Research Article - International Journal of Clinical Rheumatology (2019) Volume 14, Issue 2
Clinical, ultrasonographic and multidetector computed tomography features of temporomandibular joint in rheumatoid arthritis and psoriasis patients
- Corresponding Author:
- Fatma Ali
Department of Rheumatology, El Minia University, Egypt
E-mail: basantmenna@yahoo.com
Abstract
Background: The incidence of Tempro Mandibular Joint (TMJ) involvement in inflammatory arthritis is underestimated. It is more common in Rheumatoid Arthritis (RA) than in Psoriatic Arthritis (PsA). TMJ affection could presented by headache, pain, click difficulty in mouth opening. Different imaging modalities disclose TMJ; conventional radiography, musculoskeletal ultrasound (MSUS), Multi Detector Computed Tomography (MDCT) and Magnetic resonance imaging Due to variability of the complaints, Temporo Mandibular Disorder (TMD) is diagnosed mainly by signs and symptoms. As there are no criteria to attain a numeric value to decide the severity of TMD, indices play an important role to determine the prevalence of this disorder in a specified population. Patients and methods: 75 patients were enrolled; 50 RA according to ACR/EULAR criteria and 25 PsA according to Caspar criteria. TMJ questionnaire was assessed according to Helkimo score. Also MSUS and MDCT scores were done. Results: Clinical TMJ affection was found in 42 RA and in 10 psoriasis patients. According to Helkimo score 84% of RA and 40% of PsA were found. By MSUS 72% of RA patients and 32% of PSA patients were affected. By MDCT 66% of RA patients and only 3% of PsA patients were noticed. There were positive correlation between duration of illness and disc displacement (r=0.4, P=0.0008) and also between morning stiffness with osteophyte and effusion (r=0.3,p=0.03, r=0.4,p=0.01). In PSA there were positive correlations between tender swollen joints with US effusion and erosion (r=0.5 P=0.01, r=0.6 p=0.002, r=0.5 p=0.006, r=0.5 p=0.006) respectively In RA patients, RF positivity was positively correlated with MDCT of impaired mouth opening (r=0.3, p=0.04), and Anti-CCP positivity was positively correlated with MDCT of increased joint space (r=0.4, p=0.01). Conclusion: There was correlation between severity of TMJ dysfunction and disease activity as well as severity in RA and PSA.
Keywords
Rheumatoid arthritis, psoriatic arthritis, temporomandibular joint, musculoskeletal ultrasound, MDCT scores
Introduction
The incidence of Temporomandibular Joint (TMJ) involvement in inflammatory arthritis is often underestimated. Rheumatoid arthritis (RA) and Psoriatic Arthritis (PsA) have an affinity toward the TMJ. The prevalence is highest in RA, followed by PsA [1,2]. Typical clinical findings include joint pain, stiffness, sounds and limitation of movement [3].
Due to variability of the complaints, Temporomandibular Disorder (TMD) is diagnosed mainly by signs and symptoms. As there are no criteria to attain a numeric value to decide the severity of TMD, indices play an important role to determine the prevalence of this disorder in a specified population [4]. Imaging plays a key role in TMJ evaluation [5]. Plain X-ray can primarily evaluate the bony elements of the TMJ. MRI can document both osseous and soft-tissue abnormalities [6]. However, some of the advanced osseous changes of the condyle have not often been evaluated [7].
Computed Tomography (CT) is a good imaging modality for assessment of osseous changes. Multi-Detector Computed Tomography (MDCT) should be done to both TMJs in open and closed mouth positions using thin slice technique (0.5-2 mm thickness). Multi-Planar Reformatted images (MPR) should be done in coronal oblique (parallel to the long axis of the condyle) and sagittal oblique planes using both bone and soft-tissue algorithms [8]. MDCT was considered to be a reliable imaging modality for diagnosis of internal disc derangement, arthritis and other miscellaneous conditions of the TMJ at a relatively low radiation dose [9].
Ultrasound examination (US) of the TMJ allows dynamic evaluation of TMJ joint motion. It can evaluate the presence of joint effusion, condylar erosions as well as detect the increased power Doppler flow due to synovitis. But it was of low sensitivity to detect medial or lateral disc displacements [10].
