Review Article - Interventional Cardiology (2011) Volume 3, Issue 2
Update on disease: percutaneous coronary intervention of bifurcation lesions
- Corresponding Author:
- Ioannis Iakovou
Onassis Cardiac Surgery Center, 356 Syggrou Ave
Athens 17674, Greece
E-mail: ioannis.iakovou@gmail.com
Abstract
Keywords
bifurcation lesion, drug-eluting stents, percutaneous coronary intervention, stenting techniques
Coronary artery bifurcation lesions constitute a complex lesion subgroup encountered in 15–20% of all percutaneous coronary interventions (PCI) [1–5]. Compared to bare-metal stents, drug-eluting stents (DES) provide superior angiographic and clinical outcomes; thereby stenting using DES has become the default approach for the treatment of bifurcation coronary disease. Refinement of the various techniques used (high-pressure stent deployment or postdilatation, final kissing-balloon dilation (FKI), intravascular ultrasound (IVUS) guidance, among others), proper selection of lesions to be treated with a two-stent technique as intention-to-treat and deferring PCI in nonsignificant side branches (SB) with a suboptimal result after main branch (MB) stenting, have led to even better outcomes that have been demonstrated to be similar to those of nonbifurcation PCI [2,4]. Bifurcation PCI with DES are considered predictive of stent thrombosis (ST); however, thus far the reported ST rates are low and independent of the technique [1,2,4,6,7]. As a result, an increasing number of patients, with even more complex lesions, are currently being treated successfully with PCI. Contemporary randomized studies demonstrated that routine stenting in both branches offers no benefit over stenting of the MB only with provisional stenting of the SB in terms of angiographic or clinical outcomes [2,4,8]. The provisional strategy is now the preferred approach; it is performed in approximately 70% of true nonleft main bifurcation lesions [2].
Bifurcation lesion classification schemes
Coronary bifurcations by virtue of their marked anatomical variability (bifurcation angle, diameter and curvature of branches and bifurcation site) present various patterns of low wall shear stress, which act in concert with systemic cardiovascular risk factors to produce markedly heterogeneous lesions at these sites. Accordingly, there is marked diversity among bifurcation lesions in terms of plaque burden, distribution and composition. Lesion heterogeneity potentially affects procedural success, complication rate and long-term outcomes, and partially accounts for the complex nature of bifurcation PCI and the inability to satisfactorily standardize the techniques. Therefore, the most suitable PCI strategy should be selected and optimized on an individual basis, considering bifurcation characteristics that are known to influence the acute and long-term results. Several classification schemes have been described for bifurcation lesions, as a means of standardized description, to facilitate communication between clinicians and researchers when comparing different series and techniques, prediction of procedural complications or difficulties and planning the interventional approach [1,2,5,9–11]. Regarding the angle between the SB and the MB distal to the bifurcation, these lesions are classified as Y-shaped or T-shaped if this angle is <70° or >70°, respectively. Despite the inherent inability of conventional angiography to accurately determine atheroma distribution and extent of disease when compared with IVUS, six major angiographic classification systems have been described so far, and all but the latest are based exclusively on atheroma distribution at the bifurcation level. Chronologically, these are the Duke, the Sanborn, the Safian, the Lefevre, the Medina and the Movahed classifications. The first four classifications have not been adopted in clinical practice because the nomenclature that they use is not associated with the various anatomic features of the bifurcation lesions, making them difficult to remember and clinically irrelevant. In the Medina classification, three components of the bifurcation are evaluated successively for the presence of a significant stenosis (>50% diameter stenosis) in the following order: proximal MB, distal MB and SB. Each of these components is assigned the value one in the presence of such a stenosis; otherwise it is assigned the value zero. ‘True’ bifurcation lesions are defined by the presence of a >50% diameter stenosis adjacent (<5 mm) to, and/or at, the ostium of both a MB and a SB. If significant disease involves only the MB or the SB, the bifurcation lesion is defined as ‘nontrue’ or ‘false’. Thus, Medina lesions 1.1.1, 1.0.1 and 0.1.1 quote for ‘true’ bifurcation lesions. This classification, which has been recommended by the European Bifurcation Group, gives the reader an immediate mental picture of the distribution of atheroma at the bifurcation level and it is easy to remember and simple to use [8]. The European Bifurcation Group has also proposed a new classification of bifurcation lesion treatment, to permit accurate comparisons of well described techniques in homogeneous lesion groups. The classification of the techniques (Main, Across, Distal, Side [MADS]) is based on the manner in which the first stent has been implanted [11].
Provisional SB stenting versus systematic two-stent approach
There has been a debate in the past regarding the best approach to bifurcation PCI with DES, that is stenting of the MB only with provisional SB stenting versus routine stenting of both branches, which has been finally resolved following the publication of four large randomized trials.
