Research Article - Clinical Investigation (2018) Volume 8, Issue 4
The effect of nurses' communication skills with Nulliparous mothers on exclusive breastfeeding: A Clinical Trial Study
Mamak Shariat1, Nasrin Abedinia2*, Fedyeh Haghollahi3, Ahmad Ali Noorbala4, Akram Karimi5 and Jayran Zebardast6
1Institute of family health, maternal, fetal and neonatal Health Research Center, Vali ASR Hospital, Imam Khomeini hospital complex, Tehran University of medical sciences (TUMS). Tehran, Iran
2Institute of family health, maternal, fetal and neonatal Health Research Center, Vali ASR hospital, Imam Khomeini hospital complex, Tehran University of Medical Sciences, (TUMS), Tehran, Iran
3Institute of family health, Vali Asr Reproductive Health Research Center, Vali ASR hospital, Imam Khomeini hospital complex, Tehran University of medical sciences (TUMS), Tehran, Iran
4Psychosomatic Department, Imam Khomeini hospital complex, Tehran University of medical sciences (TUMS), Tehran, Iran
5Akbar Abadi Health Center, Tehran, Iran.
6Electronic learning in medical education, statistics expert, Deputy of affairs, Imam Khomeini Hospital, Tehran University of Medical sciences, Tehran, Iran
- Corresponding Author:
- Nasrin Abedinia
Institute of family health, maternal, fetal and neonatal Health Research Center, Vali ASR hospital, Imam Khomeini hospital complex, Tehran University of Medical Sciences, (TUMS), Tehran, Iran
E-mail: Nasrin.Abedinia@gmail.com
Submitted Date: 03 September 2018; Accepted Date: 23 September 2018; Published Date: 27 September 2018
Abstract
Exclusive breastfeeding (EBF) in the first six months of life has many benefits for mother and newborn. The purpose of the present study was to investigate the effect of medical staff communication skills training on breastfeeding in nulliparous mothers. This is a clinical trial study. One hundred- seventy nulliparous pregnant women were selected from Vali-e-Asr Hospital of Tehran. The samples were divided into two groups of intervention (n=85) and control (n=85) by randomized blocks method. The intervention in this study was in the form of therapeutic communication training to the ten nurses in delivery emergency department ward on how to communicate with mothers. The Therapeutic communication skills training course consisted of four communication skills (Empathy skills, Interpersonal skills, Stress and emotional management). Chi-square test and analysis of variance were used to analyze the data and compare the groups. There was a significant difference between the two groups regarding the exclusive breastfeeding for 6 months (P=0.046).The frequency of exclusive breastfeeding in interventional group was higher than the control group (37.5% vs. 23.5%). At six months old, the babies in the study group grew more than the control group (8218.82 ± 2308.57 vs. 7442.23 ± 1923.27 gr, p=0.018) The professional therapeutic relationship of medical staff with the mothers led to an increase in exclusive breastfeeding and continuation of breastfeeding in the first 6 months of childbirth. It seems that breastfeeding is associated with the higher baby growth and lower use of formula feeding.
Keywords
Nursing education researchs, Breastfeeding, Exclusive breastfeeding, Medical staff, Mothers, Intervention
Introduction
Breastfeeding in the health of mothers and babies is a widely accepted issue. In this regard; in the statement released by the American Academy of Pediatrics in 1997, it was noted that breast milk was the golden standard for the nutrition of healthy and mature infants up to the first 6 months of their life [1-3].
Exclusive breastfeeding (EBF) refers to mere nutrition by breast milk but no other foods and liquids for infants. In this respect; age of marriage, level of education, socio-economic status, and attitudes to breastfeeding, breastfeeding problems and support resources for mothers, maternal self-confidence and self-efficiency are as well recognized among the factors affecting EBF. These factors have also intervening impacts on the duration of breastfeeding [4].
In a report from 94 countries across the world in 2003, the WHO declared that only 35% of infants were exclusively breastfed up to 4 months of age. Nowadays, the most important index for successful implementation of breastfeeding programs across the world is EBF within the first 6 months after birth. The EBF rate in Iran was reported 49.1 % [5-7].
Beliefs as well as positive tendency and attitudes could increase the duration of breastfeeding.
Professional healthcare system especially nurses have likewise positive and negative effects on breastfeeding and its duration [8]. One of the important factors affecting the breastfeeding and its duration is the effective therapeutic communication by specialists and medical staff [9,10].
