Case Report - Interventional Cardiology (2021) Volume 13, Issue 4
Acute anterior ST elevation myocardial infarction caused by paradoxical embolus in young patient having PFO
- Corresponding Author:
- Yousif Abusalma
Department of Cardiology,
Sandwell and West Birmingham NHS Trust,
Birmingham,
England,
United Kingdom,
E-mail: yousif.abusalma@nhs.net
Received date: June 08, 2021; Accepted date: June 22, 2021; Published date: June 29, 2021
Abstract
Introduction and background: Coronary thromboembolic phenomenon can be the main pathophysiology in up to 3%-7% of acute coronary syndromes presentation. However, many times it is missed in the differential diagnosis of acute coronary syndromes. Paradoxical coronary artery embolism is a rare cause of acute myocardial infarction, and it should be thought of in patients presenting with myocardial infarction with low risk profile for atherosclerotic coronary artery disease.
Case summary: A 25-year-old woman presented with severe cardiac sounding chest pain. Her ECG confirmed ST elevation in the anterior precordial leads, elevated cardiac enzymes and apical, apicolateral hypokinesia with preserved Left Ventricular Systolic Function (LVSF) on transthoracic echocardiogram. Coronary angiogram revealed at the time distal Left Anterior Descending (LAD) artery blockage with TIMI I flow. Subsequent cardiac Computed Tomography Coronary angiogram (CTCA) 48 hours later on revealed normal good flow in the distal LAD.
Conclusion and learning points:
• This case puts the emphasis on the rare causes of acute myocardial infarction in a patient with a PFO which led to paradoxical coronary artery embolization.
• Coronary artery embolism is well recognised aetiology of Acute Coronary Syndrome (ACS), but paradoxical coronary artery embolism is seldomly observed. Hence, a high index of clinical suspicion is required for this diagnosis.
• Indeed, reaching the right diagnosis in such condition is crucial. The right diagnosis would influence management and prognosis, as it would entail closure of the defect to prevent further catastrophic events.
Keywords
ST-elevation myocardial infarction • Acute coronary syndrome•` Paradoxical thromboembolism • Coronary artery thrombosis
Introduction
We describe a case of paradoxical coronary artery embolism causing ST elevation myocardial infarction in setting of Patent Foramen Ovale (PFO). There are still no clear guidelines for the management of embolic myocardial infarction. Percutaneous device closure of the patent foramen ovale should be considered to in the management plan in order to prevent future embolic events.
Case Presentation
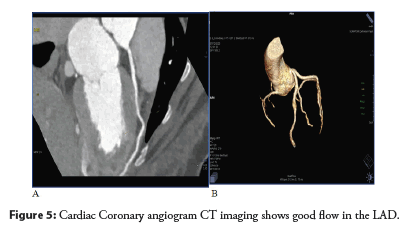
A 25-year-old woman presented with severe cardiac sounding chest pain. Her ECG confirmed ST elevation in the anterior precordial leads, elevated cardiac enzymes and apical, apicolateral hypokinesia with preserved Left Ventricular Systolic Function (LVSF) on transthoracic echocardiogram. Coronary angiogram revealed at the time distal Left Anterior Descending (LAD) artery blockage with TIMI I flow. Subsequent cardiac Computed Tomography Coronary angiogram (CTCA) 48 hours later on revealed normal good flow in the distal LAD [1-5].
Chief complaints
Central chest pain radiating to both arms and the back associated with 3 hours of vomiting.
History of present illness
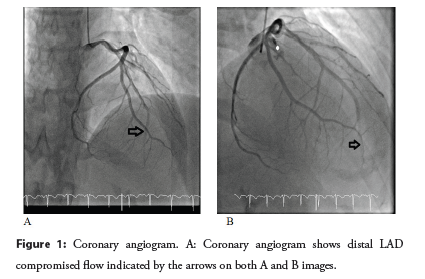
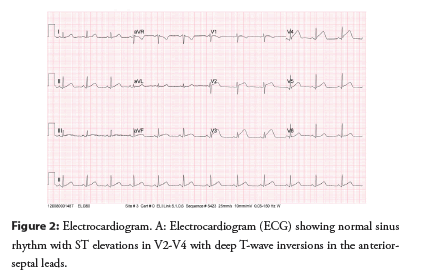
A 25-year-old female non-UK resident presented with central heaviness radiating to both arms and the back which started 5 hours prior to her presentation. This was associated with a history of vomiting for 3 hours. The pain lasted till morphine was administered in the Emergency Department (ED). Her electrocardiogram (ECG) demonstrated sinus rhythm with ST elevation, more pronounced in anterior-lateral precordial leads. Her focused bed side transthoracic echocardiogram (TTE) in the ED highlighted hypokinesia of most of the apical segments. Subsequently she underwent urgent coronary angiography which revealed widely patent right coronary artery (RCA) and Left Circumflex Artery (LCX) but had a sub-total distal occlusion of the distal LAD with TIMI I flow (Figure 1) [1-5].