In the NORDIC bifurcation study, 413 patients undergoing bifurcation PCI with sirolimuseluting stents were randomized to either the provisional approach or the two-stent approach with any technique [12]. No significant difference between the two groups was detected for major adverse cardiac events (MACE); 2.9% in the one-stent group and 3.4% in the two-stent group at 6 months. At 14 months, definite ST rates were low in both groups (1 and 0.5%, respectively; p = non significant [NS]) [7]. At 8 months, the provisional and the two-stent approaches yielded similar angiographic restenosis rates at the MB (4.6 and 5.1%, respectively; p = 0.84) and the SB (19.2 and 11.5%, respectively; p = 0.062). The crossover rate to SB stenting was 4.3% while 6‑month target lesion revascularization (TLR) rates were considerably low in both groups (1.9% in the one-stent group and 1% in the two-stent group; p = 0.36).
The ‘Bifurcations Bad Krozingen’ (BBK) study assessed the effect of routine T-stenting on SB restenosis as compared with provisional T-stenting in 202 patients; all were treated with sirolimus-eluting stents and 80% of the lesions were ‘true’ bifurcations [13]. Binary restenosis in the SB was 9.4 and 12.5% (p = 0.32) in the provisional and routine T-stenting group, respectively, while the corresponding TLR was 5.0 and 7.9% (p = 0.39). Definite ST has been reported as 1 and 2% (p = 1.0) in the provisional and routine T-stenting group, respectively. Crossover to SB stenting was required in 18.8% of patients.
In the Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus- Eluting Stents (CACTUS) study, 350 patients with bifurcation disease (94% of the lesions were ‘true’ bifurcations) were treated with either stenting of both branches with the crush technique or the provisional approach [14]. The rates of MACE were similar between the two groups (15.8 and 15% in the crush and provisional group, respectively; p = NS) while the incidence of definite ST was 1.7 and 1.1%, respectively. At 6 months no significant differences between the crush and provisional group with regard to restenosis rates in the MB (4.6 and 6.7%, respectively; p = NS) or the SB (13.2 and 14.7%, respectively; p = NS) were observed. The corresponding overall TLR rates were 5.6 and 5.8% (p = 1.00). Crossover to SB stenting was reported as 31%.
The British Bifurcation Coronary Study: Old, New, and Evolving Strategies (BBC ONE) study evaluated the clinical outcome of 500 patients undergoing bifurcation PCI, using paclitaxel-eluting stents (82% of the lesions were ‘true’ bifurcations) with either provisional T-stenting or both branch stenting with the crush or the Culotte technique [15]. At 9 months of follow-up the rates of MACE were significantly different between the two groups. (8.0% in the provisional group and 15.2% in the two-stent group; p = 0.009). The poorer outcome in the two-stent group was mainly due to higher rates of periprocedural (<30 days) myocardial infarction (11.2 vs 3.6% in the provisional group; p = 0.001). Definite ST was not significantly different between the two groups, although there was a numerical difference in favor of the provisional approach. Seven patients (3.0%) in the provisional group required SB stenting. Procedural and fluoroscopy times were significantly longer in the two-stent than the provisional approach.
These studies demonstrated that the strategy of systematic stenting of both the MB and SB offers no benefit over the strategy of stenting the MB only with provisional SB stenting, in terms of restenosis rates in both branches, TLR or overall MACE. Yet, implantation of two DES does not appear to be associated with a higher incidence of adverse events, at least up to 14 months following the procedure [7]. As a result, the provisional approach, which is less technically demanding and associated with significantly less procedure-related biomarker release is currently considered the primary strategy to bifurcation PCI when anatomically suitable. It is estimated that approximately 70% of true nonleft main bifurcations are currently being tackled with this approach [2].
Two-stent approach
Currently, bifurcation PCI with two stents is performed mainly as a crossover from a provisional strategy in case of suboptimal result in a large-sized SB (abrupt closure, flow-limiting dissection, >75% stenosis, TIMI flow <3). It should be recognized, however, that all studies that evaluated the provisional strategy included mainly bifurcations with focal, ostial SB lesions. Thus, what they demonstrated is the effectiveness of this approach in this type of lesions. Bifurcations involving large-sized SBs with extensive disease beyond the ostium or having a steep angle are much less likely to be treated optimally with a one-stent technique. It is estimated that approximately 30% of true nonleft main bifurcation lesions encountered in everyday practice warrant treatment with a two-stent technique [2].