The aim of the study was to assess TMJ involvement in RA and in psoriasis patients (with and without psoriatic arthritis) clinically, by MSUS and MDCT. Also, to study degree of TMJ affection in relation to the clinical, laboratory and radiological changes.
Patients and methods
Patients
Fifty patients (44 female, 6 male) with RA (mean age 45.4 ± 10.04 years; range 29 to 73 years) who fulfilled the 2010 American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) RA classification criteria [11]; and twenty five patients (16 male, 9 female) with psoriasis (15 patients without psoriatic arthritis and 10 patients with psoriatic arthritis "who fulfilled PsA CASPAR classification criteria" [12] (mean age 44.92 ± 12.80 years; range 20 to 66 years) were consecutively recruited from the rheumatology and dermatology outpatient clinics during the period from September 2016 to September 2018. An informed consent was taken from all patients. The study was approved by the local ethical committee.
Exclusion criteria
Patients with history of dental emergencies, drug abuse, head and neck neoplasia, vascular disease. Also, patients having visual, auditory or neurological disorders were excluded. The swollen 28-joint count (SJC28), tender 28-joint count (TJC28), DAS-28 (ESR) [13] and Ultrasound 7 score [14] were determined for each patient to assess disease activity. Health assessment questionnaire disability index (HAQDI) was calculated (ranged 0-3) [15]. Anticyclic citrullinated peptide level (Anti-CCP), Rheumatoid Factor (RF), and Erythrocyte Sedimentation Rate (ESR) were assessed. X-ray hands, wrists and feet were done for all patients. We assess Simple Erosion Narrowing Score (SENS) [16] in RA patients and assess the modified strein brocker score [17] in PsA patients.
For TMJ involvement, a questionnaire was designed to assess the anamnestic and clinical dysfunction indices according to Helkimo [18]. It was based related to subject symptoms and divided into 0, I, or II according to the anamnestic dysfunction index (Ai). The symptom free subject listed as (Ai 0), subjects with mild symptoms listed as (Ai I) and subjects with severe symptoms listed as (Ai II).
Musculoskeletal ultrasonography (MSUS) of TMJ was performed with a 10–18 MHz linear scanner and middle class to high-end machine US device; for detection of; disc changes (displacement, degeneration or other injuries); Condyle changes (erosions, irregularities or osteophytes) as well as joint effusion [19-21].
All patients underwent the same MDCT using 16-slice GE Bright Speed machine (General Electric Company, Milwaukee, USA) with the same examination protocol using 0.5 mm collimation scanner with a gantry rotation speed of 400 ms/rotation, range of box 450–500, image thickness 0.5 mm, standard pitch factor of 0.641, reconstruction interval 0.5 mm. and total exposure time 6.949. Each scan was obtained with a tube voltage of 120 kV and 250 mAs. Each TMJ was examined for detection of; disc changes, condyle changes, joint effusion, bone irregularity, and degree of opened and closed mouth [22].
Statistical analysis
The statistical analysis was performed using SPSS 16.0 (SPSS Inc., Chicago, Illinois, USA). Descriptive statistics were done by number and percent as well as mean and SD. Correlations were calculated using Pearson’s correlation coefficient. The level of statistical significance was set at p<0.05.
Results
Fifty RA patients and twenty five psoriasis patients (15 without PsA, and 10 with PsA) were included in the present study. Table 1 shows demographic, clinical, laboratory, radiologic and ultrasonographic data. In RA patients, the treatment included non-steroidal anti-inflammatory drugs in 48 (96%) patients, corticosteroids in 16 (32%), methotrexate in 49 (98%), antimalarials in 50 (100%), leflunomide in 10 (20%) and sulfasalazine in 2 (4%) patients. All psoriasis patients received topical steroid and NSAIDSs and methotrexate.
