Case Report - International Journal of Clinical Rheumatology (2019) Volume 14, Issue 5
Acute knee arthritis in psoriasis patient: What ultrasound could tell us?
- Corresponding Author:
- Ahmed Abogamal
Department of Rheumatology Al-Azhar Faculty of Medicine Cairo
Egypt
E-mail: ahmedabogamal@azhar.edu.eg
Abstract
Psoriatic Arthritis (PsA) affects almost 30% of psoriasis (PsO) patients, with different heterogeneous clinical presentations ranging from ethesitis, dactylitis, polyarticular, pauciarticular and axial spondyloarthopathy; causes joints pain in such group of patients always include psoriatic arthritis as a common cause of arthritis in such group, while other causes of joints pain could coexist in PsO patients. The early assessment using musculoskeletal ultrasound in such group could efficiently help in figuring out the cause of joint inflammation and in turn early application of the needed protocol of management.
Keywords
psoriasis • psoriatic arthritis • gout • musculoskeletal Ultrasound
Introduction
Psoriatic Arthritis (PsA) affects almost 30% of psoriasis (PsO) patients, with different heterogeneous clinical presentations ranging from ethesitis, dactylitis, to polyarticular, pauciarticular , and axial spondyloarthopathy; that’s why differential diagnosis of joints pain in any PsO patient must include PsA as the most prevalent diagnosis in such group of patients [1- 3]. Other causes joints pain also could exists in PsO patients like osteoarthritis, gouty arthritis, septic arthritis, and trauma and should be always considered in the differential diagnosis of joints pain in such group of patients [4-6].
Case report
Male patient 26 years old, a known case of psoriasis for 5 years and he have been on a stable doses 300 mg secukinumab monthly for the last two years referred to the rheumatology outpatient clinic with left knee pain. According to his dermatologist notes, he was doing well in the last follow up visits with minimal disease activity, clear skin and no previous complaints of any joint pain. Two days ago he started to develop pain and swelling in his left knee of sudden onset, he denied any trauma or fever. Pain and swelling starts mildly and then progress to be sever and affect his gait with a progressive course.
On examination, there was no regional inguinal lymphadenitis, or fever. Local examination reveals, no erythema over the knee, with tens effusion, moderate tenderness, and limited range of motion. Other joints clinically free, patient was negative for dactylitis and for ethesitis index. Ultrasound assessment show marked distension of the knee joint by hypoechoic displaceable shadow of the effusion, so the diagnosis of monoarthritis has been confirmed with a decision of synovial fluid aspiration.
The advantage of arthrocentesis as a therapeutic and diagnostic procedure has been discussed with the patient and after approval joint aspiration done under ultrasound guidance with drainage of 100 cc yellow turbid, with immediate relief of patient pain; synovial fluid was of low viscosity and sent for further laboratory testing.
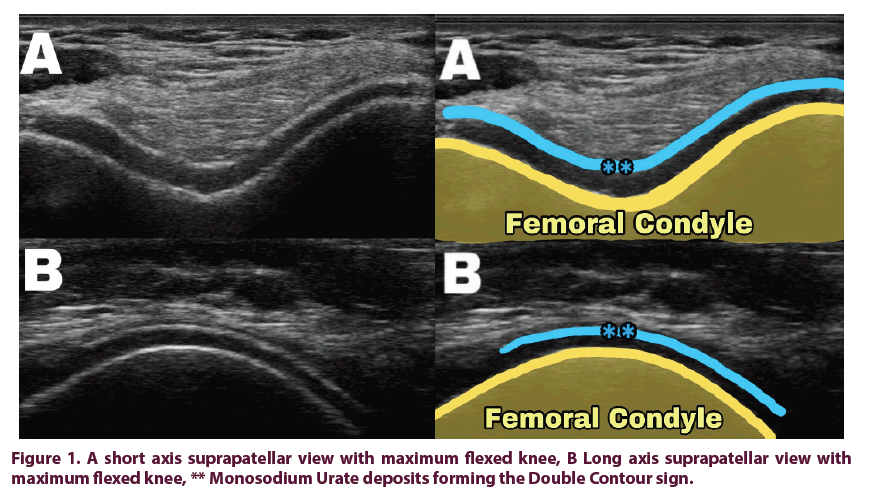
Ultrasound assessment post aspiration, shows mild synovitis in the lateral knee recess, with positive power Doppler grade II, and a hyperechoic white shadow completely overlies the femoral hyaline cartilage surface with signal similar to the subchondral bone signal; a DOUBLE CONTOUR sign which raise the diagnosis of gouty arthritis (Figure 1).