Figure 1: Coronary angiogram. A: Coronary angiogram shows distal LAD compromised flow indicated by the arrows on both A and B images.
History of past illness
The patient had no previous medical history.
Physical examination
The patient’s heart rate was 83 bpm, respiratory rate was 17 breaths per minute, blood pressure was 97/62 mmHg and oxygen saturation on room air was 98%. The clinical cardiac examination revealed a regular rate and rhythm with no added sounds, and no jugular venous distention. Lung examination revealed clear breath sounds without crackles.
Laboratory examinations
• ECG performed by the ambulance crew and in ED showed sinus rhythm with ST elevations in V3-V5 (Figure 2).
• Cardiac enzymes at the time of presentation (5 hours post symptom onset) revealed high sensitivity troponin I level of 140 ng/L but the subsequent repeat test at 24 hours was significantly elevated at >50,000 ng/L.
• COVID-19 PCR test was negative twice.
• Chest X-ray and arterial blood gas were normal.
Imaging examinations
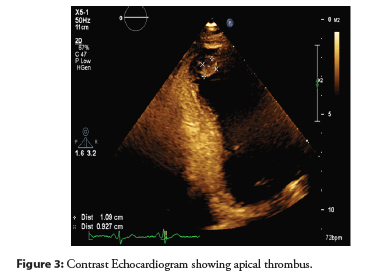
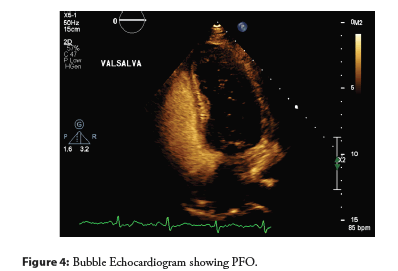
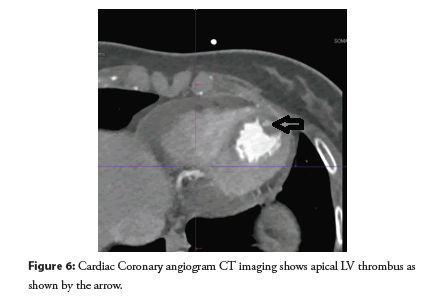
The departmental TTE revealed evidence of wall motion abnormality with hypokinesia in the whole area of the apex and mid inferoseptal Left ventricular ejection fraction estimated at 40%-45%. Although there was no obvious apical thrombus it wasn’t fully excluded. Repeat echocardiogram with contrast confirmed the presence of LV apical thrombus (measuring 1.45 cm × 1.33 cm) (Figure 3) in addition, she underwent Bubble echocardiography study which was positive with in the first 2 cycles suggesting the presence of a small PFO (Figure 4).
Coronary angiography showed widely patent RCA and LCX. The LAD artery was widely patent proximally but had a sub-total distal occlusion with TIMI I flow (Figure 4). The initial impression was possible Spontaneous Coronary Artery Dissection (SCAD). Cardiac CT Coronary angiography performed 48 hours after the angiography revealed patent LAD with normal flow (Figure 5). It was discussed in the CTCA MDT and the consensus was an acute MI secondary to thromboembolic phenomenon with presence of LV apical thrombus (Figure 6).
Figure 5: Cardiac Coronary angiogram CT imaging shows good flow in the LAD.
Figure 6: Cardiac Coronary angiogram CT imaging shows apical LV thrombus as shown by the arrow.
Multidisciplinary cardiothoracic meeting
The discussion concluded that a CTCA be performed to see if there was healing of the questionable SCAD and to assess the flow down the LAD. Discussion also occurred about what optimal antiplatelet and anticoagulation therapy.
Further diagnostic work-up and other speciality consultations
Given the presentation and the ambiguity of whether she had a paradoxical embolus, she underwent further blood test evaluation under the guidance of the Haematology team who advocated the following blood tests: autoantibodies, antiphospholipid screen, immunoglobulin levels along with JACK2 mutation-all of which came back negative. Lupus anticoagulant was weakly positive. Doppler-ultrasound of the leg ruled out Deep Vein Thrombosis (DVT).
Final diagnosis
The final diagnosis of this case is Acute ST elevation myocardial infarction caused by coronary embolism secondary to paradoxical embolus due to the presence of PFO.
