Case Report - Interventional Cardiology (2017) Volume 9, Issue 1
Whether or not to perform percutaneous coronary intervention (PCI) on sub-acute coronary occlusion in patients late after myocardial infarction
- Corresponding Author:
- João Lucas O’Connell
Department of Cardiology, Federal University of Uberlandia
Tel: +5534996651159
E-mail: oconnelljl@me.com
Submitted: 10 January 2017; Accepted: 17 January 2017; Published online: 23 January 2017
Abstract
Despite the almost instinctive tendency of interventional cardiologists to try to reopen important coronary vessels occluded for more than 12 hours post an Acute Myocardial Infarction (AMI), there are several important studies in literature that show no benefit in percutaneous treatment over that of optimized medical therapy regarding general mortality, reinfarction, or heart failure for patients with sub-acute coronary artery occlusion (from more than 12 hours to less than 3 months after an index AMI). The conclusion of prior studies not only demonstrates no benefit, but also the harm that can be caused by this conduct because of its greater tendency towards re-infarction in the group submitted to the intervention (angioplasty with or without stent implantation). Despite this evidence, most interventional cardiologists believe that an attempt at recanalization should be made on patients with a large extent of myocardial viability.
Keywords
Sub-acute coronary occlusion; Percutaneous coronary intervention; Myocardial viability
Introduction
Despite the almost instinctive tendency of interventional cardiologists to try to reopen important coronary vessels occluded for more than 12 h post an Acute Myocardial Infarction (AMI). There are several important studies in literature that show no benefit in percutaneous treatment over that of optimized medical therapy regarding general mortality, reinfarction, or heart failure for patients with sub-acute coronary artery occlusion (from more than 12 h to less than 3 months after an index AMI). The conclusion of prior studies not only demonstrates no benefit, but also the harm that can be caused by this conduct because of its greater tendency towards re-infarction in the group submitted to the intervention (angioplasty with or without stent implantation) [1]. Despite this evidence, most interventional cardiologists believe that an attempt at recanalization should be made on patients with a large extent of myocardial viability [2]. We describe a case (similar to many cases in our daily practice) that illustrates the possible threatens and benefits in trying to open a coronary artery occluded for more than 12 h.
Case Report
We present a case of a 45 year-old male patient (JXS), with a history of type 2 diabetes, obesity, hypertension, and smoking, who recently suffered a burning thoracic pain which irradiated to his back and which was triggered by physical exertion. He was taking Enalapril 5 mg/day and Metformin 500 mg/day before his arrival. He was attended at the Secondary Care Unit of the Unified Public Health System in the city of Uberlandia, Brazil. The electrocardiogram performed at his arrival showed ST segment elevation in the inferior wall (DII, DIII, aVF) and the blood exam evidenced changes in myocardial necrosis markers (Troponin and CKmb). He was not submitted to primary coronary reperfusion methods due to logistic limitations. It was given Aspirin 100 mg/ day, Clopidogrel 75 mg/day, Atenolol 25 mg (twice daily), Enalapril 10 mg (twice daily), Rosuvastatin 20 mg/day and prophylactic Enoxaparin (40 mg/day).
During the period in which he was awaiting transfer to a Tertiary Unit, he remained asymptomatic and stable. Because of logistic limitations, he stayed as an inpatient at the Secondary Unit and was sent for coronary angiography only on the 10th day after AMI. Although this time delay is not the best approach for an AMI patient, it is common for a lot of patients that depend in the public health system in our country. The electrocardiogram taken after his admission to the Tertiary Hospital presented an electrically inactive area in the inferior wall, with no signs of acute injury or ischemia.
