Case Report - Imaging in Medicine (2018) Volume 10, Issue 2
A rare complication of acute cholecystitis leading to perihepatic abscess: gall bladder perforation
Yavuz Yuksel1*, Ozkan Ozen2 and Ali Gok3
1lanya AlaaddinKeykubat University, Turkey
2Alanya Training and Research Hospital, Turkey
3Department of Radiology, Alanya, Antalya, Turkey
- *Corresponding Author:
- Yavuz Yuksel
Alanya AlaaddinKeykubat University
Turkey
E-mail: yavuz3215@hotmail.com
Abstract
Background: Gallbladder perforation secondary to cholecystitis are rarely seen. Gallbladder perforation is associated with intra or extra-hepatic abscesses and peritonitis and is high mortality rates. We report a case of gallbladder perforation.
Case presentation: An 80 year old male patient was admitted to our hospital with abdominal pain. The aspartate aminotransferase, alanine aminotransferase and C-reactive protein values of the patient were high. The patient underwent intravenous contrast-enhanced abdominal computed tomography. Abdominal computed tomography showed a hydropic gallbladder, loculated fluid collections surrounding the liver and an increase in the gallbladder wall thickness. There was also defect in fundus of the gallbladder. The patient was operated based on clinical and radiological findings. Operative findings confirmed preoperative radiological findings.
Conclusion: Gallbladder perforation is rare but in such cases early diagnosis is of vital importance. Ultrasonography and computed tomography are the imaging modalities for the diagnosis of gallbladder perforation.
Keywords
▪acute cholecystitis ▪ gallbladder perforation ▪ computed tomography ▪ ultrasonography
Introduction
Gallbladder perforation, which is a rare, but life-threatening complication of acute cholecystitis can be rarely diagnosed preoperatively, despite advanced radiological imaging modalities such as ultrasonography and computed tomography. In case of late diagnosis, it is associated with increased mortality and morbidity rates [1]. About 4-12% of acute cholecystitis cases develop severe complications requiring surgery [2-4]. As the mortality rate is up to 16% in patients with gallbladder perforation, early diagnosis is of vital importance [1]. Herein, report an 80 year old male patient who was admitted with abdominal pain and diagnosed with acute cholecystitis due to biliary sludge and who developed gallbladder perforation and a diffuse perihepatic abscess within 48 h after admission.
■Case presentation
An 80 year old male patient was admitted to our hospital with abdominal pain for 3 to 4 days. Physical examination revealed tenderness to palpation of the right upper quadrant and epigastric region. Laboratory test results were as follows: aspartate aminotransferase (AST) 131 IU/L, alanine aminotransferase (ALT) 87IU/L, C-reactive protein (CRP) 24 mg/L and white blood cells 13.500 cells/mm3. The other test results were within normal ranges. Ultrasonography showed a gallbladder diameter of 34 mm in the axial plane. There was also biliary sludge in the biliary lumen and diffuse increased thickness of gallbladder wall (up to 4.9 mm). In addition, intraluminal membranous structures in the gallbladder and fluid in the perihepatic space were observed. The patient was diagnosed with acute cholecystitis and hospitalized. Medical treatment was initiated. As the clinical status remained unchanged within 48 h of hospitalization, ultrasonography was performed, which showed perihepaticloculated fluid in addition to existing symptoms. The patient, then, underwent intravenous contrastenhanced abdominal computed tomography.