| Parameter mean ± SD (range) n (%) | RA patients (n=50) | Psoriasis patients (n=25) | |
|---|---|---|---|
| Patients without PsA (n=15) | Patients with PsA (n=10) | ||
| Age (years) | 45.4 10.04 (29-73) | 43.27 ± 13.89 (20-63) | 47.40 ± 11.19 (35-66) |
| Sex F:M | 4416 | 619 | 416 |
| DD (years) | 8.6 ± 8.8 (0.2-30) | 5.53 ± 5.43 (0.2-20) | 9.14 ± 6.46 (0.4-16) |
| TJC | 19.3 ± 7.7 (4-28) | - | 2 ± 0 (5-20) |
| SJC | 9.6 ± 5.2 (0-22) | - | 2 ± 0 (1-6) |
| DAS 28 | 2.2 ± 1.1 (0-3) | - | 1.3 ± 0.5 (0.6-3) |
| HAQ-DI | 21 ± 0.8 (0-3) | - | 3.2 ± 1.3 (0.3-2.6) |
| ESR (mm/11 h) | 38.26 ± 20.26 (7-110) | 23.5 17.5 (5-60) | 18.4 12.04 (5-35) |
| Anti-CCP | 70.000 ± 168.8 (5-S44) | 7.2 ± 3.3 (5-10) | 7.2 ± 5.1 (5-15) |
| Anti-CCP +ve | 20 (40) | 0 | 0 |
| RF +ve | 14 (28) | 0 | 0 |
| SENS | 8.4 ± 3.5 (3-20) | ||
| Modified stein broker score | - | 5.7 ± 8.2 (0-22) | 8.8 ± 7.6 (0-31) |
| US 7 score: | |||
| Synovitis in GSUS | 5.2 ± 4 (0-27) | - | 42.4 (0-10) |
| Synovitis in PDUS | 2.8 ± 2.7 (0-12) | - | 2 ± 1.2 (0-6) |
| Tenosynovitis in GSUS | 1.7 ± 1.6 (0-7) | - | 1.2 ± 0.5 (0-5) |
| Tenosynovitis in PDUS | 1.7 ± 1.6 (0-6) | - | 1.2 ± 0.4 (0-5) |
| Erosion GSUS (with wrist) | 5.9 ± 2.5 (0-12) | - | 0.4 ± 0.2 (0-12) |
| Erosion GSUS (without wrist) | 4.7 ± 1.9 (0-9) | - | 3.8 ± 3.4 (0-9) |
Table 1: Characteristics of the patients.
Frequency of clinical involvement of TMJ was shown in Table 2. In RA patients, TMJ was affected clinically in 42 (84%) {36 females and 6 males}, it was unilateral in 35 and bilateral in 7 patients. TMJ pain on palpation were the most frequently observed sign (84%), followed by TMJ sounds (62%) while jaw rigidity or impaired range of mandibular movement was the least frequent one (14%). In psoriasis patients, TMJ was affected clinically in 10 (40%) patients {8 with PsA "32%" and 2 "8%" without PsA}, unilateral in 8 and bilateral in 2 patients. TMJ pain on palpation were the most frequently observed sign (40%), followed by pain with open of mouth (lock) (24%) while joint sound was the least frequent one (8%).
| Parameter n (%) | RA patients (n=50) | Psoriasis patients (n=25) | |
|---|---|---|---|
| TMJ sounds | 31 (62) | 2 (8) | |
| painwith open of mouth (lock) | 29 (58) | 6 (24) | |
| Masticatory pain on palpation | 28 (56) | 4 (16) | |
| TMJ pain on palpation | 42 (84) | 10 (40) | |
| Palpable clicking | 20 (40) | 0 | |
| Pain inmasticatory muscle | 16 (32) | 3 (12) | |
| TMJ pain on movement | 16 (32) | 3 (12) | |
| Fatigue in TMJ | 10 (20) | 0 | |
| Difficult mouth opening | 9 (18) | 0 | |
| Jaw rigidity or impaired range of mandibular movement | 7 (14) | 0 | |
| Helkimo Anamnestic (Ai) | No symptoms | 8 (16) | 15 (60) |
| Mild symptoms | 7 (14) | 10 (40) | |
| Sever symptoms | 35 (70) | 0 | |
| Clinical dysfunction score (Di) | No dysfunction | 8 (16) | 16 (64) |
| Mild dysfunction (1-4) | 33 (66) | 0 | |
| Moderate dysfunction (5-9) | 5 (10) | 0 | |
| Sever dysfunction (9-25) | 4 (8) | 9 (36) | |
Table 2: Frequency of different temporomandi bular signs and symptoms with assessment of clinical severity of TMJ in RA and psoriasis patients.