However, some investigations suggested that levels of knowledge in healthcare specialists in terms of breastfeeding were often inadequate and affected by their own experiences [11,13]. As well, the communication between nurses and mothers could have affected the maternal self-esteem, a sense of self-control and emotional bond between mothers and babies [14].
In the nulliparous women, the delay of starting the breastfeeding decreases the rate of EBF. This problem may be due to several reasons including inadequate postpartum support by nurses as well as breastfeeding problems such as sore nipples and insufficient breast milk [15,17].
Healthcare professionals should play a supportive role that encourage mothers to breastfeeding without the prejudice which is very important and vital [18-21]. Therefore, postpartum primary care is also sensitive and critical and mothers should be encouraged to have EBF [22,23].
Noughabi (2014) and Ranjbaran (2016) reported the EBF was 46.5% in Tehran and 49.1 % in Iran respectively (6, 7). The several strong evidence showed the short and long-term benefits of breastfeeding for both baby and mother [6,7], also WHO has suggested governments by increasing the rate of breastfeeding, one-quarter of the mortality rate of heart disease, cancer, diabetes, asthma and respiratory diseases will be reduced by 2025 [5].
So, this study investigated the impacts of effective therapeutic communication between medical staff and mothers as well as its effects on the rate of breastfeeding and EBF.
Methods and Materials
This study was a clinical trial conducted for one year from July 2014 to August 2015. The study population based on the inclusion a criterion was comprised of all healthy nulliparous pregnant women aged at least 18 years with the ability to read and write. They also had decided to breastfeed and they were full-term pregnancy (>38 weeks of gestational age) with the healthy neonates. The systemic diseases during the pregnancy, postpartum psychosis, the existence of anomalies and diseases in newborns were the exclusion criteria. The samples included of 170 pregnant women for delivery which referred to the emergency department of Vali-e-Asr Hospital in Tehran.
The research purpose and the willingness to participate in the study were described, and the informed consent from mothers was obtained.
The samples were randomly divided into two groups of intervention (n=85) and control group (n=85). Based on randomized blocks with size 4; the first sample was assigned to group A, the second sample was included in group A, the third and the fourth samples were placed in group B, and such a random division continued in the following order until all 170 samples were divided. Healthcare therapists and staff as well as mothers were not aware of the groups assigned and they were only given specific codes which were entirely blind. (AABB, ABBA, ABAB, BBAA, BABA, BAAB ...)
The intervention in this study was in the form of therapeutic communication training to nurses in the delivery emergency department and gynecology ward on how to communicate with mothers.
10 nurses with the morning and night shifts of working were selected from the delivery emergency department.
The selection of nurses based on the bachelor’s degree, at least 5 years of work experience and willingness to participate in the study. Communication skills training was administered to nurses in three sessions (one hour per a session) of group training by a psychologist with an educational package. The training course and educational package consisted of four communication skills extracted out of ten life skills.
1. Empathy skills which refers to willingness to respond to emotional states of patients with the same ones. That is, a person is able to understand and respect patient-related problems even when they are not in those conditions. These skills make them like and pay attention to patients and have the same mutual feelings from patients. Through establishing better social relationships, both of them also become closer to each other.
2. Interpersonal skills i.e. ability that helps interactive relationships in which medical staff have the better collaboration and cooperation with patients and trust to them. They can recognize the borders of relationships with each other. Interpersonal relationship skills are likewise characterized as a process by which patients’ information and feelings are shared with medical staff.
3. Stress management skills can be learned by the individual stress identification and development of coping strategies to deal with each stressor.
4. Emotional management skills are the ones that enable an individual to diagnose excitements in themselves and in patients, know their effects on their behaviors, and demonstrate appropriate responses to different emotions.
In the intervention group, professional therapeutic communication was performed on mothers during the labor and postpartum by the nurses. The nurses trained to mothers and also answered the questions related to breastfeeding and other maternal cares. But in the control group, mothers received a routine communications in the delivery emergency room.
Skin contact immediately after delivery and postnatal rooming performed between mother and infant. All of samples stayed in hospital for 48 hours.
The mothers in both groups completed the demographic characteristics and patient satisfaction questionnaire. The patient satisfaction is a Researcher- structure questionnaire and included 16 items scored based on Likert-type scale (from 1 to 5). Its content was comprised of nurses’ behavior and their characteristics including patience, kindness, cooperation, responsiveness to patient, their availability, respect to patient privacy, skills and knowledge required for work. The higher score is the higher of satisfaction. The internal consistency of the questionnaire was 0.70 and 0.76 respectively. In addition, results revealed that the questionnaire had acceptable reliability and test-retest reliability coefficient was 95%.
