Research Article - Clinical Practice (2022) Volume 19, Issue 3
The radial forearm free flap versus the nasolabial flap in adults having reconstructive surgery for oral cancer: a comparison of quality of life outcomes
- Corresponding Author:
- Molly Kate White
University of Edinburgh, United Kingdom
E-mail: 0mollyk@gmail.com
Received: 03 April, 2022, Manuscript No. fmcp-22-59369, Editor assigned: 05 April, 2022, PreQC No. fmcp-22-59369, Reviewed: 16 May, 2022, QC No. fmcp-22-59369, Revised: 20 May, 2022, Manuscript No. fmcp-22-59369, Published: 25 May, 2022, DOI. 10.37532/fmcp.2022.19(3).1942-1952
Abstract
Background: Surgical resection is the preferred treatment for tongue cancer. The Radial Forearm Free Flap (RFFF) has classically been used in oral reconstructions, however, there has been researching into an alternative option in the form of the Nasolabial Flap (NLF). Surgical research is becoming more and more focussed on Quality of Life (QOL) outcomes as a way to measure a successful recovery. As a result, this review has a focus on QOL as well as functional outcomes. Objective: The aim of this review is to determine if there are better QOL outcomes between patients undergoing tongue reconstruction with the NLF or the RFFF. The quality and limitations of the included papers will be discussed. Methods: Four databases were searched using set search terms and inclusion/exclusion criteria. These searches yielded fourteen final papers which were assessed using a CASP checklist and a bias tool for quality. Results: A variety of outcome measures were featured; despite this, all the papers found good functional and QOL results at follow-up. There were problems with bias throughout all the papers and several reoccurring limitations such as small sample size and the retrospective nature of all but one study. Conclusion: Due to the significant amount of bias found, the overall low quality of literature available, and discrepancies between outcome measures, further research is needed in the form of a long-term prospective study with a larger cohort that includes objective outcome measures.
Keywords
Tongue, reconstruction, hemiglossectomy, glossectomy, surgical flap, pedicled, speech, swallowing.
Introduction
Oral cancer is one of the few life-threatening oral cavity diseases still affecting the Western world [1]. The epidemiology and survival rates of oral malignancy vary depending on the specific region; however, tongue carcinoma, the most common of oral cancers representing 40% of all occurrences [2], in particular, is increasing in incidence. Primary surgical resection followed by possible adjuvant therapy is the standard treatment for oral cancer [3]. In the case of tongue cancer, this could involve full or partial removal of the tongue, a glossectomy, or hemiglossectomy [4]. In order to improve any functional impairment that the patient may be left with, reconstructive surgery can be performed. The reconstruction can be done by primary closure or secondary intention if the defect is small enough, but this will not restore any of the lost bulk. Therefore, the usual reconstructive technique after resection is with a surgical flap [5].
The two main styles of the flap are free and pedicled. A free flap is one that is taken from a spot on the body and moved to another with its blood supply, whereas a pedicle flap is one where the tissue is left partly attached to the donor site and the rest is oriented into the recipient site, leaving its blood supply intact [5].
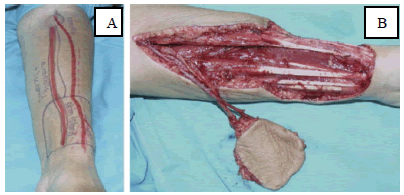
For the purposes of this review, the two flaps under consideration are the Nasolabial Flap (NLF) and the Radial Forearm Free Flap (RFFF). This is not only a comparison between locations of the body but also between flap techniques. The RFFF is the most commonly used flap for tongue reconstructions [6]. The RFFF can be used as a pedicled flap, however, this review will be focussing on the free flap technique (FIGURE 1).
Figure 1: A) Marking of the radial forearm free flap. B) Harvesting the radial forearm free flap [7].
With this flap, there tend to be quite high rates of donor site morbidity [8], meaning the skin graft used to heal the donor site may fail or the patient could be left with decreased sensation and strength [9].
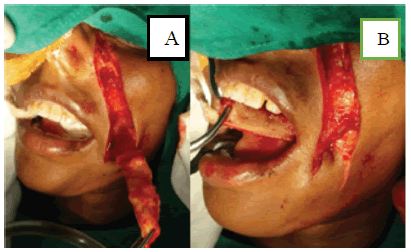
The other flap being considered in this review is the NLF. The flap can be taken unilaterally or bilaterally depending on the amount of tissue needed for reconstruction [10]. The flap technique can be islanded or pedicled, and if pedicled, it can be superiorly, inferiorly, or centrally based.