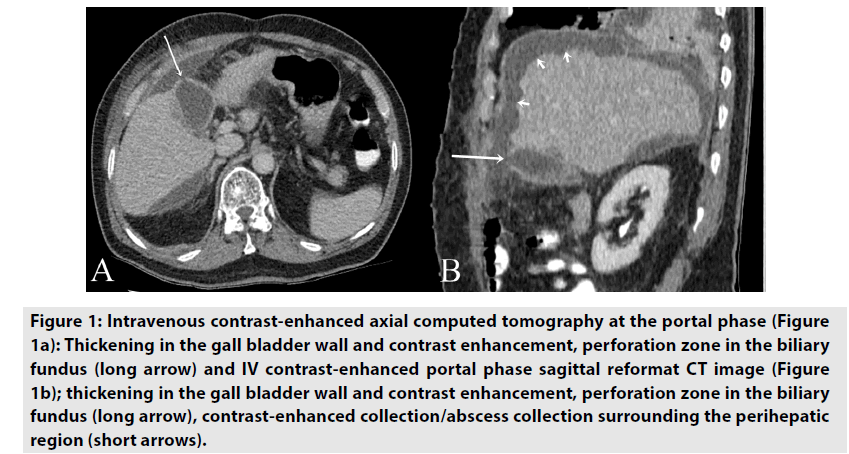
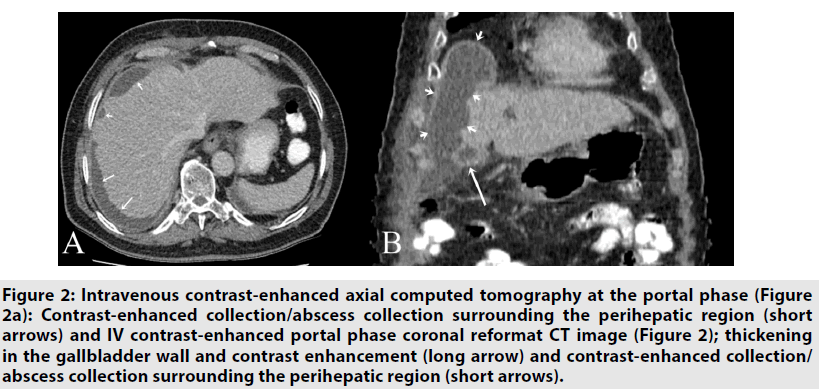
Abdominal computed tomography showed a hydropic gallbladder and 41 mm in size in the axial plane. There was also an increase in the gallbladder wall thickness up to 6 mm with defect in fundus of the gallbladder. In addition, there were loculated fluid collections surrounding the liver and parenchyma with local compression extending toward the subdiaphragmatic space, which reached up to 17 mm in the thickest section with contrast enhancement in the adjacent tissues and which were compatible with abscess (FIGURES 1 & 2). There was an increased contrast enhancement in the arterial phase in the areas adjacent to the capsule of the right hepatic lobe and parenchymal spaces adjacent to the gallbladder bed, which was suggestive of parenchymal inflammation.
Figure 1. Intravenous contrast-enhanced axial computed tomography at the portal phase (Figure 1a): Thickening in the gall bladder wall and contrast enhancement, perforation zone in the biliary fundus (long arrow) and IV contrast-enhanced portal phase sagittal reformat CT image (Figure 1b); thickening in the gall bladder wall and contrast enhancement, perforation zone in the biliary fundus (long arrow), contrast-enhanced collection/abscess collection surrounding the perihepatic region (short arrows).
Figure 2.Intravenous contrast-enhanced axial computed tomography at the portal phase (Figure 2a): Contrast-enhanced collection/abscess collection surrounding the perihepatic region (short arrows) and IV contrast-enhanced portal phase coronal reformat CT image (Figure 2); thickening in the gallbladder wall and contrast enhancement (long arrow) and contrast-enhanced collection/ abscess collection surrounding the perihepatic region (short arrows).
In the fundus of the gallbladder, there was a defective image in the anterior plane, suggesting gallbladder perforation (FÄ°GURES 1A & 1B). A written informed consent was obtained from the patient and the patient was operated based on clinical and radiological findings. The patient underwent open cholecystectomy. Intraoperative findings confirmed preoperative radiological findings, which showed that the gallbladder wall was thick and edematous suggesting gallbladder perforation at fundus with purulent fluid in the surrounding hepatic tissues. During follow-up, the patient remained stable and was discharged with full recovery on postoperative Day 11.
Discussion
About 4 to 12% of acute cholecystitis cases develop complications such as empyema, gall bladder perforation, and gangrenous cholecystitis [2-4]. The mortality rate varies from 12 to 16% in patients with gallbladder perforation, which is typically associated with gallstones [1]. In the present case, ultrasonography showed biliary sludge; however, ultrasonography and computed tomography did not show a gallstone.