Treatment
The patient has been initiated on Warfarin therapy given her LV thrombus. Furthermore, due to the positive bubble-echo study, the patient has been referred to a tertiary hospital for PFO closure consideration although she would need long term anticoagulation anyway for the LV thrombus.
Outcomes and follow-up
The patient was relatively pain free after the coronary angiogram with significant resolution of her ST elevation without any mechanical intervention. Subsequently she was shifted to the Coronary Care Unit (CCU) and treated conservatively, remaining stable throughout the rest of her hospital course. She has been referred to a tertiary hospital for PFO closure and she will undergo regular follow up in our Cardiology clinic.
Results and Discussion
We present this rare case of paradoxical embolus leading to acute myocardial infarction in young lady with significant apical infarction proven with massive troponin release along with reduction in the LV ejection fraction. This is in the setting of an undiagnosed PFO.
Coronary embolism should be considered in all cases of AMI in young adult patients without risk factors for atherosclerotic coronary artery disease. It has been well recognized in literature that the differential diagnosis of AMI in a young adult has wide arrays include vasculitis, coronary artery embolization, vasospasm, SCAD, congenital coronary anomalies, Takotsubo (or stress-induced) cardiomyopathy [6,7]. In this particular case, the differential diagnosis has been narrowed down to SCAD and thromboembolic phenomenon. Characterization of the nature of the events was explored with CTCA which in fact didn’t show evidence of SCAD. The fact that the flow normalized in less than 48 hours supported the diagnosis of embolus rather than healed SCAD as the latter usually takes longer to heal.
Due to the well-established Grown Up with Congenital Heart disease (GUCH) programs across the country, early pick up and meticulous follow up of simple cases of congenital heart disease such as PFOs, ventricular and atrial septal defects has occurred. This has also led to potential early intervention and appropriate anticoagulation. However, there are still occasional cases which did not have an early diagnosis such as in our patient. In fact, our patient is a non-UK resident without any past medical history. Moreover, if we had been aware about her PFO at the time of such unique presentation, we would have appropriately categorized her differential diagnosis. Therefore, it is quite often, such cases which are missed and underdiagnosed in the real world unless someone looks carefully for a thromboembolic event.
The detailed work-up to find a source for the embolism is usually a trigger for further investigation to look for a shunt, PFO, arrhythmias (e.g., atrial fibrillation) or a congenital abnormality. Once an established cause such as a PFO has been confirmed, it undoubtedly warrants discussion of PFO closure consideration. Particularly, this has been backed up with the results of recent randomised trials such as (PROSPECT), (Gore REDUCE) and (DEFENSE-PFO) in reducing systemic embolization incidences [8,9].
Conclusion
Paradoxical embolization is an important differential in young patients presenting with an AMI and a PFO must be ruled out in the differential diagnosis.
References
- Raphael CE, Heit JA, Reeder GS, et al. Coronary embolus: An underappreciated cause of acute coronary syndromes. JACC Cardiovasc Interv. 11(2): 172-180 (2018).
- Murthy A, Shea M, Karnati PK, et al. Rare case of paradoxical embolism causing myocardial infarction: successfully aborted by aspiration alone. J Cardiol. 54(3): 503-6 (2009).
- Popovic B, Agrinier N, Bouchahda N, et al. Coronary embolism among ST-segment-elevation myocardial infarction patients: Mechanisms and management. Circ Cardiovasc Interv. 11(1): e005587 (2018).
- Hakim FA, Kransdorf EP, Abudiab MM, et al. Paradoxical coronary artery embolism-a rare cause of myocardial infarction. Heart Views. 15(4): 124-6 (2014).
- Alenezi AR, Alanbaei M, Abouelenein I. Acute myocardial infarction secondary to paradoxical embolism. Eur J Case Rep Intern Med. 7(12): 001951 (2020).
- Acute coronary manifestations of fibromuscular dysplasia: Spontaneous coronary artery dissection. (2017).
- Sondhi S, Negi PC, Asotra S, et al. Acute ST-segment elevation myocardial infarction in an adolescent-Cryptogenic origin. IHJ Cardiovascular Case Reports (CVCR). 2(3): 143-48 (2018).
- Giblett JP, Abdul-Samad O, Shapiro LM, et al. Patent foramen ovale closure in 2019. Interv Cardiol. 14(1) 34-41: (2019).
- Wasek WC, Samul W, Ryczek R, et al. Unique case of ST-segment-elevation myocardial infarction related to paradoxical embolization and simultaneous pulmonary embolization: Clinical considerations on indications for patent foramen ovale closure in no-guidelines land. Circulation. 131(13): 1214-23 (2015).