Research Article - Clinical Practice (2016) Volume 13, Issue 3
A longitudinal study on the distribution of the severe infectious diseases in south Sudan: malaria and tuberculosis
- Corresponding Author:
- Christo Jada
Southeast University Nanjing
Jiangsu China
E-mail: monchris5@gmail.com
Abstract
Infectious diseases are disorders caused by organisms, such as bacteria, viruses, fungi or parasites. They’re normally harmless or even helpful, but some organisms under certain conditions may cause disease. Infectious diseases can be passed from person to person; some however, are transmitted through the bites from insects or animals. Tuberculosis and Malaria are considered and still the Major causes of morbidity and mortality globally and in South Sudan in particular. South Sudan is plagued by similar problems in the pubic provision of health, and relies heavily on NGOs for diseases intervention execution and the private sector for the provision of disease control commodities. Tuberculosis commonly affects people with low immunity like elderly, those with HIV/AIDs, the young and not immunized children and those who are malnourished, on the other hand malaria commonly threat children and pregnant woman seriously specially in many tropical and subtropical areas. Like in most developing countries, infectious diseases are the most public health issues. The prospects for successful project on malaria and tuberculosis control and prevention are huge in south Sudan. Nevertheless, strengthening and coordination, infrastructure and human resources and capacity building, monitoring and evaluation are required for the successful of project of control and prevention.
Keywords
Tuberculosis, malaria, health services, HIV, malaria parasite
Introduction
Background of the study
South Sudan is the youngest Nation in Africa, having seceded from the main Sudan in 2011.
Notwithstanding, the health facilities run by the two players are not evenly distributed across the country. This state of affairs best describes the poor accessibility to infectious diseases such as malaria and tuberculosis health services in south Sudan [1].
All the states are equally affected, including Juba city which is the capital of south Sudan. Juba has three health facilities, including Juba teaching Hospital, Kator Primary care Centre (PHCC), and Muniki (PHCC) provide services.
The three facilities continue to register high epidemiological trends of malaria and tuberculosis. The health system in south Sudan has three basic levels of services delivery with the fourth being the administration unit, these include community primary health care (PHC) units which provide first aid and immunization services, plus simple medication [2,4].
Second level is referred to as primary health care centers (PHCC) whish in addition to the above do provides ANC services, have admission facilities, provide maternity services and laboratory services.
The level is the county hospitals, which in addition to all the above dose operation and the main administrative centers are the county health departments which are responsible for the overall monitoring of health services within the country [2,5].
The purpose of the study
The purpose of the study is to describe the longitudinal distributions of Tuberculosis and malaria in South Sudan from 2010 to 2015, and to establish determinants of the poor adherence of prevention and treatment among the children with malaria and Tuberculosis infectious persons attending health facilities in South Sudan.
General objectives
The purpose of this study is to explore and describe the knowledge, beliefs and practices of Malaria and tuberculosis patients in order to provide helpful data for the improvement of public health education for south Sudan and in equatorial region.
Specific objectives
1. To explore and describe the longitudinal distributions of TB and Malaria in Juba county of South Sudan, regarding the causes, treatment and prevention.
2. To explore and describe the beliefs of malaria and tuberculosis patients, regarding the mode of transmission of the disease.
3. To explore and describe the lifestyle practices, of malaria and tuberculosis patients, during their period of treatment regarding alcohol consumption, smoking and nutrition.
Hypothesis
1. The incidence and mortality of malaria and tuberculosis are increasing from 2010 to 2015 in South Sudan, especially among the children.
2. Poor health condition and the civil war may be the most important reasons of this phenomenon.
3. The economic crisis is also one of the factors that threatening the health situation in South Sudan.
Literature Review
The burden of severe infectious diseases, in south Sudan
The importance of providing strong evidence based estimates of the mortality began with the global burden of disease [6]. In couples of years, malaria accounted for 7% of deaths in children age less than five years globally, and 17% of deaths in sub-Saharan Africa including south Sudan, where it was considered the leading cause of death in Africa. As a result of the large decrease in malaria mortality in children age less than five years, malaria accounted for just 5% of less than five years deaths globally in 2015 [7].
