Case Report - Interventional Cardiology (2011) Volume 3, Issue 4
64-slice computed tomography as an adjunct to aortography in suspected iatrogenic aortocoronary dissection
- Corresponding Author:
- Stephen Dorman
Morriston Cardiac Centre, Swansea, SA3 5EA, UK
Tel: + 44 1792 702 222
Fax: 416-603-6919
E-mail: stephen.dorman@wales.nhs.uk
Abstract
Keywords
aortocoronary dissection,coronary dissection,iatrogenic aortic dissection,percuataneous coronary intervention
Clinical case
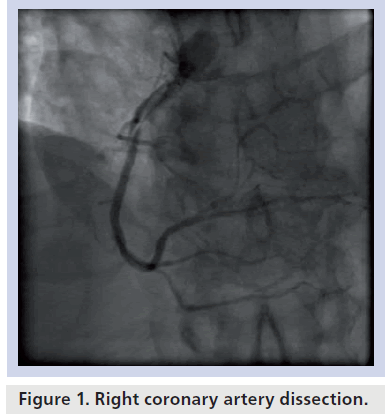
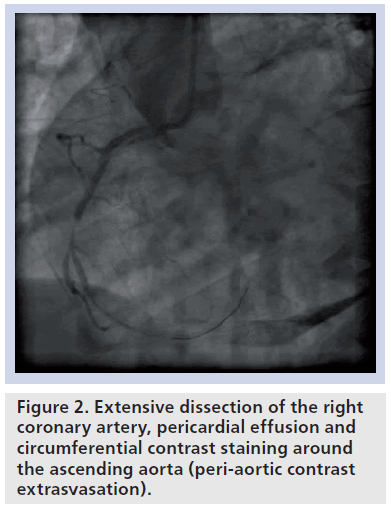
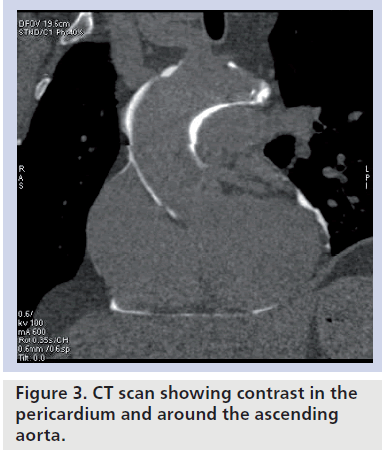
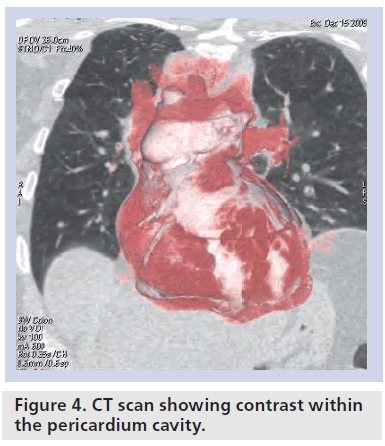
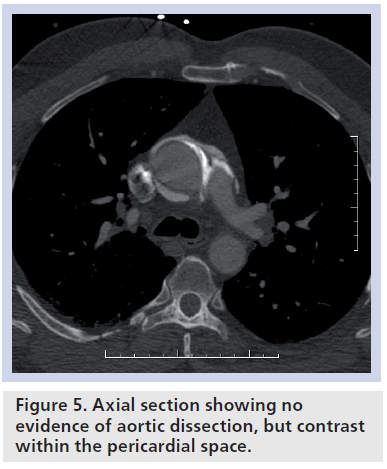
A 53‑year-old male ex-smoker with hypercholesterolemia presented with crescendo angina associated with a troponin I release of 0.21 g/l and right bundle branch block on his resting electrocardiogram. He was treated medically for an acute coronary syndrome with aspirin, clopidogrel and fondaparinux. Transthoracic echocardiogram showed preserved systolic function with no evidence of regional wall motion abnormality. Diagnostic coronary angiography was performed as an in-patient via the right radial artery using standard 5-french judkins catheters (Cordis Corp., FL, USA), 50 IU/kg heparin bolus and an automated injection system (ACIST Medical Systems, Inc., MN, USA). Coronary angiography showed single vessel disease with a thrombotic proximal right coronary artery (RCA) occlusion. Using a 6-french judkins right guide catheter and an intermediate guidewire, the occlusion was crossed, ReoPro® (abciximab; Eli Lilly and Company, IN, USA) was administered and a 3 × 18 mm Multi-link Vision™ (Abbott Vascular, IL, USA) bare-metal stent deployed at 10 atmospheres immediately restoring Thrombolysis In Myocardial Infarcation (TIMI)3 flow. Routine control angiography was performed after guidewire removal and showed evolution of an extensive coronary dissection proximal and distal to the stent mid-injection (Figure 1). The extravasation of contrast into the pericardium and circumferentially around the aortic root and ascending aorta suggested coronary dissection complicated by perforation associated with Dunning type III [1] retrograde aortic dissection (Figure 2). The patient remained hemodynamically stable, ReoPro was discontinued, the dissection recrossed into the true lumen and the proximal coronary dissection immediately stented with a further 3.5 × 28 mm Vision bare-metal stent back to the RCA ostium. The distal coronary dissection was then sealed with a 3 × 18 mm Vision bare-metal stent restoring TIMI3 flow to the distal vessel. Transthoracic echocardiography was performed in the catheter laboratory and showed a small pericardial effusion. The patient remained stable and underwent emergent 64-slice ECG gated computed tomography (CT). Somewhat suprisingly this did not demonstrate evidence of classical aortic dissection, but in fact showed extravasation of contrast into the pericardial space and within the region of the ascending aorta consistent with the anatomy of the pericardial recesses (Figures 3–5). In view of the reassuring imaging and the fact that he remained stable he was managed conservatively, discharged 7 days later and remained well at 1‑year follow-up.