Until now, there has been only one randomized study comparing two different two-stent strategies, that is The Nordic Stent Technique Study [16]. A total of 424 patients were randomized to either crush or culotte stenting. True bifurcation lesions were significantly more prevalent in the culotte group than in the crush group (82.3 vs 73.3%, respectively; p = 0.03) and final kissing-balloon inflation (FKI) was performed in significantly fewer patients in the crush group than in the culotte group (85 vs 92%, respectively; p = 0.03). At 6 months the rates of MACE were similar between the two groups (4.3% in the crush vs 3.7% in the culotte group; p = 0.87). The corresponding ST rates were 1.4 and 1.9% (p = 0.73). At 8 months, angiographic restenosis was low in both groups. There was a trend towards less restenosis in the entire lesion (MB and/or SB; 12.1% in the crush vs 6.6% in the culotte; p = 0.10), in the culotte group, which was due to significantly less SB in-stent restenosis (10.5% in the crush vs 4.5% in the culotte; p = 0.046) as compared with the crush group. The success rate of FKI was higher in the culotte group than the crush group, and may have have accounted for the higher SB instent restenosis rate observed in the latter group. Given the low MACE rates, this study was underpowered and could not definitely answer whether the crush or the culotte strategy is best in treating this type of bifurcation lesions.
A two stent approach as intention-to-treat strategy consists of implanting one stent across the MB and another across the SB. It is applied in ‘true’ bifurcation lesions where the SB is suitable for stenting and has disease extending >5 mm from its ostium. Adequate predilation of both branches to permit full stent expansion is mandatory and noncompliant balloons may be used for this purpose. Simultaneous FKI for carina reconstruction is also mandatory, whatever the technique used, and may also be performed with noncompliant balloons. However, high-pressure proximal MB inflation, using short noncompliant balloons, is often needed to correct the distortion that often occurs following kissing-balloon inflation [8]. A number of two-stent techniques are available, with various levels of complexity and indications: T-stent [1], crush [2], V stent/simultaneous kissing stents (SKS) [3] and culotte stenting [4]. These techniques are described in detail in the following text.
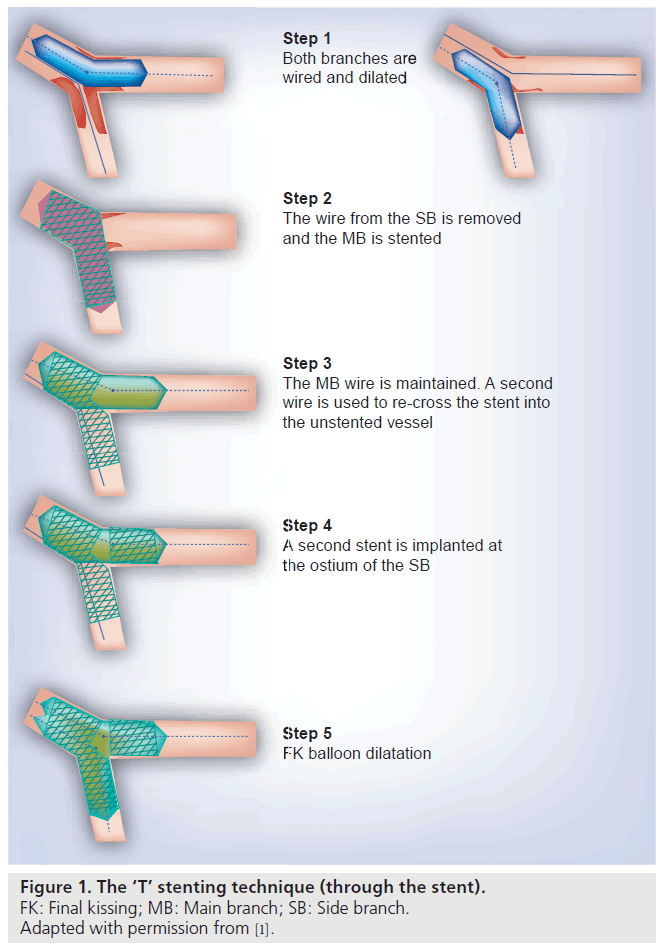
T-stent technique
The classic T-stent technique consists of delivering a stent in the SB, aiming to avoid protrusion in the MB and simultaneously cover the ostium of the SB as well as possible. Some operators leave a balloon in the MB or even inflate it at a low pressure to help precise SB stent positioning (Figure 1) [1,3]. The SB wire is then removed and the MB stent deployed. This is followed by SB rewiring, ostial SB dilation and FKI. The modified T-stent technique consists of simultaneously positioning stents at the SB and the MB [1]. The former is deployed first and then after wire and balloon removal from the SB, the MB stent is deployed. This technique is simple, particularly when compared with the crush and culotte, where recrossing and dilating the SB is more difficult. However, stenting the SB first has some drawbacks, such as accurate stent positioning at the ostium of the SB, is often difficult and the risk of leaving the ostium uncovered or having a large segment of the stent protruding in the