The location of the nasolabial fold typically allows for minimal donor site deformity after proper healing. The drawbacks of this flap are the limited amount of tissue available and the potential for facial asymmetry after surgery [10].
There are many different ways to measure a successful surgical recovery [12]. For tongue reconstructions specifically, the focus is on speech and swallowing function, and the majority of studies will perform a functional evaluation during follow-up [13,14]. As well, Quality of Life (QOL) is becoming more and more important in surgical trials as a measurement of how successful intervention has been [15]. The tool chosen to measure an outcome is just as important as the outcome itself [12], and this is something that will be discussed in depth in this review (FIGURE 2).
Figure 2: A) Dissected nasolabial flap. B) Nasolabial flap placed using a buccal tunnel [11].
The aim of this review is to determine whether there is a significantly greater improvement in QOL between patients undergoing tongue reconstruction with the NLF or the RFFF by appraising all qualifying literature from the last five years. The quality and limitations of the included papers will be discussed.
Methods
Four databases were searched on the 28th of February 2021 to find qualifying literature, these were: Ovid Medline, Ovid Embase, PubMed, and Cochrane Library. The advanced searches were completed using the following search terms, ‘[(Tongue) and (Recon* or Surgery) and (Flap) and (Nasolabial or Radial Forearm)]’.
The reporting of this review was guided by the standards of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [16]. The full PRISMA diagram including the reason for exclusion can be found in Appendix 1. After reviewing the full texts, 14 papers were found to meet all inclusion and exclusion criteria and qualified for this review. A five-year time frame (2015-current) was chosen to keep this review as relevant as possible and to ensure the currency of literature due to rapid advances in surgical approaches, especially in relation to the RFFF (TABLE 1).
TABLE 1. Inclusion and exclusion criteria were used to eliminate papers.
| Study Component | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | Adults | Children |
| Cancer patients | Noncancer patients | |
| Intervention | Primary oral reconstruction (including tongue) | Secondary reconstruction |
| Robotic surgery | ||
| Area of the body other than the oral cavity | ||
| No mention of tongue | ||
| Comparison | Any mention of nasolabial | No mention of nasolabial |
| Any mention of radial forearm | No mention of radial forearm | |
| Outcome | Focusses on more than one of speech/swallow/QOL | No mention of speech/swallow/QOL |
| Focusses on only one of speech/swallow/QOL | ||
| Quality of life in relation to the recipient site | Quality of life in relation to the donor site | |
| Study Design | Original Research | Case reports |
| Systemic reviews | ||
| Meta-analyses | ||
| Conference abstracts | ||
| Expert reviews | ||
| Publication | Published in 2015-current | Publication date older than 2015 |
| English | Any language other than English |
The study design for every paper was analyzed and classified using the Scottish Intercollegiate Guidelines Network algorithm [17]. Each of the final papers was appraised using a Critical Appraisal Skills Programme (CASP) checklist [18,19] specific to the study design. In addition, each paper was assessed for bias using the appropriate Cochrane bias tool and ROBINS-1 tool [20,21].
Results
A total of 14 papers met the inclusion and exclusion criteria for this review. These papers assessed at least two outcomes of interest for either the RFFF or the NLF.
■Study design
Of the final 14 papers that were analyzed in this review, 8 were cohort studies, 5 were case series, and 1 was a non-randomized controlled trial. All the papers focussed on flap reconstructions for oral carcinoma, specifically reconstructions of the tongue. Each paper included either the NLF or the RFFF.
■Population
The number of patients included in the studies was relatively low and ranges from 7 to 250 participants with only two studies having over 100 participants [22,23]. All of the studies drew their participants from the same single institute except for one [22], which included two centers to obtain a larger sample size. The studies varied in the amount and specificity of their inclusion and exclusion criteria. Four papers lost patients to follow-up [22-25], one paper did not state if anyone was lost to follow-up [26] and one paper excluded three patients from follow-up due to recurrence [27], leaving nine papers with complete follow-up data.
■Methods and outcome measures
The follow-up period for the studies ranged from one month to ten years. Five studies state that they received board approval and one states that the need for this was waived due to the de-identification of patient data [28]. Eleven studies included the RFFF and three included the NLF. All the studies measured postoperative speech and swallowing outcomes. Eight studies used subjective measurements for functional outcomes, two used objectives, three used both, and one study used objective measurements for speech but no information was provided on how swallowing results were obtained [29]. Six of the studies used the University of Washington Quality of Life questionnaire (UW-QOL) which is a commonly used questionnaire for head and neck cancer patients or based their questionnaire on it.