According to anamnestic component of Helkimo’s index, 16% RA patients and 60% psoriasis patients were free from symptoms, 14% RA patients and 40% psoriasis patients were found to have mild symptoms, and 70% RA patients were having severe symptoms. According to dysfunction component, most of the RA patients had mild dysfunction (66%), while 36% of psoriatic patients had severe dysfunction (Table 3).
| Parameter r (p) | Osteophyte | Disc displacement | Effusion | Erosion | ||||
|---|---|---|---|---|---|---|---|---|
| RA patients (n=50) | Psoriasis patients (n=25) | RA patients (n=50) | Psoriasis patients (n=25) | RA patients (n=50) | Psoriasi s patients (n=25) | RA | Psorias is patients (n=25) | |
| TMJ pain on palpation | 0.2 (0.05) | 0.1 (0.5) | 0.4 (0.01) | 0.3 (0.2) | -0.2 (0.2) | 0.2 (0.3) | -0.2 0.3 | -0.3 |
| Joint sound | 0.2 (0.1) | 0.1 (0.5) | 0.1 (0.4) | 0.5 (0.02) | 0.3 | 0.4 | 0.4 | 0.3 (0.2) |
| Locking jaw | 0.3 (0.03) | 0.5 | 0.3 (0.06) | 0.5 (0.02) | 0.3 | -0.4 | 0.5 | -0.5 |
| TMJ pain on movement | 0.3 (0.07) | 0.3 (0.09) | 0.3 (0.02) | 0.1 (0.5) | 0.2 (0.1) | 0.1 (0.5) | 0.2 (0.2) | 0.1 (0.6) |
| Impaired range of mandibular movement liaw riaiditvl | 0.1 (0.4) | 0.4 (0.04) | 0.3 (0.02) | 0.3 (0.2) | 0.09 | 0.2 (0.3) | 0.2 (0.2) | 0.3 (0.2) |
| Masticatory muscle pain on palpation | -0.2 (0.1) | 0.3 (0.05) | -0.2 (0.1) | 0.7 | 0.3 | 0.6 | 0.3 | 0.4 |
Table 3: Correlations between parameters of TMJ clinical dysfunction score and TMJ ultrasonographic features in RA and psoriasis patients.
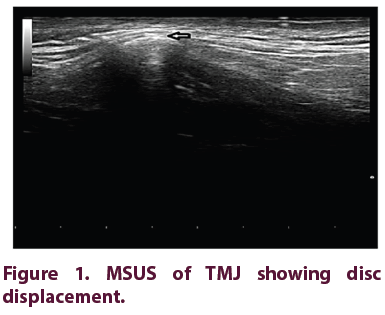
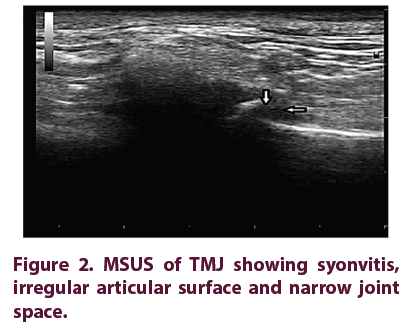
By MSUS, TMJ was affected in 36 RA patients (72%), and all parameters of TMJ MSUS were higher in the right than in the left side [effusion (60%), osteophyte (56%), erosion (50%), and disc displacement (34%) on the right side]. On the other hand, TMJ was affected in only 8 (32%) patients with PsA, and all parameters of TMJ MSUS were higher in the right than in the left side [effusion (32%), osteophyte (28%), disc displacement (28%) and erosion (16%), on the right side]. Features of TMJ MSUS are shown in Figures 1 and 2.