Intervention
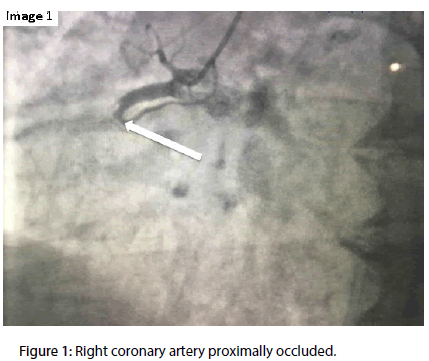
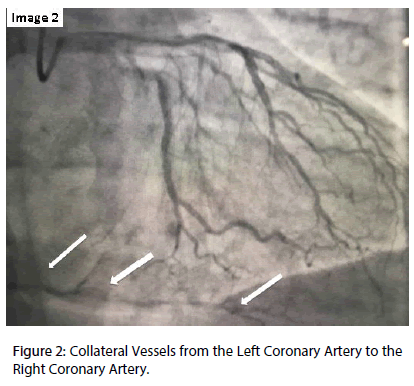
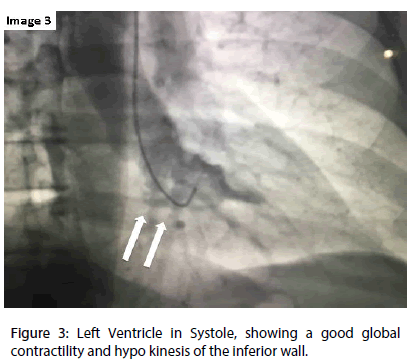
The diagnostic procedure was performed, through the radial artery, 10 days after the index AMI and demonstrated one vessel coronary disease with a total occlusion of the proximal right coronary artery (RCA) (Figure 1), having moderate-grade collaterals arising from the left coronary artery (Figure 2), and also a left ventricle with preserved function and lower basal hypo kinesis (Figure 3).
Figure 1: Right coronary artery proximally occluded.
Figure 2: Collateral Vessels from the Left Coronary Artery to the Right Coronary Artery.
The patient was stable, had a very high intra-right coronary thrombotic load and presumable extensive viability of the inferior wall of the left ventricle (LV) (evidenced by the almost normal contraction of this portion of the LV). The global Ejection Fraction of the LV (LVEF) was normal (> 60%). Thus, it was decided to maintain the patient taken Aspirin, Clopidogrel, Rosuvastatin, Atenolol and Enalapril (at the same doses described before), and to initiate complete anti-coagulation with Enoxaparin (1 mg/kg 12/12 h for 5 to 7 days).
A new coronary angiography was performed 5 days after the first exam, also through the radial artery and showed the same RCA proximal obstruction. Seeing that there was a presumption of viability by the identification of inter-coronary collaterals and good contractility in the inferior wall, a choice was made for the use of RCA angioplasty using a balloon for the predilation of the lesion.
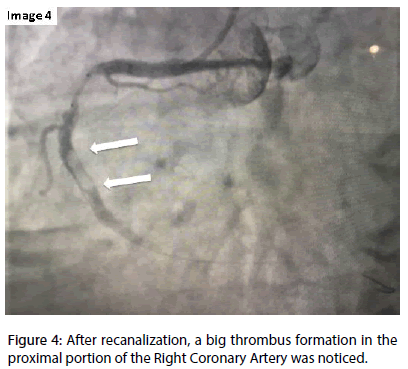
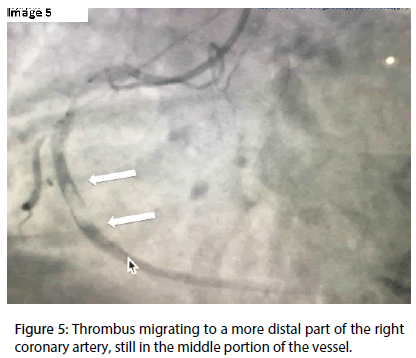
After the reopening of the vessel, the presence of a very large thrombus with distal migration through the RCA was observed (Figures 4 and 5).
Figure 4: After recanalization, a big thrombus formation in the proximal portion of the Right Coronary Artery was noticed.