■Surgical outcomes
In eight papers, some patients received postoperative radio/chemotherapy, in one paper nobody received adjuvant radio/chemotherapy and the remaining papers did not identify whether participants had any adjuvant therapy. Three papers had complete flap failures in at least one patient, and all were with the RFFF [27,30,31]. In general, the papers found the RFFF to have significantly more donor site complications. Most of the papers had complications of varying types and quantities except for two studies [32,33], which state that all the procedures went smoothly with no flap failures or complications, and both of these papers focus on the NLF.
■Functional outcomes
All the papers had good functional outcome measure results at follow-up. Of the papers that involved a comparison, five of them found there to be no statistically significant difference between the groups for functional outcomes [25,26,28,30,31]. One of these papers did however find a significant difference between groups for follow-up times [25]. Li, et al [24] found there to be significant differences between groups for the appearance and shoulder domains of the UW-QOL questionnaire, they also found significant differences between the groups for psychological discomfort and social disability from the 14-item Oral Health Impact Profile questionnaire (OHIP-14). Zhang, P et al [22] also used the UW-QOL questionnaire and they found there to be clinically and statistically significantly better scores for recreation, swallowing, chewing, and speech in the FRFF group compared to ALTF. They also found that the ALTF group had clinically significantly higher scores in the saliva domain. This study also used the Performance Status Scale for Head and Neck Cancer Patients (PSSHN) which found significantly higher scores in understandability of speech and normalcy of diet in the FRFF group. Cai, et al [34] found the RFFF group to have better recovery of speech and deglutition function, these were non-significant however there were significantly better scores for tongue flexibility in the RFFF group. The RFFF group had significantly higher scores for activity and recreation in the study done by Zhang, J et al [23]. The remainder of the studies all found acceptable and satisfactory results for speech and swallowing and those with multiple follow-ups found that the results improved over time [27,32,35].
■Stated limitations
Eight of the papers had no self-identified limitations. Of the remaining six papers, two identified that the retrospective nature of their study was a limitation [22,35]. Small sample size was identified in five papers as being a problem [23,24,28,32,35]. Exclusively using subjective measurements and no technical examinations were stated as a limitation in two papers [32,35]. One study stated the simplicity of their questionnaire to be a possible limitation [35], they also stated their evaluation modality was not sufficient for clinical research. Two papers stated how the lack of preoperative measurements was a limitation to their study [22,32]. One of these papers also identified their short follow-up time [32]. One paper identified the possible confounding of some patients receiving adjuvant radio/chemotherapy postoperatively [24]. This study along with one other [22], stated the non-randomized nature of their study to be a limitation.
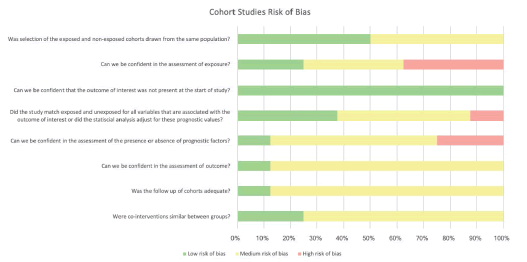
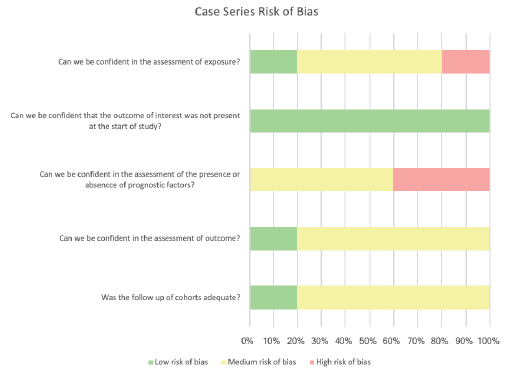
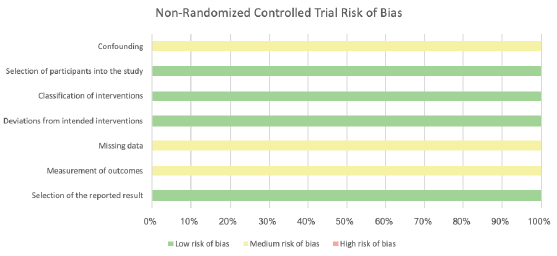
■Bias
The overall bias for all the papers was either medium or high risk. To a degree, this was to be expected as all but one of the papers were case series or cohort studies which are prone to bias as a result of the study design [36]. The assessments utilizing the Cochrane bias tools [20,21] are presented as part of the discussion as FIGURES 3-5.