Another challenge is tuberculosis, it ranks 22nd in the world high burden. The available data on tuberculosis control in the community show the ever increasing cases of tuberculosis disease alongside the steep gradient of patient defaulter trends. There is enough proof that taking anti tuberculosis medications irregularly or worst of all abandoning (non-adherence) is the biggest challenge of tuberculosis control risking multi drug resistant tuberculosis [3].
The control of the severe infectious disease
The malaria control situation is threatened by the impact of internally displaced populations, and natural disasters, civil war, that put added strain on an already weakened system from years of conflict and that may destabilize whatever gains that have been made.
To reduce the malaria burden, the (WHO) recommended case management and vector control, tools have been implemented expansively in south Sudan, which can be able to assess program implementation and progress towards attainment of (MDGs), measuring the impact of malaria control on reducing disease morbidity and mortality is essential [8].
On the other hand tuberculosis control in south Sudan is a mandate of the national tuberculosis program (NTP) established in 2006.
However, the health infrastructure is still poor and services are inequitable distributed.
The national tuberculosis program indicators are poor, for example the defaulter rate is at 14% case finding rate stand, compare to 70% target, while the treatment success rate stands at 72% as opposed to 85% recommended by (WHO) standard [9].
Transmission of tuberculosis and malaria
Mycobacterium Tuberculosis is carried in airborne particles, called droplet nuclei. Infections droplet nuclei are generated when persons who have pulmonary or laryngeal tuberculosis disease cough, sneeze, shout or sing, than Tuberculosis can be transmitted.
The risk of infection dependent on several factors such as the immune status of recipients, transmission occur when a person inhale droplet nuclei containing tuberculosis [9]. And the malaria transmission occurred throughout the year in the swampy lowlands. In all areas incidence of malaria increases during rainy season or flooding as well as in association with movement of populations with little immunity to endemic areas when outbreaks occur or the disease reaches epidemic proportion [10].
And it is transmitted by an infected female anopheles mosquito, and occasionally or rarely through blood transfusion. The anopheles from Gambiae family is the major vector system in Africa region [11]. The appearance of drugresistant strains are considered to be the primary factors that contributed to the resurgence of malaria, plus the spread of insecticide resistant of mosquito and lack of malaria vaccines [12].
Prevention of tuberculosis and malaria
Every country might have its own projects for preventing the re-emerging incidences and prevalence [13]. The best and the effective management of malaria in children less than five years require early diagnosis and prompt action [14]. There is possibility of developing of using molecular genetics to manipulate the genomes of insects, larva and vectors such that they are no longer capable of acting as a vector. The aim of this developing molecular is to replace natural vector populations of mosquitos with populations which are unable to support complete development of the malaria parasite [15].
For the prevention of tuberculosis they prefer the early diagnosis too as for malaria as the best way to protect children from getting infected. BCG immunization of babies soon after birth up to two years of age will protect them against development of tuberculosis meningitis. Globally the cure rate in such cases is about 50%.
The prevalence and death rates due to tuberculosis should be halved by 2015 compared to the rates in 1990, the world Health Organization recommends that 70% of smear positive cases should be detected and treated, while at least 855 of the positive cases should be successfully treated [16].
Socio-economic conditions
TB has been associated with factors linked to socioeconomic deprivation: poverty, overcrowding and malnutrition. The magnitude of TB is high among the poor, displace and homeless, drug addicts, elderly, malnourished and women. The association between TB and poverty was shown by the decline in TB burden with the improved living condition in developed countries prior to the introduction of treatment. Improved living condition was also found to reduce the risk of infection from 4-6% per annum. In contrast, the resurgence of TB in developing countries as the living condition worsens shows its association with poor living conditions. TB was also found to disproportion affect the poor. Therefore, free diagnosis and treatment was offered to TB p (mainly to smearpositive PTB cases) to reduce the economic burden for seeking diagnosis and treatment and treat the highly infectious cases. However, limited access to the service because of the poor socioeconomic condition of the patients and households has reduced the utilization of the available service. Thus, interventions that improve access to health service need serious consideration [17].
In South Sudan, the plummeting value of the South Sudanese pound against the dollar has left small traders unable to stock shelves with imported goods, on which the country relies heavily.
Food insecurity is also on the rise, with half of South Sudan’s 9.7 million people facing food shortages – more than double the number last year [18].