MB is inevitable. In the latter case, advancement of a stent into the MB stent is hampered. MB balloon dilation, the use of a buddy-wire or rotablation may help navigate the MB stent across the bifurcation. Hence, the use of this technique is limited to bifurcations angled at 70°–90° (T-shaped bifurcations) in which acceptable ostial SB strut coverage with a minimal gap and stent overhang in the MB can be achieved. Indeed in bifurcations with angles close to 90°, the coverage of the ostium of the SB may be almost complete whatever the MB stent strut crossed. Owing to these drawbacks, some operators use this technique only as part of a provisional approach in case crossover to SB stenting is needed or to tackle an isolated ostial SB lesion (Medina class 0.0.1 lesion) [1,4]. The T-stenting and small protrusion technique (TAP) combines features of the T-technique and the crush technique [1,3,4]. After the MB has been stented with a jailed wire in the SB, the SB ostium is rewired and dilated through the MB stent struts after the jailed wire had been removed. Then a second stent is advanced in the SB so as to minimally protrude (1–2 mm) into the MB. A balloon is advanced in the MB and left uninflated during SB stent deployment at a pressure of ≥12 atm. The SB stent balloon is then pulled slightly back into the MB and kissing-balloon inflation is performed with simultaneous inflation of the two balloons. A final kissing with two noncompliant balloons may be performed. Excellent results have been described with the TAP technique; in one study long-term TLR rates were 6.8% [4]. There have been concerns regarding the protrusion of the SB stent into the MB, causing difficulty in advancing a stent distally, either to the MB or the SB that have not been confirmed. The T-stent technique (classic, modified or TAP) is suitable for bifurcation where the MB and the SB are of similar size [17].
Figure 1. The ‘T’ stenting technique (through the stent).
FK: Final kissing; MB: Main branch; SB: Side branch.
Adapted with permission from [1].
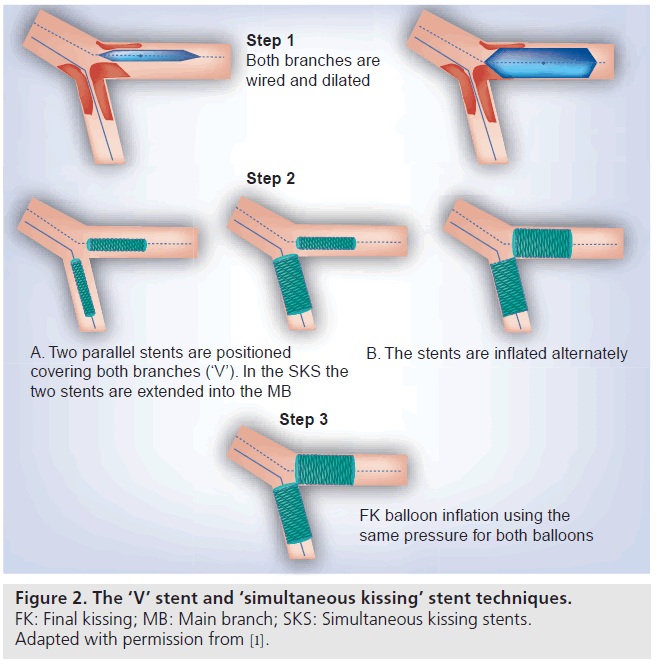
The V stent & the simultaneous kissing stent techniques
These techniques consist of implanting the MB and the SB simultaneously in a way to create a double-barrel, neocarina in the MB (Figure 2) [1,3–5,17]. When the neocarina created is rather long (≥5 mm) the technique is denominated as SKS. Many operators prefer to position the two stents within the branches, in such a way as to be sure that the ostia of the branches have been covered trying also to limit the protrusion to <5 mm. It may be necessary to advance the first stent more distally into the vessel to facilitate the advancement of the second. Having confirmed the correct alignment of the stents in two projections and proximal stent markers are overlapped, each stent is deployed individually at ≥12 atm, with the SB stent deployed first, and then both stent balloons are inflated simultaneously at 8–12 atm. Simultaneous deployment may result in shifting and misalignment of the proximal portion of the stents, hence it should be avoided. The procedure is completed with kissing-balloon dilation using short balloons inflated at 12–16 atm. At a mean follow-up of 9 months the TLR rates with this approach have been reported as 4% in one study [4].
Figure 2. The ‘V’ stent and ‘simultaneous kissing’ stent techniques.
FK: Final kissing; MB: Main branch; SKS: Simultaneous kissing stents.
Adapted with permission from [1].