Blood tests results later shows a high ESR 65, CRP 42, serum uric acid 10.2, complete blood picture normal, and three days later the synovial fluid results confirmed the monosodium urate (MSU) crystal presence, and was negative for bacteria with no growth.
Colchicine 0.5 mg twice daily, with Etirocoxib 120 mg once daily was started after the arthrocentesis, and ultrasound results. Four days later after the synovial fluid analysis cleared, patient examined again with partial improvement of pain and swelling; second ultrasound assessment shows mild joint effusion with persistent positive power Doppler signal in the lateral knee recess. Intraarticular corticosteroid injection discussed with the patient and after agreement intra-articular Betamethasone injection done ultrasound guidance, and started Febuxostat 80 mg, with continuation of Colchicine 0.5 mg twice daily, and advice for diet control.
Second follow up visit after four weeks, patient was free of pain and inflammatory markers normalized, CRP 0.4, ESR 10, serum uric acid 5.4, ultrasound assessments of the knee show no effusion, negative power Doppler, with persistence of the Double contour sign. Patient advised to stop Colchicine and continue Febuxostat 80 mg till the next follow up visit.
Discussion
The diagnostic challenge in these patient’s subset that; both PsA and gout can present as an acute monoarthritis, and both PsA and hyperuricemia can coexist in PSO patients. The confirmed diagnosis in such cases usually comes from the recognition of other findings that suggest PsA, such as prominent DIP joint disease, enthesitis, dactylitis, and axial disease would support the diagnosis of PsA; while gout confirmed by detection of MSU crystals in the joint aspirate [5-7].
In our patient negative examination at any other joints at onset of knee pain, and negative evidence of PsA in all previous follow up visits plus the clinical stability on 300 mg secukinumab for the last two years less likely the diagnosis of PsA. Gout diagnosis considerably delayed by the uncertainty about the actual intra-articular presence of monosodium urate crystals; but the ready availability of ultrasonography in our rheumatology outpatient clinic, and the ability for identification of articular abnormalities with high specificity for gout; Double contour sign, helps a lot to shorten the time needed to classify the running joint pathology and setup the diagnosis of gouty arthritis. Furthermore, ultrasound guidance successfully helps to aspirate all the collected synovial fluid, relieve patient pain, and then actual intra-articular placement of Betamethasone to control the inflammation.
With the development of musculoskeletal ultrasound (MSUS) and its introduction in the field of rheumatology; rheumatologists with sufficient training can actually get a lot of significant information about the running joint pathology in a real time examination [8,9]. MSUS can simply take the rheumatologist eye deep enough to visualize all joint areas: tendons, ligaments, cartilage, synovium, vessels, nerves, and even bone cortex [9-11].
In gout; MSU crystals reflect back the ultrasound waves higher than the surrounding articular tissues either the hyaline cartilage or the synovium; and appears as shining bright white in gray scale ultrasound (Figure 1) [12,13]. According to The Outcome Measures in Rheumatology (OMERACT) ultrasound Gout Task Force consensus; MSU deposits can be presented in three different intra-articular forms:
• The double contour sign appearance which describes the deposition of MSU crystals over the surface of the hyaline articular cartilage, which is differentiated from the calcium pyrophosphate crystal deposits, which typically deposited within the articular cartilage (Figure 1) [14].
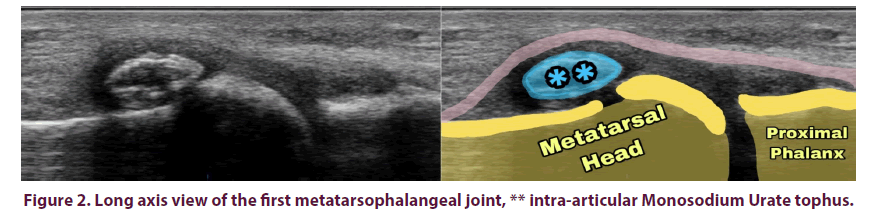
• A gouty intra-articular tophus representing a larger collection of MSU crystals within the inflamed articular soft tissue (Figure 2) [14].
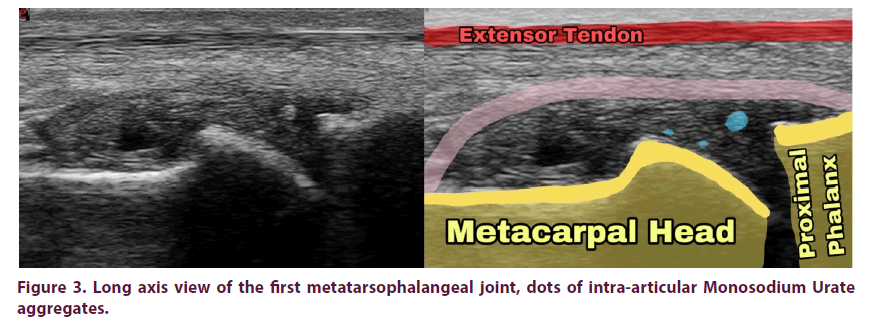
• Gouty aggregates when the collection of crystals in joints or soft tissue not large enough to be defined as a tophus (Figure 3) [14].