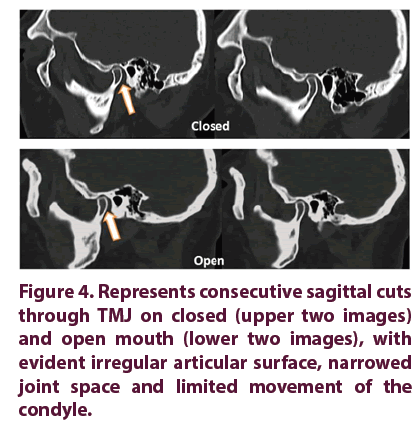
By MDCT, TMJ was affected in 33 RA patients (66%), irregular articular surface was more in the right side (42%), impaired mouth opening and increased joint space were higher in the left side (26%, 8% respectively), and marginal osteophyte at mandibular condyle was equally found in both sides (20%). However, 3 patients only with PsA had features of TMJ involvement by MDCT (impaired mouth opening in the 3 patients, irregular articular surface in 2, and increased joint space in 1 patient. Features of TMJ MDCT are shown in Figures 3 and 4.
In RA and psoriasis patients, TMJ pain and masticatory muscle pain on palpation were positively correlated with DAS-28 (ESR) - as a parameter of disease activity (r=0.4, p=0.01, r=0.4, p=0.01 respectively for RA, r=0.7, p=0.01, r=0.5, p=0.007 respectively for psoriasis patients). While lock jaw was positively correlated with DAS-28 (ESR) in RA patients only (r=0.3, p=0.02).
Correlations between parameters of TMJ clinical dysfunction score and TMJ ultrasonographic features in RA and psoriasis patients are shown in Table 3.
In RA patients, there was positive correlation between duration of illness and disc displacement (r=0.4, p=0.008); and positive correlations of morning stiffness with osteophyte and effusion (r=0.3, p=0.03, r=0.4, p=0.01 respectively).
However, in psoriasis patients, there were positive correlations of 28 tender and swollen joint count with TMJ ultrasonographic effusion and erosion (r=0.5, p=0.01, r=0.6, p=0.002, r=0.5, p=0.006, r=0.5, p=0.006 respectively).
Correlations between parameters of TMJ clinical dysfunction score and TMJ MDCT features in RA patients are shown. However, there were no similar correlations in psoriasis patients.
In RA patients, RF positivity was positively correlated with MDCT of impaired mouth opening (r=0.3, p=0.04), and Anti-CCP positivity was positively correlated with MDCT of increased joint space (r=0.4, p=0.01).
Discussion
Evaluation of TMJ affection is of great value in RA and PSA patients, as it may lead to severe disability [23]. The incidence of TMJ Involvement in RA patients varies greatly from 2-86% [24]; however PsA TMJ involvement has been thought to be rare with fewer than 40 cases reported in the last 50 years [25].
In more than 50% of RA patients are complaining from TMJ problems and it is the last joint to be involved. It is accompanied by various clinical signs and symptoms, among them; pain, limited movements, joint swelling and muscle spasm [26].
In this research, TMJ was affected clinically in 84% of RA and 40% of psoriasis patients. In RA patients, the most frequent clinical TMJ manifestation was TMJ pain on palpation (84%) followed by joint sound (62%), pain with open of mouth (lock) (58%), masticatory pain on palpation (56%), palpable clicking (40%), TMJ pain on movement (32%), fatigue in TMJ (20%), difficult opening of mouth (18%), and jaw rigidity or limited range of mandibular movement (14%). While in psoriasis patients, the most frequent clinical TMJ manifestation was TMJ pain on palpation (40%), followed by lock jaw (24%), masticatory pain on palpation (16%), masticatory muscle pain (12%), TMJ pain on movement (12%), and joint sound (8%).
In agreement with our results Tamer et al. [27] reported symptomatic TMJ involvement in 70.83% of the RA patients, where the most frequent clinical TMJ dysfunction manifestations were difficult manipulation and pain, tenderness (45.83%), clicking (29.17%), and locking (16.67%) followed by altered mouth opening (8.33%). Moreover, Witulski et al. [28] described the common features of TMJ dysfunction in RA patients as follows, joint crepitus (65%) followed by joint pain (60%) and pain on mandibular function and decrease in mouth opening (60%). However, Gopal et al. [29] found features of TMJ dysfunction in lower frequencies than previous studies, where TMJ sound (clicking or crepitus) was found in (7%) of RA patients, followed by pain (3%) and fatigue in TMJ (2%). This difference may be due to the different methods and criteria for recording joint sounds, lack of standardization and different indices used for examination.