The type of lesion that is considered suitable for this technique is a very proximal lesion, such as a bifurcation lesion located at the left main stem with a left main artery that is short or free of disease. The V technique can also be employed in other bifurcations, provided that the proximal MB is free of disease with the plaque mainly located distal to the carina and there is no need to implant a stent more proximally, such as Medina lesions 0.1.1. In addition, the proximal healthy segment must be sufficiently large to accommodate the proximal ends of two stents (typically it should be at least two thirds of the sum of the diameters of both bifurcation branches [Movahed BL2 lesions]) [9]. Ideally, the MB and the SB should be of a similar size and the angle between them <90°. This technique is both quick and safe with preserved access to both branches throughout the procedure and less hemodynamic instability. In addition, there is no need to recross any stent to perform kissing‑balloon dilation. The disadvantages of this technique include: the requirement of a guiding catheter of at least 7-Fr, the metallic neocarina, because of the concerns regarding its potential for inducing thrombosis, the possibility of gap formation beneath the overlapped portion of the stent, longitudinal stent overlap in a highangle bifurcation, distortion of the smaller stent promoted by a difference in size between the two stents and overdilation in the proximal segment [3]. If the proximal MB reference diameter is relatively small, the two balloons inflated simultaneously may be oversized thereby leading to dissection. This can be avoided by performing the kissing-balloon dilation at low pressure (4 atm). If the proximal MB disease is lengthy and the V/SKS techniques are contemplated a proximal MB stent may be deployed first (modified SKS technique) [4]. The V-technique is then performed as normal, taking care to deploy the stents in a way that their proximal portion will overlap with the distal portion of the proximal stent. The deployment of a stent proximal to the neocarina after V/SKS stenting has been completed can be very problematic. In such a case, either a stent is placed proximally leaving a small gap between the kissing stents and the proximal stent or alternatively, the double barrel can be extended proximally with two more stents or the SKS technique is converted into a crush. In the latter scenario the SB stent is compressed with a MB balloon. The SB is then rewired, redilated with a kissing inflation and the stent for the proximal segment is advanced toward the MB. In this case we are left with a short segment of the MB proximal to the bifurcation, which has four layers of struts. During rewiring the wire may possibly cross from the lumen of one stent to the lumen of the other, therefore IVUS is recommended to confirm that the correct lumen has been wired.
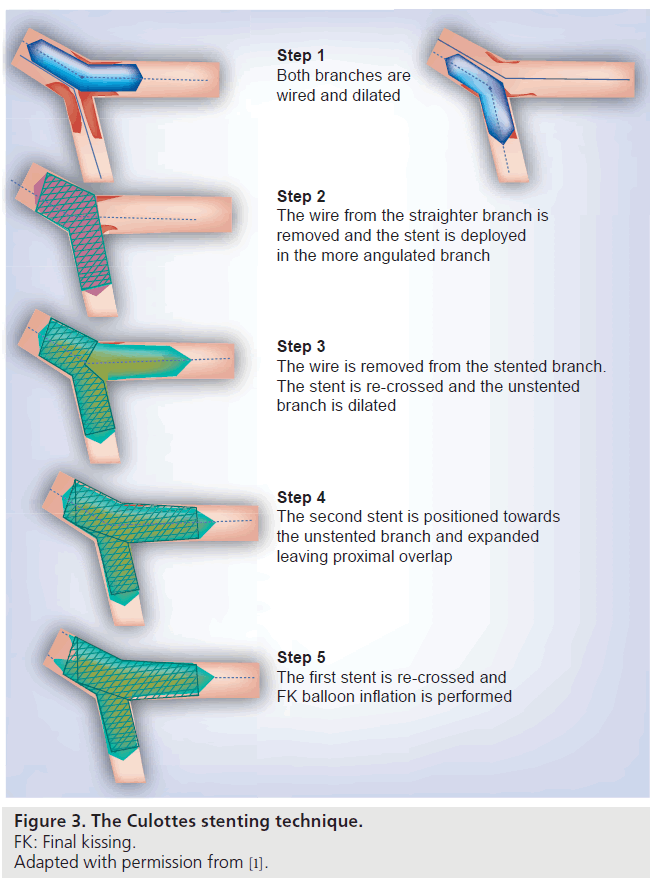
The Culotte technique
This technique consists of deploying a stent across the most angulated branch, usually the SB (inverted culotte) (Figure 3) [1,3–5,17]. The nonstented branch is then rewired, preferably through the distal strut, and dilated. A second stent is then advanced and deployed into the nonstented branch, usually the MB. The first stent is rewired and dilated, and separate high pressure dilations (>18 atm) are performed using noncompliant balloons. The procedure is completed with kissing-balloon dilation at 10–12 atm. This technique is considered best for large-sized vessels in a bifurcation angle <70° (Y-shaped); ideally the MB and the SB should be of a similar size (at least 3 mm in diameter). However, it allows tackling bifurcations with branches of different diameters and may be employed whatever the bifurcation angle; therefore, it can be employed in most bifurcations in which a two-stent approach is indicated. It probably provides the best coverage of the carina and it is compatible with a 6-Fr guiding catheter. The disadvantages of this technique are the excess of metal (double-stent layer) created over the carina and the proximal MB and the fact that rewiring both branches through the stent struts can be difficult and time consuming. In a bifurcation where the branches measure at least 3 mm in diameter, the sirolimus-eluting Cypher stent, which has a maximum achievable cell diameter of 3.0 mm, should probably be avoided as it is likely to have a suboptimal strut opening towards the branches. The Culotte technique, when appropriate, offers some advantages over crush stenting [8].