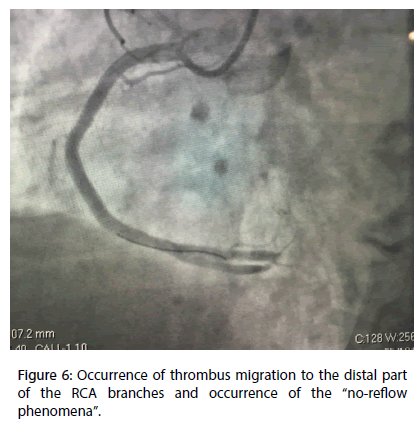
There was an occurrence of a complete cloth blockage of the RCA branches and the installation of the “no-reflow phenomena” (Figure 6).
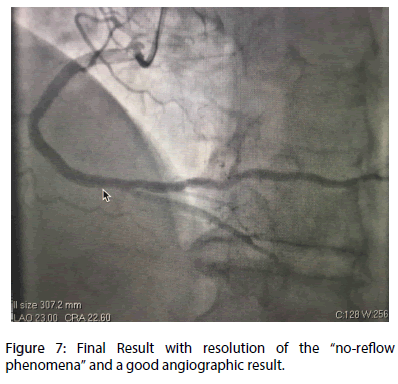
The non-occurrence of a distal reflow was associated with important clinical and hemodynamic instability, as well as the presence of complete AV block and bradycardia. The patient’s condition improved after the use of intravenous NaCl 0.9%, atropine, and then (after clinical and hemodynamic status improvement), the use of intracoronary mononitrate, adenosine and tirofiban. We also maintained the intravenous use of tirofiban for 12 hours after the end of the procedure. After improvement in the coronary flow, we implanted two 4 × 24 mm Omega® bare metal stents (Boston Scientific) involving the proximal and middle portion of the RCA. There was a good angiographic result and a good coronary flow at the end of the procedure (TIMI 3 flow, intra-myocardial grade 2 Blush classification) (Figure 7).
After the procedure, the patient improved clinically and hemodynamically without electrocardiographic alterations, but with a slight elevation of cardiac markers (CKmb: 62, upper limit of 25 U/L). He was discharged for outpatient follow-up 2 days after the percutaneous intervention, asymptomatic for mild activity in the hospital infirmary. He remains asymptomatic and without any new cardiovascular event, 9 months after the index AMI. The contractility of the inferior wall of the LV and its global function also improved.
Discussion
This case illustrates a situation of total sub-acute occlusion of the right coronary artery that arrived at our Interventional Cardiology Unit (tertiary hospital) for coronary angiography 10 days after the onset of the index AMI. The patient was asymptomatic, stable and without significant changes at the time of arrival at the hospital.
It is very well known that early reperfusion reduces mortality from acute myocardial infarction (AMI) [3]. Also, patients with sub-acute coronary occlusions who manifests angina after AMI or who suffer other severe ischemic equivalents (such as pulmonary congestion or hypotension possibly related to myocardial ischemia, frequent ventricular arrhythmias, 2nd or 3rd degree atrium-ventricular blockages, and others, are generally submitted to coronary recanalization by most professionals. Due to clinical, hemodynamic or electrical instability, the recanalization procedure is usually performed immediately after coronary angiography in most of these cases3.
However, the role of late opening of the totally occluded infarct-related artery days post MI, in a stable and asymptomatic patient has remained controversial1. Also, the ideal time to promote recanalization (whether immediately after elective coronary angiography or a few days after diagnosis) is not well established. There is also controversy about the use of other strategies to facilitate the recanalization of the vessel: anti-platelets, anti-coagulants, intra-coronary thrombolytic, IIb-IIIa glycoprotein inhibitors, intra-coronary filters or other devices [3]
There are several arguments to defend the attempt to restore the natural coronary flow to the totally blocked artery. It is commonly accepted that the recanalization procedure could improve the coronary flow and preserve the myocardium from possible ischemic injury when the patient returns to his usual activities, which require greater physical effort than that of the myocardial demand in the period of hospitalization. Thus, the procedure could prevail patients from angina or myocardial hibernation (decreased myocardial contractility secondary to chronic hypo perfusion). Opening the vessel could also promote reduction in adverse left ventricular (LV) remodelling [2,4-7]. Also, even in the absence of viability in the related myocardium, the reopened vessel could be a source of collaterals to other vessels (eventually future compromised).