As regards TMJ involvement in psoriasis patients, it was varied in different studies. Crincoli et al. [30] found TMJ involvement in 68.8% of psoriasis patients (with "64%" and without PsA "4.8%"). This result differs from that of similar studies by Dervis et al. [1] who found TMJ involvement in 35% and 48% of PsA patients respectively.
Our results proved the relationship between clinical features of TMJ involvement and disease activity, as there were positive correlations of TMJ pain on palpation and masticatory muscle pain on palpation with DAS-28 (ESR) (r=0.4, p=0.01, r=0.4, p=0.01 respectively for RA, r=0.7, p=0.01, r=0.5, p=0.007 respectively for psoriasis patients). In concordance with our findings, Aliko et al. [2] reported that TMJ pain and masticatory muscle tenderness suggest an active RA disease.
In the present study, TMJ affection was detected by US imaging in 36 RA patients (72%). All parameters of TMJ MSUS were higher in right side than in left side [effusion (60%), osteophyte (56%), erosion (50%), and disc displacement (34%) on the right side], and they were correlated with the clinical TMJ dysfunction as there was positive correlation between osteophyte and locking jaw (r=0.31, p=0.03 respectively), and another one between disc displacement and pain of TMJ in movement & impaired range of mandibular movement (jaw rigidity) (r=0.32, p=0.02, r=0.32, p=0.02 respectively). Effusion and erosion were positively correlated with joint sound, locking jaw and masticatory muscle pain (r=0.29, p=0.04, r=0.3, p=0.04, r=0.37, p= 0.008, r=0.45, p=0.001, r=0.32, P=0.02 respectively). In addition, there were positive correlations between ultrasound findings and other disease parameters as a positive correlation between disc displacement and duration of illness (r=0.37, p=0.008), positive correlation between osteophyte and duration of morning stiffness (r=0.31, p=0.03), positive correlation between effusion, duration of morning stiffness and CRP positivity (r=0.35, p=0.01, r=0.33, p=0.02 respectively). However, there were no relationships between ultrasound findings and DAS 28, US 7 score, SENS, ESR, RF positivity, or anti-CCP.
Similarly, Melchiorre et al. [23] evaluated the use of US in assessment of TMJ changes in RA patients and found that 7 (31.8%) of patients with RA showed disc alterations. The disc was noted displaced anteriorly and appeared hypoechoic.
In the present study, involvement of the TMJ was detected by multi-detector computed tomography in 33 RA patients (66%). Irregular articular surface was more in the right side (42%), impaired mouth opening and increased joint space were higher in the left side (26%, 8% respectively), and marginal osteophyte at mandibular condyle was equally found in both sides (20%).
Our results revealed significant correlations between features of multi-detector computed tomography and clinical TMJ dysfunction. There was positive correlation of marginal osteophyte at mandibular condyle and increased joint space with impaired range of mandibular movement (jaw rigidity) (r=0.38, p=0.007, r=0.31, p=0.03 respectively). Irregular articular surface was positively correlated with TMJ pain in palpation, TMJ pain in movement and masticatory muscle pain in palpation (r=0.30, p= 0.03, r=0.29, p=0.04, r=0.34, p=0.02 respectively). Moreover, impaired mouth opening was positively correlated with masticatory muscle pain in palpation (r=0.32, p=0.02).
Goupille et al. [31] stated that a good correlation between clinical symptoms and CT findings of TMJ, in contrary to Axelsson et al. [32] who could not found any correlation between clinical symptoms and CT findings of TMJ changes.
Our results revealed significant correlations between features of multi-detector computed tomography and markers of severity. Impaired mouth opening was positively correlated with RF positivity (r=0.29, p=0.04), and increased joint space was positively correlated with anti- CCP positivity (r=0.36, p=0.01). However, there were no relationships between MDCT features and duration of disease, DAS 28, US 7 score, SENS, or ESR.
Celiker et al. [33] postulated that a great positive relation between CT scan scores and RF positivity. They concluded that, there was a positive correlation between the severity of RA and the severity of involvement in TMJ. Further studies on a larger number of RA and psoriasis patients are recommended to better evaluate the clinical relevance of the available methods for assessing TMJ dysfunction. Finely, we conclude that TMJ involvement is a frequent manifestation of RA and PsA. US evaluation of the TMJ is of great value in assessment of joint effusion and disc displacement in RA and psoriasis patients. MDCT showed high sensitivity and specificity for assessment of TMJ in RA and psoriasis patients.