Discussion
This review aims to determine whether there is a significantly greater improvement in QOL between patients undergoing tongue reconstruction with the NLF or the RFFF. The included studies and their results have been outlined above. Relevant sources of bias will now be discussed in more depth, followed by an appraisal of the outcome measures used and the limitations of the included studies.
■Performance bias
Performance bias is often present in trials that are not able to be randomized [37]. It results from differences that occur due to knowledge of which intervention was allocated to whom. Since many studies are unable to blind their participants, the risk of performance bias can be reduced by using objective outcome measures [37] which are much less susceptible to this kind of bias. Subjective vs objective outcome measures will be discussed further below.
■Co-intervention bias
For this review, an important subset of performance bias is co-intervention bias. This occurs when the amount and type of additional treatments on top of the main intervention being studied are not balanced between groups and could impact the outcome of interest [37]. In the context of oral cancer resection and reconstruction, postoperative adjuvant radio-chemotherapy, in addition to surgery, is relatively common and can improve results. The benefits of postoperative radiotherapy for oral squamous cell carcinoma were originally demonstrated in a 1996 randomized clinical trial in India [38]. They found that compared to surgery alone, the addition of radiotherapy postoperatively improved disease-free survival by 30% (p<0.005). The benefits are clear; however, the problem is when the amount of adjuvant treatment is not balanced between the groups. Zhang P, et al. [22] and Zhang J, et al. [23] provided the criteria they had for which patients received radiotherapy in addition to surgery. The numbers of patients who received it in each group ended up being similar in both studies. Two papers [28,34] mentioned that some patients received adjuvant treatment. However, no criteria or numbers for each group were provided, and as a result, it is unknown whether the treatment was spread evenly between the groups therefore the possibility of co-intervention bias cannot be eliminated in these cases.
■Information Bias
Information bias can present itself during outcome measurement [39]. It is commonly found in observational studies especially retrospective ones [37,39]. Studies that involve some sort of self-reporting [37], as many of those included in this review, are at an even higher risk.
■Measurement Bias
Measurement bias, also known as detection bias, can occur if the outcome assessor is not blinded to the intervention status of the participant [37]. Liang et al. [26] and Nguyan et al. [27] both blinded their outcome assessors. Liang et al [26] clearly state that the outcome questionnaire was given by a qualified member of staff blinded to the study. Nguyan et al [27] do not use the word blind; however, they say that the functional evaluation was done by three untrained volunteers with no knowledge of the patients; this can be interpreted as blinding. The blinding in these two studies will ideally prevent or minimize systemic differences in measurements between groups [40].
■Observation Bias (Hawthorne Effect)
Observation bias occurs when the participant is aware that they are being observed and alter their answers or actions. This may be conscious or unconscious [41]. This has been described as the Hawthorne effect [37]. Tom Brody states in Chapter 7 of the second edition of Clinical Trials [42] that the Hawthorne effect can influence the participant’s responses to health-related QOL tools. This is relevant as the majority of the papers included in this review used questionnaires (FIGURES 4 AND 5).
Five papers had the participants complete the questionnaires themselves with no observation. Of the remaining papers, seven had participants complete their functional assessments in person with an assessor present [27-31,34,35]. This makes these studies susceptible to observation bias. For objective speech assessments like that of Cai, et al [34], the patient may be more nervous, which could make them speak faster or even stutter. Two studies performed the questionnaires over the telephone [22,26]. The literature does not include a comparison between telephone and in-person interviews and the Hawthorne effect; however, an assumption can be made that a telephone interview would lessen any potential observation bias, at least to a degree, as there is no direct observation occurring.
■Appraisal of Outcome Measures
The type of outcome measure chosen, how it is implemented, and when the data is collected are all important. The different outcome measures used will be appraised in this section, outlining the strengths and weaknesses and when possible, the most ideal option for the specific scenario of tongue reconstruction.
■Subjective vs. Objective Measures
Both subjective and objective measures are demonstrated throughout the included literature. In the context of QOL assessments and functional evaluations, it is important to determine whether subjective or objective measures are superior.
In terms of measuring speech function, five studies [27-29,31,34] chose to use objective measures while the remainder used a subjective measure. The results from those studies that used objective measures are comparable to those that chose subjective ones. This suggests that for speech outcomes after tongue reconstruction, objective or subjective assessments are both sufficient and yield similar results. This is supported by a study Cox, et al. [43]. Their study compared the use of objective and subjective measures for speech intelligibility in elderly hearing-impaired listeners and found that when they compared the two types of scores they were closely related in both groups of subjects.