There are some previous published studies that reported good results in the evolution of patients submitted to the recanalization of the coronary vessel in the sub-acute phase post an AMI. The Swiss Interventional Study on Silent Ischemia Type II (SWISSI II) randomized controlled trial, conducted at 3 public hospitals in Switzerland, followed 201 patients with a recent MI, who presented with silent myocardial ischemia verified by stress imaging, and one or two-vessel coronary artery disease and who were submitted to percutaneous coronary intervention aimed at full revascularization (n=96) or intensive anti-ischemic drug therapy (n=105). During a mean (SD) follow-up of 10.2 (2.6) years, patients in the PCI group had lower rates of ischemia (11.6% vs. 28.9% then patients in the drug therapy group; P=0.03), despite the use of fewer drugs. Left ventricular ejection fraction remained preserved in PCI patients (mean [SD] of 53.9% [9.9%] at baseline to 55.6% [8.1%] at final follow-up) and decreased significantly (P < 0.001) in drug therapy patients (mean [SD] of 59.7% [11.8%] at baseline to 48.8% [7.9%] at final followup) [8].
The BRAVE (Beyond 12 Hours Reperfusion Alternative Evaluation Trial)-2 study has demonstrated that residual viability is very frequent in asymptomatic patients with sub-acute myocardial infarction, and more importantly, that PCI may be effective in salvaging viable myocardium8. In this study, 365 asymptomatic patients with acute myocardial infarction presenting between 12 and 48 h from the symptom onset were randomized to an invasive (PCI) or a conservative treatment strategy. The primary end point of the study was infarct size as assessed by sestamibi scintigraphy performed between 5 and 10 days after randomization. The median time from symptom onset to hospital admission was 22 h. In the invasive group, 98.6% of patients had mechanical revascularization. The final infarct size was smaller in the invasive group as compared with the conservative group (median 8% vs 13%, p < 0.001). The scintigraphy sub-study that included 261 patients who had paired studies (before randomization and 5 to 10 days after randomization) showed that the final smaller infarct size in the invasive strategy group as compared with the conservative strategy group was due to increased myocardial salvage in the former [9].
However, there are some other studies that showed that recanalization had no advantage over drug therapy regarding myocardial viability, improvement in ejection fraction, in systolic and diastolic debits of the left ventricle artery, in myocardial re-modelling, or in patients survival, even in cases where angioplasty is successful in obtaining adequate coronary flow [10,11]. This way, there are a lot of medical doctors that still do not recommend the attempt to reopen the sub-acute coronary artery.
The arguments of those who criticize the attempt to try to reopen the recently occluded coronary arteries in stable patients are basically related to the fears of acute and chronic complications related to this procedure. The risk of occurrence of no-reflow and re-infarction is present in these patients since the recently formed clot could easily migrate distally and lead to complications related to the migration of thrombi to coronary microcirculation that may jeopardize the collateral flow. The altered integrity of the downstream non-reperfused infarct zone may also be vulnerable to reperfusion injury [12].
There is also risk of other acute complications such as coronary dissection, extension of the occlusion in to proximal portion of the vessel, loss of coronary branches and coronary perforation associated or not to pericardial effusion and even cardiac tamponade [13-15]. We cannot forget to list other complications commonly related to interventional procedures such as worsening renal function and those related to vascular access [13-15].
Besides all the possible acute cardiac and peripheral complications related to the procedure, we have to remember that patients with occluded vessels had already presented an acute injury related to vessel occlusion during the index AMI. Despite the risk of future chronic myocardial ischemia, the risk of further acute events is much lower if the artery remains closed and protected by good collaterals (which actually tend to increase over time). Recanalization with the use of coronary stents is related to episodes of stent thrombosis and thus, higher chances of future coronary acute events. In addition, the use of conventional stents (mainly used in patients from the Public Health System in our country) is related to higher rates of future coronary restenosis and possible needs of re-interventions [13-15].
There are several data in previous literature that support this fear of part of the medical community that are still afraid of indicating the attempt to re-canalize a sub-acute occluded coronary vessel. The most used trial to support this view is The Occluded Artery Trial (OAT).