In addition, systemic diseases such as diabetes mellitus, traumas, malignancies, infections, and corticosteroids are known as predisposing factors for gallbladder perforation [4]. Elderly patients are also at an increased risk for gallbladder perforation, as in our case [5]. According to the Niemeier’s classification, there are three types of gallbladder perforations: Type I- acute free perforation into the peritoneal cavity; Type II- subacute perforation with pericholecystic abscess; and Type III- chronic perforation with cholecystoenteric fistula [6]. The subacute type has been more frequently reported in the literature. Similarly, in our case, symptoms were compatible with Type II (subacute type).
Distension of the gallbladder and increased intraluminal pressure secondary to acute cholecystitis prevent lymphatic and venous drainage, leading to perforation of the gallbladder wall [7,8]. The fundus part, which is less perfused than the other parts of the gallbladder, is the most common site of gallbladder perforation [4]. In the present case, computed tomography showed a noncontrast enhanced defective site, suggesting fundus perforation and it was confirmed intraoperatively. Sovia et al. [9] reported that distension of the gallbladder and edeme in the gallbladder wall might be early indicators of high-risk for gallbladder perforation. Using computed tomography and ultrasonography, focal interruption of the gallbladder wall, complex pericholecystic fluid and biliary lumen inside or near the pericholecystic abscess may be suggestive of perforation [10]. In our case, there was increased wall thickness of the gallbladder and peripheral contrast-enhanced abscess in the perihepatic space compressing the liver. However, as in our case, the presence of non-enhanced defective image in the gallbladder wall, as assessed by computed tomography, was the most reliable sign for gallbladder perforation [11].
Acute cholecystitis is a serious condition which may cause gallbladder perforation and increase mortality, particularly in elderly. Ultrasonography and computed tomography are the main imaging modalities for the diagnosis of gallbladder perforation. In our case, we detected gallbladder perforation early during clinical follow-up. Interestingly, a large perihepatic abscess formation was observed within 48 h. We believe that early diagnosis and emergent surgery were the main indicators of discharge with full recovery in our case.
Conclusion
Although a rare complication, clinicians should recognize this entity and it should be kept in mind that early diagnosis and emergent surgery are of vital importance.
Competing interests approval
The authors declare no competing interest.
References
- Simmons TC, Miller C, Weaver R. Spontaneous gall bladder perforation. Am. Surg. 55, 311-313 (1989).
- Isch J, Finneran JC, Nahrwold DL. Perforation of the gall bladder. Am. J. Gastroenterol. 55, 451-458 (1971).
- Bennet GL, Balthazar EJ. Ultrasound and CT evaluation of emergent gallbladder pathology. Radiol. Clin. N. Am. 41, 1203-1216 (2003).
- Strohl EL, Diffenbaugh WG, Baker JH et al. Collective reviews: Gangrene and perforation of the gallbladder. Int. Abstr. Surg. 114, 1-7 (1962).
- Martin JD Jr, Stone HH. Perforations of the gallbladder: A report of three cases. Geriatrics. 12, 476-480 (1957).
- Neimeier OW. Acute free perforation of gall bladder. Ann. Surg. 99, 922-944 (1934).
- Glenn F, Moore SW. Gangrene and perforation of the wall of the gallbladder. Arch. Surg. 44, 677-686 (1942).
- Madrazo BL, Francis I, Hricak H et al. Sonographic findings in perforation of the gall bladder. AJR. Am. J. Roentgenol. 139, 491-496 (1982).
- Soiva M, Pamilo M, Paivansalo M et al. Ultrasonography in acute gall bladder perforation. Acta. Radiol. 29, 41-44 (1988).
- Gore RM, Yaghmai V, Newmark GM et al. Imaging benign and malignant disease of the gall bladder. Radiol. Clin. N. Am. 40, 1307-1323 (2002).
- Sood BP, Kalra N, Gupta S et al. Role of sonography in the diagnosis of gallbladder perforation. J. Clin. Ultrasound. 30, 270-274 (2002).