Postnatal breastfeeding (breastfeeding within one hour after the birth), the newborn weight at the end of 6 months of age, Use of formula milk and patient satisfaction from the medical staff services are the main outcomes. A medically trained staff followed the breastfeeding duration and weight gain at 6-month-old babies by the phone call.
It should be noted that the present study was recorded in the Iranian Registry of Clinical Trials with the code number IRCT2014020510746N4. The SPSS (Version 20) software (SPSS, Inc., Chicago, Il, USA) was also used for data analysis. The data analyzed by using descriptive statistics (mean, standard deviation, frequency) by chi-square and T- test, ANOVA was used to compare the groups. The level of significance and the test power were estimated equal to 95% and 80%, respectively.
Sample size
The report of the Ministry of Health in the year of 2012 indicates the lactation nearly to 60% by the end of the 6th month [7]. Kronberg in 2007 stated that promoting self-esteem and establishing a good relationship with mother could bring Breastfeeding to 80% [10]. Using a sample size formula, comparisons of the relationships between the two groups with 95% confidence, 90% power, and the difference of 20% - about 110 samples is needed for review.
Z1-a/2=1.96
Z1-B=1.28
alfa=0.05
Beta=0.1
p1=0.60
p2=0.80
n=110
Results
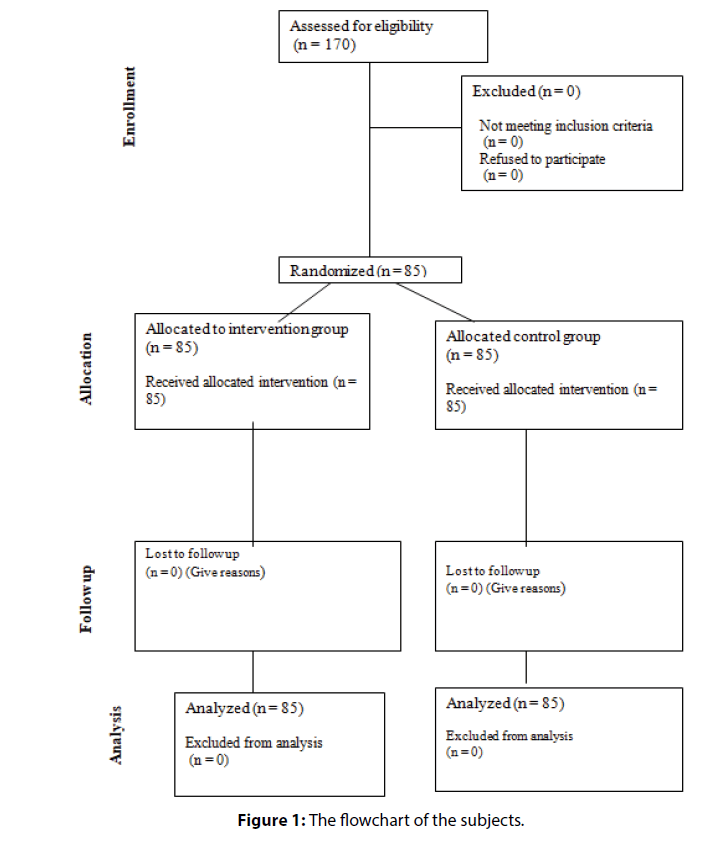
In the present study, both groups were similar in the demographic characteristics; in other words, the intervention and control groups were homogeneous (Figure 1).
In the intervention group, the newborn weight at the end of 6 months of age was much more than the Control group (8218.2308.57 ± 2308.57 g vs. 7442.23 ± 1923.27 g; P=0.018).
The mean of patient satisfaction score from the medical staff services was significantly higher in the intervention group (72.89 ± 4.64 vs. 50.01 ± 13.9; P=0.0003) (Table 1).
| Variables | Intervention group N (%) |
Control group N (%) | P |
|---|---|---|---|
| Maternal education | |||
| Below high school diploma | 32 (37.6%) | 33 (38.8%) | 0.381 |
| High school diploma | 32 (37.6%) | 21 (24.7%) | |
| Above high school diploma | 38 (44.7%) | 14 (16.5%) | |
| Paternal education | |||
| Below high school diploma | 41 (48.2%) | 47 (55.3%) | 0.49 |
| High school diploma | 29 (34.1%) | 28 (32.9%) | |
| Above high school diploma | 15 (17.6%) | 10 (11.8%) | |
| Maternal occupation | |||
| Housewife | 81 (95.3%) | 76 (89.4%) | 0.149 |
| Employed | 4 (4.7%) | 9 (10.6%) | |
| Type of delivery | |||
| Normal | 65 (76.5%) | 20 (23.5%) | |
| Caesarean section | 63 (74.1%) | 0.687 | |
Table 1: Clinic-pathology features of metastatic colon cancer patients whose disease was not radically resectable
EBF was significantly higher in the intervention group than the control group, (32 (37%) vs. 20 (23%), P=0.046).