Undertaken in 83 US and 134 non-US sites, the OAT Trial showed no reduction in death, myocardial infarction (MI), or class IV heart failure when stable patients with persistent infarct artery occlusion underwent routine coronary recanalization using percutaneous coronary intervention (PCI) with stenting compared with optimal medical therapy alone. Patients were followed over a 2.9 years mean follow-up period. Actually, there was an adverse trend in the PCI group in the secondary endpoint of nonfatal re-infarctions (p=0.08) [1]. Angina was reduced (in the PCI group) through 3 years in the main trial. Both angina and dyspnoea were reduced in the PCI group over 24 months with no difference in physical functioning beyond 4 months of follow up [2]. In addition, treatment with medical therapy was less expensive than PCI in OAT [2].
There is also some scientific controversy about the apparent attenuation of remodelling associated with performing PCI in stable patients several hours post PCI. It should be noted that there was no difference by treatment assignment in one-year change in Ejection Fraction (EF), among 389 patients who had serial measurements of Left Ventricle (LV) function within the nuclear viability and angiographic ancillary studies to OAT [2,16]. The viability study confirmed that most OAT patients (70%) had at least moderately retained viability in the infarct zone and that PCI did not affect EF or volume changes compared to medications even among patients with viability [16].
Some authors suggest that the use of conventional stents (mainly used in the OAT study) could possibly explain excess in re-infarctions and an absence of PCI benefits in the trial. But, another study, that made additional follow up and accrual of 194 additional events in the OAT cohort, also provided evidence that there was no long term benefit to a strategy of routine PCI of the totally occluded IRA, even with the use of drug-eluting stents. There was no difference in the primary outcome in these patients based on the type of stent implanted. Rates of nonfatal re-infarction and death were also similar between groups based on type of stent used. However, a potentially important association between DES use and freedom from angina and revascularization relative to BMS and medical therapy was suggested [17,18].
The unexpected evolution of patients treated with PCI in the OAT study led some questioning about the impact if better rates of success in the procedures could be accomplished in that trial. But, a report described in detail the high rates of PCI success and low rates of PCI complications observed in the PCI arm of the OAT. Analysis of long-term outcomes comparing cohorts with PCI success versus failure and cohorts with PCI success versus medical treatment did not suggest that higher rates of PCI success or protocol compliance would have altered the findings of the primary intention-to-treat analysis [15].
In this presented case, we opted for percutaneous intervention due to the presumption of a large area of myocardial viability due to the good contractility in the infarcted related area. Despite the immediate success of the procedure, the visualization of the large thrombus distally migrating through the coronary artery (and the impressive worsening of the patient’s condition after this) is a good example of the fear that exists about the worsening of clinical and angiographic due to the recanalization of the vessel. We choose to perform the attempt to reopen the vessel only 5 days after the diagnostic procedure to try to diminish the amount of intra-coronary thrombus (by giving Aspirin, Clopidogrel and Enoxaparin), and also adequately promote prophylaxis of contrast-induced kidney impairment. The use of techniques that decrease the risk of embolization should be considered in all cases.
Conclusion
We can conclude that, based on the evidence currently available, there is yet no good scientific significant evidence to support the benefit from mechanical reopening sub-acute occluded coronary vessels in the absence of viable myocardium. But, in the presence of viable myocardium, a PCI with a technically good result that restores an adequate flow at the myocardial level could promote a better recovery of the injured myocardial. This way, PCI should be driven by the assessment of a correct risk/benefit ratio and not simply by the desire to re-establish the coronary flow. The goal of the procedure should be effective reperfusion at the myocardial level. Otherwise, the procedure could become detrimental to the patient and prove that, in some cases, an occluded artery is better than an open one.
References
- Hochman JS, Lamas GA, Buller CE, et al. Coronary intervention for persistent occlusion after myocardial infarction. N. Engl. J. Med. 355, 2395–2407 (2006).