A study by Ding et al. [44] compared patients’ perceptions of swallowing difficulties to expert analysis by video fluorography. They found that while many patients were able to describe the same swallowing problem which was later confirmed by the expert, there were also quite a few patients who showed inconsistencies between their self-perception and the expert rating. The inconsistencies were lowest in the patients with general medical diagnoses, medium in those with structural deficits, and high in those with neurological disorders [44]. Oral cancer would be included in the structural deficits category as after reconstruction, the goal of the swallowing assessment is to see if a deficit remains. Eleven of the 24 patients (46%) in this group showed inconsistencies between their perceptions and the experts [44]. These results show that while subjective assessments may appear sufficient, ideally they should be reinforced with additional objective analysis. Nguyen et al. [27] and Lu et al. [31] both used objective measures to assess swallowing function, so therefore their results for swallowing are most reliable.
■Differences Between the Tools Used
There were six pre-established tools used to assess multiple domains within the papers. Six papers [22-25,32,33] used the UW-QOL questionnaire or parts of it, and Liang et al. [26] based their questionnaire on it. Two studies used the OHIP-14 questionnaire, Yuan et al. [25] and Li et al [24], Yuan et al. [25] also used the European Organization for Research and Treatment of Cancer Quality of Life questionnaire [EORTC-QLQ-H&N35] [45]. The final tool is the PSS-HN scale, which was used by Zhang P et al. [22].
The UW-QOL questionnaire involves 12 domains as well as additional questions on which domains are the most important to the participant and three direct questions on QOL. The three domains of the PSS-HN scale are normalcy of diet, public eating, and understandability of speech. This questionnaire has the fewest domains, and the information from these domains is also gathered in the other three questionnaires. EORTC-QLQ-H&N35 [45] and OHIP-14 both have seven domains; however, they have different foci. The OHIP-14 questionnaire, as the title suggests, has a focus on oral health and is strongly disability-oriented. The questions address psychological factors so somewhat QOL, however, the questions are quite leading. The other questionnaire with seven domains is the EORTC-QLQ-H&N35 [45]. This tool collects some information that the UW-QOL does not, namely: information on the sense of smell, social eating, social contact, and sexuality. There is a newer version of this tool EORTC-QLQ-H&N43 [45] which has additional questions regarding skin problems, neurological symptoms, and shoulder problems which may be a better option.
The UW-QOL is the longest and most commonly used questionnaire in the studies considered in this review and that is likely due to its direct questioning of the patient’s opinion on their QOL [46]. The questions are posed in a way that relates each aspect to QOL. Another benefit of this option is asking the patient which three domains are most important to them. This approach can help guide future treatment and support to the creation of a more personalized treatment plan. Given the specificities and focus of each questionnaire, the right one for a study should be determined by taking into account which specific aspects the study wishes to evaluate [46]. In this case, where QOL is the focus, the UW-QOL questionnaire is the superior option [46] but it is ultimately up to the researcher’s discretion.
■When They Were Used Follow-Up Time
Follow-up time for surgical studies should extend to at least 12 months [47]. Despite the notable variation in the time frame of outcome measures, there were no drastic differences found between any of the studies regardless of follow-up time, however, within one study [35], a significant difference between the functional outcome results at 1 year versus 5-year followups was found. By only looking at the results there may not appear to be any obvious need for a minimum follow-up time however, considering the wider context that these are surgical trials and that functional outcomes are shown to improve sequentially over time [35], these measures are likely most accurate and reliable at least 12 months after intervention regardless of intervention type.
This section outlines the differences between the papers and what the effects of those differences are. In some cases, there is a preferred option and the majority of the differences hinder the comparison of the papers’ results. Standardization across all areas not only makes it easier to compare the outcomes of the studies but also works to minimize bias.
Limitations of the Papers
Six out of the fourteen papers identified limitations of their study [22-24,28,32,34]. The importance of two of these identified limitations will be described in detail along with one additional unidentified limitation.
■Identified
No Technical Examinations: As mentioned above, subjective measures should be backed up by additional objective measures at least for swallowing outcomes [44]. The lack of technical examinations was identified by Akashi et al. [35], while Nueangkhota et al. [32] made a similar statement in their limitations that functional evaluation by patient’s subjective perceptions was a limitation. The remaining eight papers with no objective measures did not state this as a limitation.
Adjuvant Chemo/Radiotherapy: During the process of appraising the papers using the CASP checklists [18,19], one of the important possible confounders was any adjuvant therapy and if the amount and type were balanced between groups. As stated previously, eight papers mentioned that some participants received adjuvant chemo/radiotherapy. However, only Li et al. [24] included this as a possible limitation by saying that some patients’ QOL may have been affected by this adjuvant therapy. This highlights a further issue in addition to simply ensuring the amount of adjuvant treatment is balanced between the groups and that is its possible impact on QOL. As QOL is an important outcome measure for many of these papers, as well as the overarching theme of this review, this is important to keep in mind for the papers that include adjuvant therapy [22-25,28,32-34].