Conclusion
TMJ is involved frequently in patients with Rheumatoid and Psoriatic arthritis. Clinical and laboratory correlations with the available imaging modalities are essential for accurate estimation of joint affection. MDCT is of high sensitivity and specificity regarding the diagnosis of joint effusion and disc displacement. Also, the severity of TMJ dysfunction was positively correlated with parameters of disease activity and/or severity in RA and psoriasis patients.
References
- Dervis E, Dervis E. The prevalence of temporomandibular disorders in patients with psoriasis with or without psoriatic arthritis. J. Oral. Rehabil. 32(11), 786-793 (2005).
- Aliko A, Ciancaglini R, Alushi A et al. Temporomandibular joint involvement in rheumatoid arthritis, systemic lupus erythematosus and systemic sclerosis. Int. J. Oral. Maxillofac. Surg. 40(7), 704-709 (2011).
- Bessa-Nogueira RV, Vasconcelos BCE, Niederman R. The methodological quality of systematic reviews comparing temporomandibular joint disorder surgical and non-surgical treatment. BMC. Oral. Health. 8(1), 27 (2008).
- Rani S, Pawah S, Gola S et al. Analysis of Helkimo index for temporomandibular disorder diagnosis in the dental students of Faridabad city: A cross-sectional study. J. Indian. Prosthodont. Soc. 17(1), 48-52 (2017).
- Petscavage-Thomas JM, Walker EA. Unlocking the jaw: Advanced imaging of the temporomandibular joint. Am. J. Roentgenol. 203(5), 1047-1058 (2014).
- Bag AK, Gaddikeri S, Singhal A et al. Imaging of the temporomandibular joint: An update. World. J. Radiol. 6(8), 567-582 (2014).
- Talmaceanu D, Lenghel LM, Bolog N et al. Imaging modalities for temporomandibular joint disorders: an update. Clujul. Med. 91(3), 280-287 (2018).
- Ishizuka Y, Shibukawa Y, Nagayama M et al. TMJ Degeneration in SAMP8 Mice is Accompanied by Deranged Ihh Signaling. J. Dent. Res. 93(3), 281-287 (2014).
- Boeddinghaus R, Whyte A. Computed tomography of the temporomandibular joint. J. Med. Imaging. Radiat. Oncol. 57, 448-454 (2013).
- Bas B, Yılmaz N, GÙÂkce E et al. Diagnostic value of ultrasonography in temporomandibular disorders. J. Oral. Maxillofac. Surg. 69, 1304-1310 (2011).
- Aletaha D, Neogi T, Silman AJ et al. Rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. ACR. Open. Rheumatology. 9(62), 2569-2830 (2010).
- Helliwell PS, Taylor WJ. Classification and diagnostic criteria for psoriatic arthritis. Ann. Rheum. Dis. 64(Suppl II), ii3-ii8 (2005).
- Riazzoli J, Nilsson JÅ, Teleman A et al. Patient-reported 28 swollen and tender joint counts accurately represent RA disease activity and can be used to assess therapy responses at the group level. Rheumatology (Oxford). 49(11), 2098-2103 (2010).
- Pereira LJ, Gaviao MB, Bonjardim L et al. Ultrasound and tomographic evaluation of temporomandibular joints in adolescents with and without Signs and symptoms of temporomandibular disorders: a pilot Study. Dentomaxillofac. Radiol. 36(7), 402-408 (2007).
- Maska L, Anderson J, Michaud K. Measures of functional status and quality of life in rheumatoid arthritis: Health Assessment Questionnaire Disability Index (HAQ), Modified Health Assessment Questionnaire (MHAQ), Multidimensional Health Assessment Questionnaire (MDHAQ), Health Assessment Questionnaire II (HAQâ€ÂII), Improved Health Assessment Questionnaire (Improved HAQ), and Rheumatoid Arthritis Quality of Life (RAQoL). ACR. Open. Rheumatology. 63(11), S4-S13 (2011).