Figure 3. The Culottes stenting technique.
FK: Final kissing.
Adapted with permission from [1].
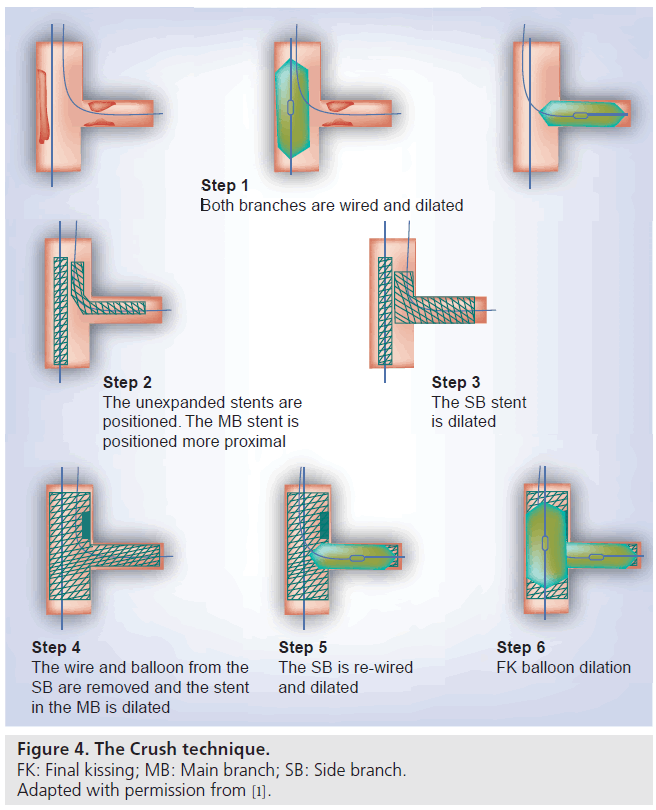
The crush technique & its variations
The crush technique has been proposed at a time when the T-stenting technique was the default two-stent approach in order to address the SB strut coverage issue (Figure 4) [1,3–5,17]. The idea was to allow some protrusion of the SB stent into the MB (usually 5–10 mm in the original description of the classical crush) in order to obtain better ostial SB strut coverage. The SB stent located in the proximal MB was then crushed against the MB stent. A subsequently proposed variation of the technique is the minicrush, in which only 1–2 mm of the SB stent are retracted proximal to the carina. As demonstrated by Ormiston et al., in an in vitro model the mini-crush, when compared with the classical crush, resulted in significantly less residual ostial SB stenosis (36 vs 47%, p = <0.002) and minimal multiple strut layering, while gaps in strut scaffolding and drug application in the SB ostium were less common [18]. The minicrush is performed as follows: following wiring and predilation of both branches the two stents are positioned by retracting the SB stent approximately 1–2 mm into the proximal MB. Following confirmation of the correct position of the stents in two projections, the SB stent is deployed with at least 12 atm and the balloon is deflated and removed into the guiding catheter. The result in the SB is then verified for appropriate lumen and normal flow and that no dissection or residual lesions are present. If a second stent is needed for the SB, this is the right time to deliver it. Then the SB wire is removed and the MB stent is deployed at high pressure, usually >12 atm crushing the SB stent. After removal of the MB stent balloon the SB is rewired through a proximal strut and twostep kissing-balloon inflation is performed. The latter consists of dilation of the SB at a high pressure (≥12 atm) followed by kissingballoon dilation at ≥8 atm. The two-step kissing- balloon inflation facilitates significantly less residual ostial SB stenosis when compared with the one-step kissing post-dilation technique where a single simultaneous kissing-balloon post-dilation is performed. When a two-stent strategy must be employed as an intention-totreat and only a 6-Fr guiding catheter is allowed (radial approach), the step crush or modified balloon crush technique can be used. In fact, this is the only situation in which this technique is used. The only difference with the classical crush is that the SB stent is crushed with a MB balloon. The double-kissing crush or ‘sleeve’ technique are performed to optimize stent expansion and apposition. The difference with the classical crush is that the SB stent is first crushed with a balloon in the MB, and then kissing-balloon inflation is performed followed by MB stenting and FKI. The reverse/internal crush is performed primarily as a provisional SB strategy. After MB stenting and kissing-balloon dilation the SB stent is positioned in a way to protrude a few millimeters into the MB stent. The MB balloon is then inflated at high pressure (≥12 atm) and crushes the SB stent. The SB stent is rewired, dilated at high pressure (12–20 atm) and the procedure is completed with kissing-balloon inflation.