Tuberculosis and HIV co-infection
A complex interaction exists between TB and HIV infection. HIV increases the risk of infection, as it reactivates LTBI and increases the progression to active disease. TB-HIV co-infection has fatal consequences as TB becomes the leading cause of death in HIV infected individuals and patients with acquired immunodeficiency syndrome (AIDS). HIV lowers the host’s immune response to MTB. The lifetime risk of developing active TB in HIV infected individuals is 10% per year compared with lifetime risk of 5-10% in individuals without HIV. As a result, the TB case notification rate (CNR) has increased four to six fold in sub-Saharan Africa.
HIV affected the performance of TB control programmes by increasing the number of TB cases and by compromising the treatment outcomes. It created a huge challenge to the already overstretched and under staffed health system in high burden countries. It reduced the proportion of smear-positive cases; and increased the rate of treatment failure, defaulter and death, which in turn compromised the progress towards achieving the targets recommended for TB control under DOTS strategy [17].
Co-infection with tuberculosis (TB)/HIV has not precisely been documented. TB/HIV co-infection rate of 12% among new smear positive cases and 10.8% among all forms of TB. In 2010, the co-infection rate was 9.7% among new smear positive cases and 11.4% among all forms of TB [18].
Methodology
Study area
This study will be conducted in Juba County which is comprised of seven administrative centers known as payams with a population of about 300,000 people.
Juba municipality is the major administrative center of the county. The study will focus on only three payams namely Juba town, Kator Primary Health Care Centers and Munuki Primary Health Care Centers and include Juba Teaching Hospital since they are the only ones with TB management centers including malaria. Among them, Juba Teaching Hospital has the majority of the qualified medical staff and for that matter attracts most patients.
Source of data
Data for this study will be extracted from the malaria and tuberculosis patients who recently got their treatment, and the service providers working in Kator Primary Health Care Centers, Munuki Primary Health Care Centers and Juba Teaching Hospital, that provide Malaria and Tuberculosis in Juba county. And from the Ministry of Health database.
Research design
The study will adopt a cross-sectional study design, employing both quantitative and qualitative techniques of data collection. A crosssectional study design is chosen in consideration of the limited time required to accomplish the project. The study will involve consulting the tuberculosis registers and malaria surveillance department at the various health facilities in order to identify TB and malaria patients to participate in study.
Data processing and analysis
Quantitative data will be checked for completeness and accuracy prior to coding and editing during the data entry process. This will ensure data viability and validity pertaining to the information provided.
Quantitative data generated from the study will be cleaned, validated for completeness before entering into the computer for final analysis. Data analysis will be done using SPSS and Origin soft-ware packages or EXCEL. Thereafter, the data will be summarized in form of tables, graphs, figures, frequencies and percentages. Statistical tests of significance will be subjected to the analyzed data to come up with valid deductions.
Results and Discussion
Plan for dissemination
The findings of this study will be shared with Malaria surveillance, the Ministry of Health, the NTP, the State Ministry of Health Central Equitoria State and the Juba County Health Department, and other stakeholders like WHO, UNDP, USAID, Global Fund, MSF in South Sudan.
Results of TB
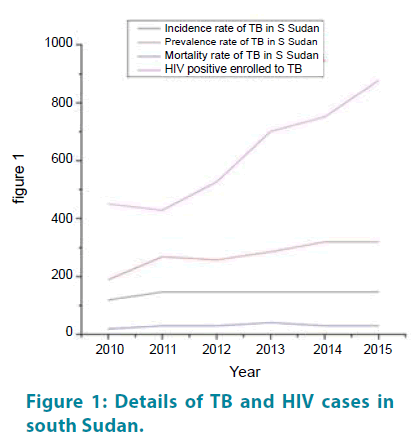
Increased incidence rate of TB in South Sudan was found form 2010 to 2015, but the mortality of tuberculosis was table for the whole period. While the proportion of HIV positive enrolled with TB was very high and continue increasing from 40% to 80% (TABLE 1).
| Year | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
| TB Incidence | 119 | 146 | 146 | 146 | 146 | 146 |
| TB Prevalence | 188 | 268 | 257 | 286 | 319 | 319 |
| TB Mortality | 19 | 30 | 30 | 40 | 29 | 29 |
| NEW Cases of Tb | 6,000 | 7,053 | 8,155 | 7,054 | 8,076 | 9,381 |
| Relapse | 154 | 165 | 181 | 186 | 259 | 276 |
| CNR/100,000 | 59 | 68 | 76 | 64 | 71 | 80 |
| CDR (%) | 50 | 46 | 52 | 44 | 59 | 55 |
| Enrolled | 6,430 | 7,595 | 8,862 | 7,799 | 8,856 | 10,250 |
| HIV Tested | 3,628 | 3,542 | 4,583 | 4,791 | 5,892 | 7,598 |
| HIV Positive | 450 | 428 | 527 | 701 | 752 | 878 |
Table 1: TB and HIV results in south Sudan.