Figure 1: Right coronary artery dissection.
Discussion
In this case, contrast staining around the aorta in the context of iatrogenic antegrade and retrograde RCA dissection justifiably suggested an extensive aortic dissection involving the ascending aorta. Immediate percutaneous coronary intervention to seal the presumed entry site and distal dissection was successful in restoring TIMI3 flow to the affected artery and the patient’s stable hemodynamic condition permitted further diagnostic evaluation with 64-slice CT. This adjunctive imaging was highly instructive in excluding classical dissection and confirming coronary rupture, with associated pericardial extravasation supporting a conservative management strategy, validated by the patient’s excellent outcome. As forceful injections are known to exacerbate retrograde aortic dissections, the ACIST CVi® system was reviewed by ACIST Medical Systems, Inc. who found no evidence of device malfunction and quoted a coronary dissection rate of 2 per million with their system based on their last 4 years data.
▪ Iatrogenic aortic dissection
Iatrogenic aortic dissection (IAD) is a rare and highly feared complication of coronary angiography and PCI with reported incidences of 0.02–0.15% [1,2] and mortality rates of up to 32%, similair to that of spontaneous type A aortic dissection [3]. By contrast, coronary artery dissection is a relatively frequent complication of percutaneous intervention, detected in 20–30% of cases angiographically [4] but far more so with intravascular ulatrasound or optical coherence tomography. These limited dissections are not usually clinically significant but in less than 1% of cases acute vessel closure can occur and in 0.3–0.6% of cases, coronary perforation [5,6]. Whilst retrograde extension to the aorta is particularly dramatic, antegrade coronary artery dissection can of course be equally life threatening, depending on the extent of the ischemic territory involved.
▪Pathophysiology of aortocoronary dissection
The exact pathophysiology of IAD remains obscure but an entry point often originates within the coronary dissection and then blood flow or forceful injection of contrast leads to progressive retrograde extension of the subintimal space tracking back to the aortic root. As the supravalvular ridge is rich in collagenous fibers, dissections usually remain below the sinotubular junction of the aorta. Approximately half of iatrogenic dissections are confined below the aortic root (Dunning type I) and generally have an excellent prognosis [7]. A number of risk factors for aortocoronary dissection have been described including hypertension, older age, connective tissue disease, extensive atherosclerosis, previous myocardial infarction, use of left amplatz-shaped guiding catheters, variant anatomy and vigorous injection of contrast media [1,8,9]. Aortocoronary dissections affect the RCA 80% of the time and are more common in acute myocardial infarction [1] and with chronic total occlusions [10].