■Unidentified
Non Generalizable: All of the included studies are not able to be generalized to the greater population mainly because the sample sizes are simply too small to be representative [48]. Another issue with the sample population that can affect generalizability is how participants are recruited. In retrospective studies, the most common sampling method used is convenience sampling [49]. This is the case in the included papers of which all but one [23] are retrospective studies. This method is when the researchers select patients for their study based on availability and accessibility [49]. This strategy is cheap, efficient, and simple which is why it is so commonly used, however it makes the results unable to be generalized to the whole population. All the previously mentioned threats to the validity of the studies such as biases also hinder a study’s generalizability.
All studies will have limitations [this is the nature of research], however, it is still important to declare them and ideally, to lay out how they could have affected the study.
Limitations
This review does have some limitations. Of the fourteen total papers included, only three are about the use of the NLF [30,33,34]. There is much more literature surrounding the RFFF and it is a limitation that there is not a more even number of papers to compare for each flap type. The inclusion and exclusion criteria shown in TABLE 1 could be interpreted differently by someone other than the author of this review, specifically when looking at the outcome criteria. This means that there is some subjectivity in the screening process which hinders the reproducibility of this review. As outlined in the discussion, there were a variety of outcome measures used throughout the papers as well as issues with comparability. Ideally, there would be a level of standardization in the outcome measures so as to better interpret and compare the results. The limitations of the primary studies, including biases and small sample size, addressed in the body of the discussion, are limitations to this review as well.
Suggestions for future research
There were many comparisons included in this review, yet none directly compared the RFFF with the NLF for tongue reconstruction. There is sufficient evidence of the benefits to QOL outcomes with NLF reconstruction with Sharma et al. [35] naming it the “locoregional flap of choice and an alternative to free flap for tongue reconstruction” [35]. This review has provided an idea of how the NLF stands up to the usual choice of the RFFF for tongue reconstruction, however, a direct comparison is needed so as to minimize any possible confounders and biases present. As addressed in this review, the quality of the papers available on this topic is not ideal. Future research on this comparison as well as on these two flaps individually should make an effort to perform a longer prospective study using a larger cohort and objective evaluations, at least for swallowing function. The area of research and specific topic has been well described, however it is the quality of the studies performed that is lacking. Future research should attempt to ensure a higher level of validity and minimize bias.
Implications for practice
Due to the low number of included studies and the relatively poor quality throughout, recommendations cannot be made directly from this review. Further stronger quality research must be undertaken, including a direct comparison between the RFFF and NLF for tongue reconstruction in order to close the gaps in the research. The main conclusions gathered from this review are regarding the quality of the included studies and the general lack of high-quality research available on this topic. Therefore, the findings of this review will likely be of more importance to academics than to policymakers and can hopefully guide future research.
Conclusion
This review has presented the QOL and functional outcomes of the fourteen included papers that focus on either the RFFF or NLF. It has discussed the main sources of bias in the papers and any limitations as well as performed an appraisal of the outcome measures used throughout the included studies. Due to the significant amount of bias found, the overall low quality of literature available, and discrepancies between outcome measures, further research is needed in the form of a long-term prospective study with a larger cohort and some objective outcome measures. This review set out to discover if one flap type offers a better recovery of QOL over the other. Evidence is still inconclusive however, this review has provided more insight into the problems with the current literature, and therefore can serve to guide future research for academics.
References
- Zini A, Czerninski R, Sgan-Cohen HD. Oral cancer over four decades: epidemiology, trends, histology, and survival by anatomical sites. J Oral Pathol Med. 39, 299-305 [2010].
[Google Scholar] [Crossref] - Kirita T, Omura K. Oral Cancer Diagnosis and Therapy. Japan, Springer. [2015].
[Google Scholar] [Crossref] - Kamrani P, Sadiq NM. Anatomy, head and neck, oral cavity [mouth]. Treasure Island [FL]. StatPearls. [2020].
[Google Scholar] [Crossref] - University of Rochester Medical Center. Oral cancer: surgery. URMC. [2021].
- Kaur1 R, Sahni VR, Satyapal S, et al. Functional outcomes of oral tongue reconstruction: A subjective analysis. J Head Neck Physicians Surg. 7, 26-31 [2019].