Use of formula milk in the control group was higher than the intervention group (41 (48%) vs. 18 (21%); P=0.0001). Postnatal breastfeeding in the intervention group was significantly more than the control group (85(100%) vs. 62(73%) individuals; P=0.0001) (Table 2).
| Variables | Intervention group M ± SD |
Control group M ± SD |
P |
|---|---|---|---|
| Maternal age | 28.88 ± 5.04 | 28.85 ± 6.24 | 0.968 |
| Paternal age | 32.82 ± 5.35 | 33.46 ± 6.41 | 0.484 |
| Duration of marriage | 7.23 ± 5.37 | 7.42 ± 5.74 | 0.828 |
| Age of marriage | 21.59 ± 4.06 | 21.39 ± 4.45 | 0.76 |
| Age of delivery | 38.24 ± 1.72 | 38.15 ± 1.64 | 0.716 |
| Baby weight at birth | 307.76 ± 696.79 | 3080.41 ± 744.58 | 0.974 |
| Baby weight at 6 months of age | 8218.82 ± 2308.57 | 7442.23 ± 1923.27 | 0.018 |
| Patient Satisfaction | 72.79 ± 4.64 | 50.01 ± 13.9 | 0.0003 |
Table 2: Comparison of Quantitative variables of demographic characteristics in both intervention and control groups.
Data analysis also revealed that breastfeeding in the early hours of birth could multiply the breastfeeding continuation until the end of 6 months of age. In this respect, breastfeeding was started by 122 mothers within the first hours of birth which led to breastfeeding continuation by 110 (90%) individuals until the end of 6 months of age. However; in 48 mothers with no breastfeeding within the first hours of birth, 72% breastfeeding continuation for 6 months was observed (P=0.001).
At six months infants in the study group grew more those in the control group (8218.82 ± 2308.57 vs. 7442.23 ± 1923.27 gr, p=0.018).
Discussion
The purpose of this study was to teach the techniques of communication skills to medical staff in order to enhance and provide better healthcare services to mothers, which are leading to an increase the rate of EBF in the first 6 months of birth. The results of the present study showed that effective and high-quality therapeutic communications by medical staff in the intervention group could significantly increase EBF in the first 6 months of age compared to control group. Besides, the use of formula milk in the intervention group was lower than the control group. However, the rate of breastfeeding in the intervention group by the end of 6 months showed a significant rise than the control group.
In a systematic review on encouraging breastfeeding, (968 abstracts and 268 studies in which 53 cases were clinical trials) were evaluated the EBF at 4-6 weeks and 6 months after delivery. The reports showed 137% increase (more than 6 times) in EBF in developing countries compared to 1.3 times rise in the studies conducted in developed countries. The results demonstrated that prenatal counseling had a significant effect on the results of breastfeeding at 4-6 weeks and at 6 months [24].
Li (2014) in a study assessed staff training as well as policies of organizational structure associated with breastfeeding of newborns 24 to 48 hours after delivery. The results showed that hospital staff training could further the rate of breastfeeding in infants in terms of improving knowledge, attitudes, and skills related to breastfeeding [25]. Fox (2015) in their qualitative study on the experiences of nursing mothers through baby cafe service and breastfeeding support reported that readiness for breastfeeding was required to be established before childbirth and breastfeeding support with the centrality of parents needed to be provided immediately after delivery. These findings suggested that effective social support along with reassurance and guidance by the experienced staff could help women overcome difficulties and increase their self-esteem in order to achieve nutritional goals [26]. A specific model of midwifery care and dialogues with mothers within the first week of delivery could facilitate mother-infant relationships in terms of breastfeeding [27,28]. In addition, Grochans reported that professional support to nulliparous mothers and pregnant women with no breastfeeding training should be provided by midwives and nurses which could lead to a better preparation of mothers to breastfeed. Midwives and nurses were also required to utilize their professional skills in order to improve and enhance the quality of maternal care [29]. It also seems that obtaining information as well as providing practical and emotional support by nurses can reduce potential problems of breastfeeding [30]. According to the results of the studies [25-30], it was concluded that all their results were consistent with the findings of the present study.