▪ Diagnosis of aortocoronary dissection
The diagnosis of aortocoronary dissection secondary to cardiac catheterization is typically made on the basis of dense staining of the aortic wall with incomplete dye clearance following contrast media injection [11]. Clinical symptoms and signs are variable and often nonspecific as there may be concomitant coronary ischemia and in some cases tamponade from coronary dissection/perforation. Januzzi et al. reviewed the International Registry of Aortic Dissection (IRAD) and showed that IAD is more difficult to diagnose clinically than spontaneous aortic dissection owing to its atypical clinical presentation and lack of classical signs on imaging studies [3]. Modern imaging techniques such as transesophageal echo [12], CT [13] and MRI [12] have been well validated in the setting of classical spontaneous aortic dissection with reported sensitivities between 97 and 100%. Their diagnostic utility is, however, highly dependent on their ability to detect an intimal flap or separate true and false lumens. A variant of aortic dissection exists in which intimal tear is present without intimal flap or hematoma and consequently these dissections may be missed by current imaging modalities [14]. In addition, the acute setting of IAD means that adjunctive imaging is not always appropriate in unstable patients and so it is common for there to be no adjunctive imaging used for diagnostic confirmation in case series reported in the literature [11]. This last limitation applies particularly to cardiac CT, which requires a patient to be hemodynamically stable for transfer. In addition, cardiac CT necessitates use of ionizing radiation as well as iodinated contrast media, which can be problematic immediately following cardiac catheterization. For this reason, transesophageal echo has potential advantages in the unstable patient who cannot be safely transferred from the catheterization laboratory.
Our case nicely illustrates the potential pitfalls of relying solely on aortography to make the diagnosis of aortic dissection. With the advent of 64-detector row CT, the increased spatial and temporal resolution has greatly increased the ability of CT to confirm or exclude the diagnosis of aortic dissection in hemodynamically stable patients. There are, however, well-documented pitfalls in the interpretation of the cardiac and pericardial structures [15]. Motion artifact simulating an intimal flap in the ascending aorta still occurs with non-ECG gated 64-detector CT [16] and in particular the normal anatomy of the pericardial recesses needs to be appreciated as these can equally mimic the appearances of aortic dissection and intramural hematoma [17]. Our case also nicely illustrates the diagnostic utility of 64-slice cardiac CT in excluding the diagnosis of IAD and further refining the final diagnosis of coronary dissection/rupture with pericardial extravasation.
▪ Management
In view of the limited case series in the literature, no consensus exists on the optimum management of IAD. Nevertheless, it appears that if the entry point of the dissection within the coronary artery is immediately sealed with aorto-ostial stenting and the dissection is confined to the aortic root then the prognosis with conservative management is excellent [1]. The management of dissection extending into the ascending aorta is more controversial, with some authors advocating an immediate aorto-ostial stenting policy with surgery reserved as a ‘bail out’ [7], whilst others have questioned the safety of postponing surgery [10]. Aortic and coronary surgery in patients on full antiplatelet therapy with active ischemia is clearly not without risk but equally it is not always possible to achieve satisfactory percutaneous results in the context of extensive anterograde and retrograde dissection. What our case illustrates is the potential to use adjunctive imaging when an early stenting strategy has stabilized the situation to further assess the risk/benefits of surgical intervention.
Future perspective
With the expansion of percutaneous valve programs and an increasingly complex coronary caseload, it seems inevitable that IAD will remain a rare but significant complication of percutaneous intervention. Aortography has always been the yardstick by which the initial diagnosis of IAD is suspected but the sub-millimeter resolution of cardiac CT, potentially complemented by invasive imaging with intravascular ultrasound, provides the opportunity to refine our understanding of this complex heterogeneous condition. In turn, this should allow evidencebased management algorithms to evolve, which identify those patients who benefit most from early surgical intervention and those that can safely be managed conservatively.
Conclusion
IAD remains a rare but feared complication. In this case, aortography was suggestive of coronary dissection complicated by extensive type A dissection. Immediate percutaneous intervention, however, appeared to seal the entry point to the retrograde dissection and restored TIMI3 flow antegradely. Further evaluation with 64-slice CT then clarified the diagnosis suggesting coronary perforation/ rupture complicated by pericardial extravasation rather than classical IAD. The pathophysiology of IAD remains poorly understood but in the future new imaging modalities are likely to contribute significantly to our understanding of how best to manage this dangerous condition.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Executive summary
▪▪ Iatrogenic aortic dissection (IAD) is a rare but highly feared complication of cardiac catheterization with a high associated mortality.
▪▪ The existing literature on IAD is limited to small case series with a degree of publication bias, meaning that no evidence-based guidelines currently exist on optimum management.