- Voshaar OMA, Schenk O, Klooster TPM et al. Further Simplification of the simple erosion narrowing score with item response theory methodology. Arthritis Care Res (Hoboken). 68(8), 1206-1210 (2016).
- Wassenberg S, Fischer-Kahle V, Herborn G et al. A method to score radiographic change in psoriatic. arthritis. J. Rheumatol. 60, 156-166 (2001).
- Helkimo M. Studies on function and dysfunction of the masticatory system IV. Age and sex distribution of symptoms of dysfunction of the masticatory system in Lapps in the north of Finland. Acta. Odontol. Scand. 32(4), 255-267 (1974).
- Pesquera-Velasco J, Casares-García G, Jiménez-Pasamontes N et al. Method of help for the diagnosis of the temporomandibular joint internal derangements. Discriminant analysis applied to the temporomandibular derangements. Med. Oral. Patol. Oral. Cir. Bucal. 10(4), 294-300 (2005).
- Ueki K, Nakagawa K, Takatsuka S et al. Temporomandibular joint morphology and disc position in skeletal class III patients. J. Craniomaxillofac. Surg. 28(6), 362-368 (2000).
- Hayashi T, Ito J, Koyama J et al. The accuracy of sonography for evaluation of internal derangement of the Temporomandibular Joint in Asymptomatic Elementary School Children: Comparison with MR and CT. Am. J. Neuroradiol. 22(4), 728-734 (2001).
- Voog U, Alstergren P, Eliasson S et al. Inflammatory mediators and radiographic changes in temporomandibular joints of patients with rheumatoid arthritis. Acta. Odontol. Scand. 61(1), 57-64 (2003).
- Melchiorre D, Calderazzi A, Bongi SM et al. A comparison of ultrasonography and magnetic resonance imaging in the evaluation of temporomandibular joint involvement in rheumatoid arthritis and psoriatic arthritis. Rheumatology. 42, 673-676 (2003).
- Gleissner C, Kaesser U, Dehne F et al. Temporomandibular joint function in patients with longstanding rheumatoid arthritis - I. Role of periodontal status and prosthetic care - a clinical study. Eur. J. Med. Res. 8(3), 98-108 (2003).
- O’Connor RC, Fawthrop F, Salha R et al. Management of the temporomandibular joint in inflammatory arthritis: Involvement of surgical procedures. Eur. J. Rheumatol. 4(2), 151-156 (2017).
- Ruparelia PB, Shah DS, Ruparelia K et al. Bilateral TMJ involvement in rheumatoid arthritis. Case. Rep. Dent. 1-5 (2014).
- Tamer GMD, Eman A, Shorouk KH et al. Using clinical and multislice computer tomographic features to assess temporomandibular joint osseous involvement in rheumatoid arthritis: a preliminary study. Turk. J. Rheumatol. 27(1), 47-55 (2012).
- Witulski S, Vogl TJ, Rehart S et al. Evaluation of the TMJ by means of clinical TMD examination and MRI diagnostics in patients with rheumatoid arthritis. Biomed. Res. Int. 1-9 (2014).
- Gopal SK, Shankar RS et al. Prevalence of Temporo-mandibular joint disorders in symptomatic and asymptomatic patients: A cross-sectional study. Int. J. Adv. Health. Sci. 1(6) (2014).
- Crincoli V, Di Comite M, Di Bisceglie MB et al. Temporomandibular disorders in psoriasis patients with and without psoriatic arthritis: an observational study. Int. J. Med. Sci. 12(4), 341-348 (2015).
- Goupille P, Fouquet B, Goga D et al. The temporomandibular joint in rheumatoid arthritis: correlations between clinical and tomographic features. J. Dent. 21, 141-146 (1993).
- Axelsson S, Holmlund A, Hjerpe A. Glycosaminoglycans in normal and osteoarthrotic human temporomandibular joint disks. Acta. Odontologica. Scandinavica. 50(2), 113-119 (1992).
- Celiker RY. Gokçe-kutsal, Eryilmaz M. Temporomandibular joint involvement in rheumatoid arthritis: relationship with disease activity. Scand. J. Rheumatol. 24(1), 22-25 (1995).