| Variables | Intervention group | Control group | P |
|---|---|---|---|
| Breastfeeding | M ± SD | M ± SD | |
| Immediate breastfeeding after birth | 85 (100%) | 62 (72.9%) | 0.0001 |
| Exclusive breastfeeding for 6 months | 32 (37.5%) | 20 (23.5%) | 0.046 |
| Breastfeeding up to 6 months | 79 (92.9%) | 66 (77.6%) | 0.005 |
| Use of formula milk up to 6 months | 18 (21.2%) | 41 (48.2%) | 0.001 |
| Breastfeeding along with other liquids | 19 (22.4%) | 23 (27.1%) | 0.477 |
| Less than a bottle of formula milk a day | 15 (17.6%) | 23 (27.1%) | 0.141 |
| At least one bottle of formula milk a day | 13 (15.3%) | 15 (17.6%) | 0.679 |
| Partial breastfeeding | 13 (15.3%) | 19 (22.4%) | 0.239 |
| Use of breast milk in a bottle | 14 (16.5%) | 29 (34.1%) | 0.008 |
Table 3: Comparison of outcomes in both intervention and control groups.
Based on the systematic review conducted by Swerts in 2016, attention to mother-infant relationships immediately after birth was very important and it could have significant effects on EBF [30]. In the present study, not only training courses in terms of communication skills and techniques were provided for medical staff but also educational packages as well as psychological and support counseling were given to mothers which in some way focused on mother-infant relationships and led to an increase in breastfeeding and EBF and reduction in the use of formula milk by mothers.
The results of this study also showed that mothers who breastfed their babies immediately after birth, it leads to continuation of lactation until the first 6 months of the baby's birth. The onset delay in the baby's lactation increases the use of formula milk. These problems are more likely to be observed in nulliparous and employed mothers. Thus, they should be provided with the more maternal care before childbirth [31]. It seems that early breastfeeding especially within the first hours of birth should be considered by medical staff as well as mothers since that is the golden time for continuation and duration of breastfeeding. To achieve the desired results in terms of breastfeeding, it seems that Professional and specialized courses that promote better communication between medical staff with the breastfeeding mothers, and also breastfeeding support should be considered. It is essential to establish professional courses to provide knowledge and evidence-based performance to support breastfeeding mothers and their infants.
Conclusion
The professional therapeutic relationship of the medical staff with the mothers led to an increase in exclusive breastfeeding and continuation of breastfeeding in the first 6 months of childbirth and reduced the use of formula milk.
At six months old, the babies in the study group grew more than the baby of the control group. So; it seems that breastfeeding is associated with higher baby growth and lower use of formula feeding.
Acknowledgments
We hereby express our gratitude to the Office of the Vice-Chancellor for Research in Tehran University of Medical Sciences for their financial support and scientific-ethical approval of this study (code no. 22835). We also appreciate all the staff in Vali-e-Asr hospital especially Ms. Khadijeh Goudarzi for their cooperation in the implementation of this study.
References
- Schanler SJ, Dooley S. Breastfeeding handbook for physicians. Washington: American College of Obstetricians and Gynecology (2006).
- Akhlaghi F, Ebrahimzadeh S, Baghani R, Azhari S, Salehi Federdi J. Comparing the effects of hands-on and hand-off breastfeeding methods on self-efficacy in primiparous mothers. JSUMS 17: 248-255 (2011).
- World Health Organization Part 1: Definitions; Indicators for assessing infant and young child feeding practices: conclusions of a consensus meeting held; 6-8 November 2007; Washington, DC, USA. Geneva: (2008).
- Alikassifoglu M. Factors influencing the duration of exclusive breastfeeding in a group of Turkish women. J Hum Lact 17: 220-226 (2001).
- http://www.who.int/maternal_child_adolescent/topics/newborn/nutrition/breastfeeding/en/
- Noughabi ZS, Tehrani SG, Foroushani AR, Nayeri F, Baheiraei A. Prevalence and factors associated with exclusive breastfeeding at 6 months of life in Tehran: a population-based study. East Mediterr Health J 20:24-32 (2014).
- Ranjbaran M, Nakhaei MR, Chizary M, Shamsi M. Prevalence of exclusive breastfeeding in Iran: Systematic review and meta-analysis. Int J Epidemiol Res 3: 294-301 (2016).
