US is performed by specialist Vascular Scientists in the Vascular Laboratory. The expertise of these scientists means that any vessel thought to be affected can be scanned, in addition to the temporal artery. Carotid arteries are routinely scanned for patients who present with visual symptoms to assess for carotid stenosis and where necessary other arteries can also be looked at [14]. US is performed using a high resolution 5-18MHz Hockey Stick probe (General Electric). Transverse and longitudinal views are examined and colour flow imaging is performed to assess for typical features of GCA including echolucent haloes, incompressible wall thickening, stenoses, and occlusions. In order to optimise the US findings, we aim to perform US before corticosteroids have been initiated. Patients referred out of hours however, are commenced immediately on corticosteroids and their US is performed on the next working day.
Initial pilot phase
When we first set up the fast track GCA pathway in mid-2013, we decided to pilot the initial few months with both US and biopsies. Primarily, this was to ensure patient safety by evaluating the new pathway compared to conventional management. During this pilot 50 patients were seen, the results of investigations for these patients are shown in Table 1. We found a strong correlation between US and TABs. All patients who had definite GCA on US were confirmed by biopsy. Similarly, all patients who had normal US had negative biopsies. US showed indeterminate features in some patients, and some of these were found to have GCA on biopsy, but the majority did not have GCA. These results gave us confidence in our fast track pathway and this was bolstered by the findings of the TABUL study which recommended a similar model as being the best approach for managing GCA [15]. For internal quality assurance, there are regular discussions between the vascular scientists, ophthalmology and rheumatology around patients seen on this pathway. Further evidence of benefit from a fast track pathway comes from a Norwegian study suggesting a reduction in permanent visual loss through FTGCA pathways [16].
Table 1. Initial performance of the Coventry FT GCA pathway.
| Ultrasound | Number of pts. | Biopsy |
|---|---|---|
| Normal | 34 | Normal |
| Stenosis/Occlusion | 4 | 3 normal, 1 GCA |
| Possible halo | 8 | 6 normal, 1 GCA |
| Halo | 4 | All GCA |
| Total | 50 |
Advantages of the Coventry fast track GCA pathway
• It offers patients same day clinical (rheumatology +/- ophthalmology) and radiological assessments, diagnosis and management.
• It removes the need for GPs to routinely initiate corticosteroids prior to specialist assessment thus avoiding corticosteroid exposure for large majority of patients who do not have GCA with reduction in cost and wasted drugs.
• Vascular sonographers are experienced at imaging blood vessels so learning to assess the features of GCA is relatively easy.
• Vascular scientists can assess vessels other than the temporal artery, such as the carotid arteries and occipital arteries, and produce reports that are acceptable to other departments, for example where there is carotid artery stenosis needing endarterectomy. Our group has previously published a case series about occipital artery involvement in GCA [14].
• The pathway is not affected by individual clinician or sonographer absence.
• Patients can be discharged at the first visit.
• Reduction in hospital inpatient bed days.
The Coventry fast track GCA pathway was ‘highly commended’ during the British Society for Rheumatology best practice awards in 2018.
Conclusion
Coventry fast track GCA pathway is the first FTGCA pathway that performs the assessments on the same day (within normal working hours) and does not need GPs to commence corticosteroids resulting in significant multifaceted benefits to patients, reducing prescription costs and wastage of drug. The pathway has demonstrated its robustness in the initial data that are reported here, and appears to have good correlation with biopsies for the diagnosis of temporal arteritis. US is a safe and effective investigation for patients with suspected GCA.
References
- Dasgupta B, Borg FA, Hassan N et al. BSR and BHPR guidelines for the management of giant cell arteritis. Rheumatology. 49(8), 1594–1597 (2010).
- Gonzalez-Gay MA, Blanco R, Rodriguez-Valverde V et al. Permanent visual loss and cerebrovascular accidents in giant cell arteritis: predictors and response to treatment. Arthritis. Rheum. 41(8), 1497–1504 (1998).
- Dejaco C, Brouwer E, Mason JC et al. Giant cell arteritis and polymyalgia rheumatica: current challenges and opportunities. Nat. Rev. Rheumatol. 13(10), 578 (2017).
- Chmelewski WL, McKnight KM, Agudelo CA et al. Presenting Features and Outcomes in Patients Undergoing Temporal Artery Biopsy: A Review of 98 Patients. Arch. Intern. Med. 152(8), 1690–1695 (1992).
- Schmidt WA, Kraft HE, Volker L et al. Colour Doppler sonography to diagnose temporal arteritis. Lancet. 345(8953), 866 (1995).
- Bley TA, Reinhard M, Hauenstein C et al. Comparison of duplex sonography and high-resolution magnetic resonance imaging in the diagnosis of giant cell (temporal) arteritis. Arthritis. Rheum. 58(8), 2574–2578 (2008).
- Karassa FB, Matsagas MI, Schmidt WA et al. Meta-analysis: test performance of ultrasonography for giant-cell arteritis. Ann. Intern. Med. 142(5), 359–369 (2005).
- Ball EL, Walsh SR, Tang TY et al. Role of ultrasonography in the diagnosis of temporal arteritis. Br. J. Surg. 97(12), 1176–-1771 (2010).
- Arida A, Kyprianou M, Kanakis M et al. The diagnostic value of ultrasonography-derived edema of the temporal artery wall in giant cell arteritis: a second meta-analysis. BMC. Musculoskelet. Disord. 11(1), 44 (2010).
- Maldini C, Dépinay-Dhellemmes C, Tra TT et al. Limited value of temporal artery ultrasonography examinations for diagnosis of giant cell arteritis: analysis of 77 subjects. J. Rheumatol. 37(11), 2326–2330 (2010).
- Santoro L, D’Onofrio F, Bernardi S et al. Temporal ultrasonography findings in temporal arteritis: early disappearance of halo sign after only 2 days of steroid treatment. Rheumatology.52(4), 622 (2013).
- Hauenstein C, Reinhard M, Geiger J et al. Effects of early corticosteroid treatment on magnetic resonance imaging and ultrasonography findings in giant cell arteritis. Rheumatology. 51(11), 1999–2003 (2012).
- Ezeonyeji AN, Borg FA, Dasgupta B. Delays in recognition and management of giant cell arteritis: results from a retrospective audit. Clin. Rheumatol. 30(2), 259–262 (2011).
- Luqmani R, Lee E, Singh S et al. The role of ultrasound compared to biopsy of temporal arteries in the diagnosis and treatment of giant cell arteritis (TABUL): a diagnostic accuracy and cost-effectiveness study. Health Technology Assessment: No 20(90), 1-238 (2016).
- Pinnell J, Tiivas C, Perkins P et al. Ultrasonography of occipital arteries to diagnose giant cell arteritis: a case series and literature review. Clin. Rheumatol. 37(2), 569 (2018).
- Diamantopoulos AP, Haugeberg G, Lindland A et al. The fast-track ultrasound clinic for early diagnosis of giant cell arteritis significantly reduces permanent visual impairment: towards a more effective strategy to improve clinical outcome in giant cell arteritis? Rheumatology. 55(1), 66–70 (2016).