[Google Scholar] [Crossref] - Megerle K, Sauerbier M, Germann G. The evolution of the pedicled radial forearm flap. Hand [NY]. 5, 37-42 [2010].
[Google Scholar] [Crossref] - Maciejewski A, Szymczyk C, Poltorak S, et al. Tracheal reconstruction with the use of radial forearm free flap combined with biodegradative mesh suspension. Ann Thorac Surg. 87, 608-610 [2009].
[Google Scholar] [Crossref] - Jaquet Y, Enepekides DJ, Torgerson C, et al. Radial forearm free flap donor site morbidity: ulnar-based transposition flap vs split-thickness skin graft. Arch Otolaryngol Head Neck Surg. 138, 38-43 [2012].
[Google Scholar] [Crossref] - Engel H, Huang JJ, Lin CY, et al. A strategic approach for tongue reconstruction to achieve predictable and improved functional and aesthetic outcomes. Plast Reconstr Surg. 126, 1967-1977 [2010].
[Google Scholar] [Crossref] - Rahpeyma A, Khajehahmadi S. The place of nasolabial flap in orofacial reconstruction: A review. Ann Med Surg [Lond]. 12, 79-87 [2016].
[Google Scholar] [Crossref] - Kumar L, Bhasker P, Pol SA. Inferiorly pedicled nasolabial flap for extra-articular trismus. Otorhinol Head Neck Surg. 5, 1-2 [2020].
[Google Scholar] [Crossref] - Myles PS. More than just morbidity and mortality-quality of recovery and long-term functional recovery after surgery. Anaesthesia. 75, e143-e50 [2020].
[Google Scholar] [Crossref] - Hsiao HT, Leu YS, Lin CC. Tongue reconstruction with free radial forearm flap after hemiglossectomy: a functional assessment. J Reconstr Microsurg. 19, 137-142 [2003].
[Google Scholar] [Crossref] - De Vicente JC, Villalain, Torre A, et al. Microvascular free tissue transfer for tongue reconstruction after hemiglossectomy: a functional assessment of radial forearm versus anterolateral thigh flap. J Oral Maxillofac Surg. 66, 2270-2275 [2008].
[Google Scholar] [Crossref] - Urbach DR. Measuring quality of life after surgery. Surg Innov. 12, 161-165 [2005].
[Google Scholar] [Crossref] - Page MJ, Bossuyt PM, Boutron I, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 372, n71 [2021].
[Google Scholar] [Crossref] - Oral cancer over four decades: epidemiology, trends, histology, and survival by anatomical sites
- Critical Appraisal SKills Programme. CASP cohort study checklist. CASP. [2018].
- Critical Appraisal Skills Programme. CASP randomized controlled trial checklist. CASP. [2018].
- Cochrane. Tool to assess risk of bias in cohort studies. Methods Cochrane. [2021].
- Sterne JAC, Hernan MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 355, i4919 [2016].
[Google Scholar] [Crossref] - Zhang PP, Meng L, Shen J, et al. Free radial forearm flap and anterolateral thigh flap for reconstruction of hemiglossectomy defects: A comparison of quality of life. J Craniomaxillofac Surg. 46, 2157-2163 [2018].
[Google Scholar] [Crossref] - Zhang J, Wang Y, Han X, Chen H. Comparison of clinical results and quality of life in tongue cancer patients undergoing submental island flap and radial forearm free flap reconstruction. J Oral Maxillofac Surg Med Pathol. 78, 1639-1644 [2020].
[Google Scholar] [Crossref] - Li W, Zhang P, Li R, Liu Y, Kan Q. Radial free forearm flap versus pectoralis major pedicled flap for reconstruction in patients with tongue cancer: Assessment of quality of life. Med Oral Patol Oral Cir Bucal. 21, e737-e42 [2016].
[Google Scholar] [Crossref] - Yuan Y, Zhang P, He W, et al. Comparison of Oral Function: Free Anterolateral Thigh Perforator Flaps Versus Vascularized Free Forearm Flap for Reconstruction in Patients Undergoing Glossectomy. J Oral Maxillofac Surg Med Pathol. 74, 1500.e1-1500.e6 [2016].
[Google Scholar] [Cross Ref] - Liang Y, Cui Y, Liao G. Comparison of quality-of-life in tongue cancer patients undergoing tongue reconstruction with lateral upper arm free flap and radial forearm free flap. Int J Clin Exp Med. 8, 4533-4538 [2015].
[Google Scholar] - Nguyen KA, Bui TX, Van Nguyen H, et al. Progressive functional improvement in hemiglossectomy defects reconstructed with radial forearm free flap at 6-months. Am J Otolaryngol. 39, 317-320 [2018].