Figure 4. The Crush technique.
FK: Final kissing; MB: Main branch; SB: Side branch.
Adapted with permission from [1].
A bifurcation angled at <70° is considered ideal for the crush technique, although outcomes may be better with bifurcations angled at <50°. The main advantage of the Crush technique is that the immediate patency of both branches is assured and the risk of SB occlusion is low; these features are particularly important if the SB is functionally relevant or difficult to be wired. Limitations are the need to re-cross multiple struts with a wire and a balloon to perform kissing-balloon dilation, difficulty to determine the position of the SB stent, difficulty in wiring the proximal ostial SB strut that is warranted for better ostial SB scaffolding and optimal carina reconstruction, and the potential of having more residual ostial SB stenosis with stents of limited maximum strut opening (<3.5 mm) [1,3,17,18].
Dedicated bifurcation stents
Dedicated bifurcation stents are designed to overcome limitations associated with conventional stents, such as SB protection and access, wire crossing through stent struts, multiple strut layering, ostial SB scaffolding gaps and stent deformation and/or disruption [19,20]. They are categorized into dedicated MB devices, which primarily provide access into the SB and only some coverage of the SB ostium, dedicated SB devices that are intended for primary SB treatment, dedicated MB plus SB devices that offer significant stent coverage of both branches but minimal coverage of the carina, and the MB stent with SB access port device that are designed primarily for MB stenting preserving access to the SB [19]. A number of studies evaluating this new technology demonstrated promising results; however, thus far studies have yet to demonstrate that these devices provide superior results relative to the conventional ones. More clinical data and randomized trials are needed before reaching definite conclusions as regards the efficacy and safety of this technology.
Conclusion & future perspective
Clinical experience with bifurcation PCI has demonstrated to us all that no two bifurcation lesions are the same and no single strategy exists to be employed in every bifurcation. An individualized lesion-specific approach and optimization of the performance of the technique are key steps to a successful bifurcation PCI. The consensus is that the strategy of routine implantation of two DES in bifurcation lesions does not improve either angiographic or clinical outcomes for most patients and that the provisional strategy should be the default approach in most bifurcation lesions. Lesions suitable for treatment with the provisional approach are those with SB disease confined to or extending <5 mm from the ostium whereas lesions with more extensive SB disease and/or a steep bifurcation angle (<60–70°) are best treated with a two-stent technique. In the latter scenario, achieving optimal stent expansion/ apposition across the ostia of both bifurcation branches is crucial and likely more important than the particular two-stent technique used. Reaching this task is greatly facilitated by the use of IVUS, which should be employed at least in the more complex cases. Furthermore, substantiation of the result at jailed SBs by the use of fractional flow reserve may enable a more rational approach to treating these vessels. These measures, if systematically applied, may further enhance the outcomes of bifurcation PCI, which nevertheless have already been substantially improved approximating those of nonbifurcation PCI. Expansion of the use of IVUS as well the introduction of new imaging modalities, such as optical coherence tomography in the field of bifurcation PCI to guide optimal stent positioning and expansion apposition, is warranted. Furthermore, these indications have revealed the compositional and morphological characteristics of the bifurcation lesions and more such data are likely to be revealed in the near future. More accurate characterization of bifurcation lesions may help matching a type of lesion to a specific technique. Dedicated bifurcation stents is a promising technology that may ultimately accommodate the limitations of conventional DES techniques, yet its efficacy remains to be demonstrated.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Executive summary
Bifurcation lesion classification schemes
▪ Coronary artery bifurcation lesions are markedly heterogeneous with regard to anatomy and the dynamic changes in anatomy that occur during treatment. The most suitable percutaneous coronary intervention strategy should be selected and optimized on an individual basis considering bifurcation characteristics that are known to influence the acute and long-term results.
▪ The Medina classification scheme has been validated by the European classification scheme and is widely used. It does not require memorization and gives the reader an immediate mental picture of the distribution of atheroma at the bifurcation level.
Provisional side branch stenting
▪ Stenting of the main branch only with provisional side branch (SB) stenting has been established as the default approach to the majority of bifurcation lesions. Lesions with SB disease confined to or extending < 5 mm from the ostium are considered suitable for treatment with this strategy.