The incidence rate of TB was stable for the whole five years. In 2010 it was Sudan not south Sudan. We included that year (2010) to see if the trend was raised after the separation of South Sudan from Sudan (FIGURE 1).
The prevalence of TB was low and was increased a bit in 2011 and continuous at one level from 2011 to 2015, as well as HIV enrolled to TB in 2011 was a bit higher, then in 2011 dropped in 5% and starting increasing till 2015.
HIV positive enrolled TB make a different shape in the trend by increased dramatically since 2011 till 2015, and it was higher in term of percentage compared to other trends, and it can estimated more than 80%.
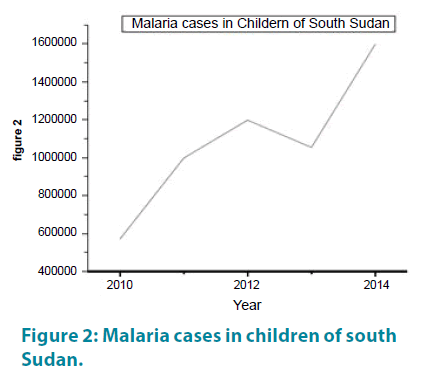
Malaria results
Another issue is Malaria as public health problem in South Sudan especially among the children. In our study we found that the cases from the trend increases from the year 2012 to the month of May 2015, but the cases continue increases every year from the Months early April and declining in late October, in a year 2012 it declined from October to the normal and in 2013 raises from May as usual and continue up to September and start declining, and in 2014 raises from May to August and then declining, and in 2015 up to May increases as in the previous years, especially during rainy season (FIGURE 2).
Figure 2: Malaria cases in children of south Sudan.
Discussion
In the recent decades, the number of Malaria and TB cases has increased by several folds especially in South Sudan.
As showed in trend, incidence and mortality were bit lower and stable, this shows the treatment concerns and follow up for TB patients.
HIV infection is considered the main risk factor for the increase in the number TB patients. The information about the rate of HIV infection among different groups of a community is important to understand the extent of the problem and to implement appropriate prevention and control measures.
In a trend of TB patients in South Sudan, more than a fifth of them were HIV infected enrolled to Tuberculosis patients.
Higher TB-HIV co-infection rates, as high as 60% was reported from South Sudan.
These studies however were comparison and were conducted in few major payams in Juba city where the prevalence of HIV infection in the general population was much higher.
In our study, there was no difference in the rate of Malaria infection among TB patients by gender.
As expected, the prevalence of HIV among the population was higher in urban areas than rural areas; this could be due to the difference in the risk and rate of HIV infection in urban and rural communities.
In our study, the rate of HIV infection in TB patients strongly correlated with the rate of HIV infection among the population. This was because HIV is the main risk factor fuelling TB epidemic and that is the reason of a higher trend of TB enrolled with HIV. Similarly, countries with high HIV prevalence in the general population had higher incidence of TB and relatively higher rates of TB-HIV co-infection.
Our study has shown an increase in TB notification trend rate of 60% increase in HIV prevalence in South Sudan with high prevalence of HIV infection. In a generalized, the rate of HIV infection among TB patients is an indicator of the maturity of the HIV epidemic and predicts the occurrence of new TB cases at country level. As hypothesized poor health condition, bed net use was associated with a significant reduction in the probability of testing positive for malaria.
Malaria on other hand also shows a high public health issue especially among the Children in South Sudan. The predicted probability of a child testing positive for malaria jumped from 40 percent for an urban resident to 85 percent for a rural resident, although age was significantly positively associated with malaria infection, these findings are consistent with previous studies that found that the risk of malaria infection in young children increases with age according to Bejon et al., and the author agrees with him because if you realize from author’s data that the most affected children are under five years old, but the above five years are better than under five years.