[Google Scholar] [Cross Ref] - Ng MJM, Goh CSL, Tan NC, et al. A head-to-head comparison of the medial sural artery perforator versus radial forearm flap for tongue reconstruction. J reconstr Microsurg. 37, 445-452 [2021].
[Google Scholar] [Cross Ref] - Shah GH, Misra G, Meena A, et al. Pedicled Islanded Nasolabial Flap Tunneled Under Mandible For Tongue Reconstruction. J Maxillofac Oral Surg. 20, 100-104 [2019].
[Cross Ref] - Zhang S, Chen W, Cao G, et al. Pedicled supraclavicular artery island flap versus free radial forearm flap for tongue reconstruction following hemiglossectomy. J Craniofac Surg. 26, e527-e530 [2015].
[Google Scholar] [Cross Ref] - Lu M, Sun G, Hu Q, et al. Functional assessment: Free thin anterolateral thigh flap versus free radial forearm reconstruction for hemiglossectomy defects. Med Oral Patol Oral Cir Bucal. 20, e757-e762 [2015].
[Google Scholar] [Cross Ref] - Nueangkhota P, Liang YJ, Zheng GS, et al. Reconstruction of tongue defects with the contralateral nasolabial island flap. J Oral Maxillofac Surg. 74, 851-859 [2016].
[Google Scholar] [Cross Ref] - Sharma V, Pandey S, Gandhi AK, et al. Island nasolabial flap for tongue reconstruction: locoregional flap of choice and an alternative to free flap for tongue cancer. Indian J Surg Oncol. 12, 94-99 [2021].
[Google Scholar] [Cross Ref] - Cai YC, Li C, Zeng DF, et al. Comparative analysis of radial forearm free flap and anterolateral thigh flap in tongue reconstruction after radical resection of tongue cancer. ORL J Otorhinolaryngol Relat Spec. 81, 252-264 [2019].
[Google Scholar] [Cross Ref] - Akashi M, Hashikawa K, Sakakibara A, et al. Long-term follow-up study of radial forearm free flap reconstruction after hemiglossectomy. J Craniofacial Surg. 26, 44-47 [2015].
[Google Scholar] [Cross Ref] - Ramirez-Santana M. Limitations and biases in cohort studies, cohort studies in health sciences. Intechopen. [2018]
- Catalogue of Bias. Catalogue of Bias. Catalogue of Bias. [2021].
- Mishra RC, Singh DN, Mishra TK. Post-operative radiotherapy in carcinoma of buccal mucosa, a prospective randomized trial. Eur J Surg Oncol. 22, 502-504 [1996].
[Google Scholar] [Cross Ref] - Ranstam J. Bias in observational studies. Acta Radiol. 49, 644-645 [2008].
[Google Scholar] [Cross Ref] - British Medical Journal. Appendix, The seven domains of bias addressed in the ROBINS-I assessment tool. BMJ. [2021].
- Understanding Health Research. Common sources of bias. Unders Health Res. [2021].
- Brody T. Clinical Trials, Second Edition. Amsterdam. Elsevier Inc. Chapter 7 Placebo Arm as Part of Clinical Trial Design. 155-172 [2016].
[Google Scholar] - Cox RM, Alexander GC, Rivera IM. Comparison of objective and subjective measures of speech intelligibility in elderly hearing-impaired listeners. J Speech Hear Res. 34, 904-915 [1991].
[Google Scholar] [Cross Ref] - Ding R, Logemann JA. Patient self-perceptions of swallowing difficulties as compared to expert ratings of videofluorographic studies. Folia Phoniatr Logop. 60, 142-150 [2008].
[Google Scholar] [Cross Ref] - EORTC Quality of Life. Quality of life group website. QOL EORTC Org. [2021].
- De Araujo Gomes EPA, Aranha AMF, Borges AH, et al. Head and neck cancer patients’ quality of life: analysis of three instruments. J Dent [Shiraz]. 21, 31-41 [2020].
[Google Scholar] [Cross Ref] - Dzioba A, Aalto D, Papadopoulos-Nydam G, et al. Head and neck research network. functional and quality of life outcomes after partial glossectomy: a multi-institutional longitudinal study of the head and neck research network. J Otolaryngol Head Neck Sur. 46 [2017]
[Google Scholar] [Cross Ref] - Simmons AE. The Disadvantages of a Small Sample Size. Sciencing. [2018].
- Edgar TW, Manz DO. Exploratory Study, Research Methods for Cyber Security. Amsterdam. Elsevier Inc. 106p [2017].
[Cross Ref]