Two-stent approach
▪ Currently, stenting of both bifurcation branches is performed mainly as a crossover from a provisional approach in case of a suboptimal result in a large-sized SB (≥2.5 mm in diameter). ‘True’ bifurcations involving large-sized SBs with extensive disease beyond their ostium or having a steep angle are considered suitable for treatment with this approach.
▪ Current evidence suggests that this approach is not associated with a significantly increased rate of stent thrombosis.
▪ Simultaneous final kissing inflation for carina reconstruction is mandatory whatever the technique used.
▪ In contrast to other two-stent techniques, the crush technique requires SB recrossing through a proximal strut and two-step kissingballoon inflation.
▪ The culotte technique, when appropriate, offers some advantages over crush stenting.
References
- Iakovou I, Ge L, Colombo A: Contemporary stent treatment of coronary bifurcations. J. Am. Coll. Cardiol. 46, 1446–1455 (2005).
- Latib A, Colombo A: Bifurcation disease: what do we know, what should we do? JACC Cardiovasc. Interv. 1, 218–226 (2008).
- Stankovic G, Darremont O, Ferenc M et al.: Percutaneous coronary intervention for bifurcation lesions: 2008 consensus document from the fourth meeting of the European Bifurcation Club. EuroIntervention 5, 39–49 (2009).
- Hermiller JB: Contemporary bifurcation treatment strategies: the role of currently available slotted tube stents. Rev. Cardiovasc. Med. 11(Suppl. 1), S17–S26 (2010).
- Sharma SK, Sweeny J, Kini SA: Coronary bifurcation lesions: a current update. Cardiol. Clin. 28, 55–70 (2010).
- Iakovou I, Schmidt T, Bonizzoni E et al.: Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA 293, 2126–2130 (2005).
- Jensen JS, Galløe A, Lassen JF et al.: Safety in simple versus complex stenting of coronary artery bifurcation lesions. The Nordic bifurcation study 14‑month follow-up results. EuroIntervention 4, 229–233 (2008).
- Hildick-Smith D, Lassen JF, Albiero R et al.: Consensus from the 5th European Bifurcation Club meeting. EuroIntervention 6, 34–38 (2010).
- Movahed MR, Kern K, Thai H, Ebrahimi R, Friedman M, Slepian M: Coronary artery bifurcation lesions: a review and update on classification and interventional techniques. Cardiovasc. Revasc. Med. 9, 263–268 (2008).
- Louvard Y, Thomas M, Dzavik V et al.: Classification of coronary bifurcation lesions and treatments: time for a consensus! Catheter. Cardiovasc. Interv. 7(3), 259–262 (2008).
- Louvard Y, Lefèvre T, Morice MC: Percutaneous coronary intervention for bifurcation coronary disease. Heart 90, 713–722 (2004).
- Steigen TK, Maeng M, Wiseth R et al.: Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic bifurcation study. Circulation 114, 1955–1961 (2006).
- Ferenc M, Gick M, Kienzle RP et al.: Randomized trial on routine vs. provisional T-stenting in the treatment of de novo coronary bifurcation lesions. Eur. Heart J. 29, 2859–2867 (2008).
- Colombo A, Bramucci E, Saccà S et al.: Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations: the CACTUS (Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus-Eluting Stents) Study. Circulation 119, 71–78 (2009).
- Hildick-Smith D, de Belder AJ, Cooter N et al.: Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions: the British Bifurcation Coronary Study: old, new, and evolving strategies. Circulation 121, 1235–1243 (2010).
- Erglis A, Kumsars I, Niemelä M et al.: Randomized comparison of coronary bifurcation stenting with the crush versus the culotte technique using sirolimus eluting stents: the Nordic stent technique study. Circ. Cardiovasc. Interv. 2, 27–34 (2009).
- Stankovic G, Mehmedbegovic Z, Zivkovic M: Bifurcation coronary lesions – Approaches to management. Interv. Cardiol. 5, 53–57 (2010).
- Ormiston JA, Webster MW, Webber B, Stewart JT, Ruygrok PN, Hatrick RI: The “crush” technique for coronary artery bifurcation stenting: insights from microcomputed tomographic imaging of bench deployments. JACC Cardiovasc. Interv. 1, 351–357 (2008).
- Rizik DG, Klassen KJ: Dedicated bifurcation devices. Rev. Cardiovasc. Med. 11(Suppl. 1), S27–S37 (2010).
- Colombo A: Bifurcational lesions and the “crush” technique: understanding why it works and why it doesn’t – a kiss is not just a kiss. Catheter. Cardiovasc. Interv. 63, 337–338 (2004).