Nutrition status was strongly associated with malaria infection, as hypothesized as beliefs. Children that tested positive for anemia were predicted to have a significantly higher risk of malaria infection.
As expected, there was a significant difference among children living in poor, not poor, rural and urban households.
The location of the child’s residence was also found to be a significant predictor of infection. Children living in rural regions had higher chances of testing positive for malaria.
The all two trends decline in 2012 and suddenly raised in 2013, the reason is that: in that year the country had witnessed war followed by the financial crisis, and this situation usually companied by insecurity, and a lot of patients might have quit their follow up looking for their better living conditions and secure places to live.
Ethical issues
An ethical clearance will be obtained from government authorities and consent will be obtained from each respondent prior to being enrolled in the study. Only those who will consent to participate will be enrolled for the study while those who will refuse to consent will be excluded. Maximum confidentiality will be ensured to be people’s views.
Limitations of the study
The escalating civil war in South Sudan may render our movements into the communities/ villages rather impossible.
Some malaria patients will not able to reach to the nearest Primary Health Care, due to distance problem and for Tuberculosis patients it may be unable to trace them since many of them could have crossed the borders for security reasons.
The targeted sampling population may not be met due to the unforeseen circumstance.
References
- Anderson RM, May RM, Anderson B. Infectious diseases of humans: dynamics and control. Oxford: Oxford University press. (28) (1992).
- Huerga H, Spillane H, Guerrero W, Odongo A, Varaine F. Impact of introducing human immunodeficiency virus testing, treatment and care in a tuberculosis clinic in rural Kenya. Int. J. Tuberc. Lung Dis. 14(5),611-615 (2010).
- Pasquale H, Jarvese M, Julla A et al. Malaria control in South Sudan, 2006–2013: strategies, progress and challenges. Malar. J. 12(1),1 (2013).
- National TB Program NTP Report. South Sudan (2012) TB CARE I Annual Report Year
- NTP Reports for 2012/2013 Juba Teaching Hospital, Kator PHCC and Munuki PHCC monthly Report.
- Snow RW, Craig MH, Newton CRJC, Steketee RW. The public health burden of Plasmodium falciparum malaria in Africa. Working Paper11. Disease Control Priorities Project, Bethesda, Maryland, USA: Fogarty International Center, National Institutes of Health. (2003).
- World Health Organization. Malaria rapid diagnostic test performance: results of WHO product testing of malaria RDTs: round 6 (2014-2015). (2015).
- Pasquale H, Jarvese, M, Julla A et al. Malaria control in South Sudan, 2006–2013: strategies, progress and challenges. Malar. J. 12(1), 374 (2013).
- Cometto G, Fritsche G, Sondorp E. Health sector recovery in early post‐ conflict environments: experience from southern Sudan. Disasters. 34(4),885-909 (2010).
- Schmidt BM. Tuberculosis interventions to prevent transmission of infection in health care workers: a systematic review (Doctoral dissertation, University of Cape Town). (2015).
- World Health Organization. Guidelines on prevention of the reintroduction of malaria (No. 34). World Health Organization. (2007).
- Breman JG, Mills A, Snow RW et al. Conquering malaria (2006).
- Saleh AMA, Adam SM, Ibrahim AMA, Morsy TA. Malaria: A General Minireview With Reference To Egypt. J. Egypt Soc. Parasitol. 46(1),35-48 (2016).
- Kassile T. Prevention and management of malaria in under-five children in Tanzania: a review. Tanzan. J. Health Res. 14(3) (2012).
- Phillips RS. Current status of malaria and potential for control. Clin. Microbiol. Rev. 14(1),208-226 (2001).
- Narasimhan P, Wood J, MacIntyre CR, Mathai D. Risk factors for tuberculosis. Pulm. Med. (2013).
- Mai NJH, Mayai AT, Tiitmamer N Sporadic Fuel Crisis in South Sudan: Causes, Impacts and Solutions1 (2016).
- El Sony AI, Baraka O, Enarson DA, Bjune G Tuberculosis control in Sudan against seemingly insurmountable odds. Int. J. Tuberc. Lung Dis. 4(7),657-664 (2000).