- Udelson JE, Pearte CA, Kimmelstiel CD, et al. The occluded artery trial (OAT) viability ancillary study (OAT-NUC): influence of infarct zone viability on left ventricular remodeling after percutaneous coronary intervention versus optimal medical therapy alone. Am. Heart. J. 161, 611–621 (2011).
- Levine G, Bates E, Blankenship J, et al. 2015 ACC/AHA/SCAI Focused Update on Primary Percutaneous Coronary Intervention for Patients With ST-Elevation Myocardial Infarction? An Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention and the 2013 ACCF/AHA Guideline for the Management of ST-Elevadion Myocardial Infarction. Circulation. 134, 21 (2016).
- Braunwald E. Myocardial reperfusion, limitation of infarct size, reduction of left ventricular dysfunction, and improved survival. Should the paradigm be expanded? Circulation. 79, 441–444 (1989).
- Kim CB, Braunwald E. Potential benefits of late reperfusion of infracted myocardium: the open artery hypothesis. Circulation. 88, 2426 –2436 (1993).
- Abbate A, Biondi-Zoccai GG, Baldi A, Trani C, Biasucci L, Vetrovec G. The ‘open-artery hypothesis’: new clinical and pathophysiologic insights. Cardiology. 100, 196–206 (2003).
- Erne P, Schoenenberger AW, Burckhardt D, et al. Effects of percutaneous coronary interventions in silent ischemia after myocardial infarction: the SWISSI II randomized controlled trial. JAMA. 297(18), 1985-1991 (2007).
- Schömig A, Mehilli J, Antoniucci D. Mechanical reperfusion in patients with acute myocardial infarction presenting more than 12 hours from symptom onset. JAMA. 293, 2865-2872 (2005).
- Parodi G, Ndrepepa G, Conti A. Ability of mechanical reperfusion to salvage myocardium in patients with acute myocardial infarction presenting beyond 12 hours after onset of symptoms. Am. Heart. J. 152, 1133-1139 (2006).
- Wijns W, Kolh P, Danchin N, et al. Guidelines on myocardial revascularization. Eur. Heart. J. 31, 2501-2555 (2010).
- Hannan EL, Zhong Y, Jacobs AK, et al. Patients with Chronic Total Occlusions Undergoing Percutaneous Coronary Interventions. Circ. Cardiovasc. Interv. 9(5), e003586 (2016).
- Asanuma T, Tanabe K, Ochiai K, et al. Relationship between progressive microvascular damage and intramyocardial hemorrhage in patients with reperfused anterior myocardial infarction: myocardial contrast echocardiographic study. Circulation. 96, 448–453 (1997).
- Patel VG, Brayton KM, Tamayo A, et al. Angiographic success and procedural complications in patients undergoing percutaneous coronary chronic total occlusion interventions: a weighted meta-analysis of 18,061 patients from 65 studies. JACC. Cardiovasc. Interv. 6(2), 128-136 (2013).
- Buller CE, Dzavik V, Carere RG, et al. Primary stenting versus balloon angioplasty in occluded coronary arteries: the Total Occlusion Study of Canada (TOSCA). Circulation. 100, 236–242 (1999).
- Buller GC, Rankin JM, Carere RG, et al. Percutaneous coronary intervention in the Occluded Artery Trial: Procedural success, hazard, and outcomes over 5 years. Am. Heart. J. 158(3), 408 (2009).
- Dzavik V, Buller CE, Lamas GA, et al. TOSCA-2 Investigators. Randomized trial of percutaneous coronary intervention for subacute infarct-related coronary artery occlusion to achieve long-term patency and improve ventricular function: the Total Occlusion Study of Canada (TOSCA)-2 trial. Circulation. 114, 2449–2457 (2006).
- Freixa, X, Dzavik V, Forman S, et al. Long-term outcomes after a strategy of percutaneous coronary intervention of the infarct-related artery with drug-eluting stents or bare metal stents vs medical therapy alone in the Occluded Artery Trial (OAT). Am. Heart. J. 163(6), 1011–1018 (2012).
- Antoniucci D. Is an Occluded Artery Better Than an Open One? J. Am. Coll. Cardiol. Intv. 1(5), 521-523 (2008).