The diagnostic value of ultrasound detected MSU deposits has been frequently studied by many researches and confirmed a significant specificity to the presence of gouty arthritis furthermore the double contour sign has been included as a significant parameter in the 2015 ACR/EULAR Gout classification criteria. This promotes the ultrasound to be the important diagnostic tool for gouty arthritis in absence of microscope [14,15].
Furthermore, ultrasound can helpful for follow up disease progression through following the inflammatory signs like effusion, synovitis, power Doppler signals, and also the amount of MSU deposits to judge the treatment response [15,16].
Conclusion
In spite of psoriatic arthritis is the commonest form of arthritis in patients with psoriasis, many other causes could be attributed for arthritis including gouty arthritis, and ultrasound detection of MSU deposits in such cases very helpful for early classification of the cause of arthritis, early treatment, and rapid relieve of pain and inflammation.
Patient consent
Written consent taken from the patient for approval of publishing his case scenarios, clinical, laboratory, and images.
Conflict of interest
The author declares that no any potential conflict of interest that might constitute an embarrassment related to this publication.
References
- Brockbank J, Gladman D. Diagnosis and management of psoriatic arthritis. Drugs. 62(17), 2447–2457 (2002).
- Shbeeb M, Uramoto KM, Gibson LE et al. The epidemiology of psoriatic arthritis in Olmsted County, Minnesota, USA, 1982–1991. J. Rheumatol. 27(5), 1247-1250 (2000).
- Madland TM, Apalset EM, Johannessen AE et al. Prevalence, disease manifestations, and treatment of psoriatic arthritis in Western Norway. J. Rheumatol. 32(10), 1918–1922 (2005).
- Guidelines for the initial evaluation of the adult patient with acute musculoskeletal symptoms. American College of Rheumatology Ad Hoc Committee on Clinical Guidelines. Arthritis. Rheum. 39(1), 1–8 (1996).
- Mohana-Borges AV, Chung CB, Resnick D. Monoarticular arthritis. Radiol. Clin. North. Am. 42(1), 135–149 (2004).
- Schumacher HR, Habre W, Meador R et al. Predictive factors in early arthritis: long-term follow-up. Semin. Arthritis. Rheum. 33(4), 264–272 (2004).
- Swan A, Amer H, Dieppe P. The value of synovial fluid assays in the diagnosis of joint disease: a literature survey. Ann. Rheum. Dis. 61(6), 493–498 (2002).
- Kane D, Grassi W, Sturrock R, Balint PV. Musculoskeletal ultrasound--a state of the art review in rheumatology. Part 2: Clinical indications for musculoskeletal ultrasound in rheumatology. Rheumatology (Oxford). 43(7), 829–838 (2004).
- McAlindon T, Kissin E, Nazarian L et al. American College of Rheumatology report on reasonable use of musculoskeletal ultrasonography in rheumatology clinical practice. Arthritis. Care. Res (Hoboken). 64(11), 1625–1640 (2012).
- Backhaus M, Burmester GR, Gerber T et al. Guidelines for musculoskeletal ultrasound in rheumatology. Ann. Rheum. Dis. 60(7), 641–649 (2001).
- Balint PV, D'Agostino MA. Spondyloarthritis: a journey within and around the joint. Rheumatology (Oxford). 51(Suppl 7), 13–17 (2012).
- Chowalloor PV, Keen HI. A systematic review of ultrasonography in gout and asymptomatic hyperuricaemia. Ann. Rheum. Dis. 72(5), 638–645 (2013).
- Fodor D, Nestorova R, Vlad V et al. The place of musculoskeletal ultrasonography in gout diagnosis. Med. Ultrason. 16(4), 336–344 (2014).
- Gutierrez M, Schmidt WA, Thiele RG et al. International Consensus for ultrasound lesions in gout: results of Delphi process and web-reliability exercise. Rheumatology (Oxford). 54(10), 1797–1805 (2015).
- Neogi T, Jansen TL, Dalbeth N et al. Gout classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann. Rheum. Dis. 74(10), 1789–1798 (2015).
- Christiansen SN, Ostergaard M, Terslev L. Ultrasonography in gout: utility in diagnosis and monitoring. Clin. Exp. Rheumatol. 114(5), 61–67 (2018).