▪▪ The exact pathophysiology of IAD remains obscure and whilst classical aortic dissection is easily recognized, conventional aortography alone may not always delineate the subtle but important differences in presentation, such as coronary rupture with circumferential periaortic extravasation.
▪▪ Immediate aorto-ostial stenting followed by stenting of the retrograde dissection can rapidly stabilize a deteriorating clinical situation.
▪▪ A detailed understanding of pericardial anatomy is important in interpreting the results of aortography and imaging studies of IAD to ensure the correct diagnosis is made.
▪▪ The sub-millimetre resolution of the latest generation of CT scanners has augmented our ability to identify and characterize the pericardium. This is of particular value when deciding on the need for surgery in stable patients with IAD.
References
- Dunning DW, Kahn JK, Hawkins ET, O’Neill WW. Iatrogenic coronary artery dissections extending into and involving the aortic root. Catheter Cardiovasc. Interv. 51(4), 387–393 (2000).
- Ruda-Vega M. Aortic dissection – exceedingly rare complication of coronary angioplasty. Cathet. Cardiovasc. Diagn. 42(4), 416 (1997).
- Januzzi JL, Sabatine MS, Eagle KA et al. Iatrogenic aortic dissection. Am. J. Cardiol. 89(5), 623–626 (2002).
- Sharma SK, Israel DH, Kamean JL, Bodian CA, Ambrose JA. Clinical, angiographic, and procedural determinants of major and minor coronary dissection during angioplasty. Am. Heart J. 126(1), 39–47 (1993).
- Gruberg L, Pinnow E, Flood R et al. Incidence, management, and outcome of coronary artery perforation during percutaneous coronary intervention. Am. J. Cardiol. 86(6), 680–682, A8 (2000).
- Ellis SG, Ajluni S, Arnold AZ et al. Increased coronary perforation in the new device era. Incidence, classification, management, and outcome. Circulation 90(6), 2725–2730 (1994).
- Carstensen S, Ward MR. Iatrogenic aortocoronary dissection: the case for immediate aortoostial stenting. Heart Lung Circ. 17(4), 325–329 (2008).
- Wilson SK, Hutchins GM. Aortic dissecting aneurysms: causative factors in 204 subjects. Arch. Pathol. Lab. Med. 106(4), 175–180(1982).
- Awadalla H, Sabet S, El Sebaie A, Rosales O, Smalling R. Catheter-induced left main dissection incidence, predisposition and therapeutic strategies experience from two sides of the hemisphere. J. Invasive Cardiol. 17(4), 233–236 (2005).
- Hunt I, Faircloth ME, Sinha P, Marber MS, Venn GE, Young CP. Aortocoronary dissection complicating angioplasty of chronically occluded right coronary arteries: is a conservative approach the right approach?J. Thorac. Cardiovasc. Surg. 131(1), 230–231(2006).
- Gómez-Moreno S, Sabaté M, Jiménez-Quevedo P et al. Iatrogenic dissection of the ascending aorta following heart catheterisation: incidence, management and outcome. EuroIntervention 2(2), 197–202 (2006).
- Nienaber CA, Spielmann RP, von Kodolitsch Y et al. Diagnosis of thoracic aortic dissection. Magnetic resonance imaging versus transesophageal echocardiography. Circulation 85(2), 434–447 (1992).
- Ribeiro C, Ribeiro N, Figueiredo A, Carvalho J, Beirão I. Computed tomography in the evaluation of acute aortic dissection. Rev. Port. Cir. Cardiotorac. Vasc. 17(2), 81–89 (2010).
- Svensson LG, Labib SB, Eisenhauer AC, Butterly JR. Intimal tear without hematoma: an important variant of aortic dissection that can elude current imaging techniques. Circulation 99(10), 1331–1336 (1999).
- Broderick LS, Brooks GN, Kuhlman JE. Anatomic pitfalls of the heart and pericardium. <em>Radiographics</em> 25(2), 441–453 (2005).
- McMahon MA, Squirrell CA. Multidetector CT of aortic dissection: a pictorial review. <em>Radiographics </em>30(2), 445–460 (2010).
- O’Leary SM, Williams PL, Williams MP et al. Imaging the pericardium: appearanceson ECG-gated 64-detector row cardiac computed tomography. Br. J. Radiol. 83(987), 194–205 (2010).