- Thulier D , Mercer J. Variables Associated With Breastfeeding Duration. AWHONN. 2009: 259-268 (2009).
- Britton C, McCormick FM, Renfrew MJ, Wade A, King SE. Support for breastfeeding mothers. Cochrane Database Syst Rev 24:CD001141 (2007).
- Kronborg H, Vaeth M, Olsen J, Iversen L, Harder I. Effect of early postnatal breastfeeding support: a cluster-randomized community based trial. Acta Paediatr 96: 1064-1070 (2007).
- Freed GL, Clark SJ, Lohr JA, Sorenson JR. Pediatrician involvement in breast-feeding promotion: a national study of residents and practitioners. Pediatrics. 96 :490-494 (1995).
- Hellings P, Howe C. Assessment of breastfeeding knowledge of nurse practitioners and nurse-midwives. J Midwifery Womens Health 45: 264-270 (2000).
- Hellings P, Howe C. Breastfeeding knowledge and practice of pediatric nurse practitioners. J Pediatr Health Care. 18:8-14 (2004).
- Fenwick J, Barclay L, Schmied V. ‘Chatting’: an important clinical tool in facilitating mothering in neonatal nurseries. J Adv Nurs. 33: 583-593 (2001).
- Frei IA, Mander R. The relationship between first-time mothers and care providers in the early postnatal phase: an ethnographic study in a Swiss postnatal unit. Midwifery 27: 716-722 (2011).
- Hauck YL, Fenwick J, Dhaliwal SS, Butt J, Schmied V. The association betweenwomen's perceptions of professional support and problems experienced on breastfeeding cessation: a Western Australian study. J Hum Lact 27: 49-57(2011).
- Wilkins C. A qualitative study exploring the support needs of first time mothers on their journey towards intuitive parenting. Midwifery 22: 169-180 (2006).
- Backström CA, Wahn EH, Ekström AC. Two sides of breastfeeding support: experiences of women and nurses. Int Breastfeed J 5: 1-8 (2010).
- Kuan LW, Britto M, Decolongon J, Schoettker PJ, Atherton HD, Kotagal UR. Health system factors contributing to breastfeeding success. Pediatrics 104:e28 (1999).
- Hegney D, Fallon T, O’Brien ML. A retrospective case controlled study of women who experienced extraordinary breastfeeding problems. J Clin Nurs 17: 1182-1192.
- Graffy J, Taylor J. what information, advice and support do women want with breastfeeding? Birth. 2005; 32: 179-186.
- Geçkil ES¸ ahin T, Ege E. Traditional postpartum practices of women and infants and the factors influencing such practices in South Eastern Turkey. Midwifery 25: 62-71 (2009).
- Kim SK, Park S, Oh J, Kim J, Ahn S. Interventions promoting exclusive breastfeeding up to six months after birth: A systematic review and meta-analysis of randomized controlled trials. Int J Nurs Stud 80:94-105 (2018).
- Imdad A, Yakoob MY, Bhutta ZA. Effect of breastfeeding promotion interventions on breastfeeding rates, with special focus on developing countries. BMC Public Health 11: S24 (2011).
- Li CM, Li R, Ashley CG, Smiley JM, Cohen JH, Dee DL. Associations of hospital staff training and policies with early breastfeeding practices. J Hum Lact 30:88-96 (2014).
- Fox R, McMullen S, Newburn M. UK women's experiences of breastfeeding and additional breastfeeding support: a qualitative study of Baby Café services. BMC Pregnancy Childbirth. 7:147 (2015).
- Swerts M, Westhof E, Bogaerts A, Lemiengre J. Supporting breast-feeding women from the perspective of the midwife: A systematic review of the literature. Midwifery 37:32-40 (2016).
- Burns E, Fenwick J, Sheehan A, Schmied V. Mining for liquid gold: midwifery language and practices associated with early breastfeeding support. Matern Child Nutr 9:57-73 (2013).
- Grochans E, Jurczak A, Augustyniuk K, Szych Z, Trypka I. Comparative analysis of informative support in lactation in lying-in women hospitalized in rooming-in system. Adv Med Sci 52:68-72 (2007).
- Demirtas B. Breastfeeding support received by Turkish first-time mothersi.nr. 33. Int Nurs Rev 59:338-344 (2012).
- Masood S, Mahmood-ur-Rahman, Mahmood H, Faisal T, Maroof S, Qureshi AM. Observance of who ten steps towards successful breastfeeding; a survey from postpartum mothers. J Ayub Med Coll Abbottabad 28:84-88 (2016).