Mini Review - Interventional Cardiology (2025) Volume 17, Issue 3
The DELIVER Technique: A Comprehensive Review of Deep Catheter Engagement for Rotational Atherectomy in Complex Coronary Anatomy
- Corresponding Author:
- Umihiko Kaneko
Umihiko Kaneko, Department of Cardiovascular Medicine, Sapporo Cardio Vascular Clinic, Sapporo Heart Center, North 49, East 16, 8-1, Higashi Ward, Sapporo, Japan
E-mail: uk434471@gmail.com
Received date: 02-Jun-2025, Manuscript No. FMIC-25-166240; Editor assigned: 04-Jun-2025, PreQC No. FMIC-25-166240 (PQ); Reviewed date: 18-Jun-2025, QC No. FMIC-25-166240; Revised date: 25-Jun-2025, Manuscript No. FMIC-25-166240 (R); Published date: 02-Jul-2025, ![]()
Abstract
Rotational Atherectomy (RA) is an essential technique for managing severely calcified coronary artery disease during percutaneous coronary intervention. However, burr delivery can be significantly hindered in patients with complex anatomy, such as proximal vessel tortuosity, previously implanted stents, transcatheter aortic valves, or anomalous coronary origins. These anatomical limitations elevate the risk of procedural failure and severe complications, including burr entrapment, burr fracture, coronary artery perforation, and dissection. The DELIVER technique— Deep Engagement of guide catheter or chiLd-guIde catheter for burr deliVEry and Rotational atherectomy—was developed to overcome these challenges through strategic deep catheter positioning using dedicated advancement techniques. This mini-review provides an in-depth exploration of the DELIVER technique, including clinical rationale, procedural steps, device selection, anatomical considerations, safety strategies, and comparative performance with other calcium modification methods. Recent evidence and procedural experience suggest that the DELIVER technique offers an effective and versatile solution for improving procedural success in RA for anatomically complex cases.
Keywords
Calcified lesion . Child guide catheter . Complex coronary anatomy . Deep engagement . DELIVER technique . Guiding catheter . Rotational atherectomy
Introduction
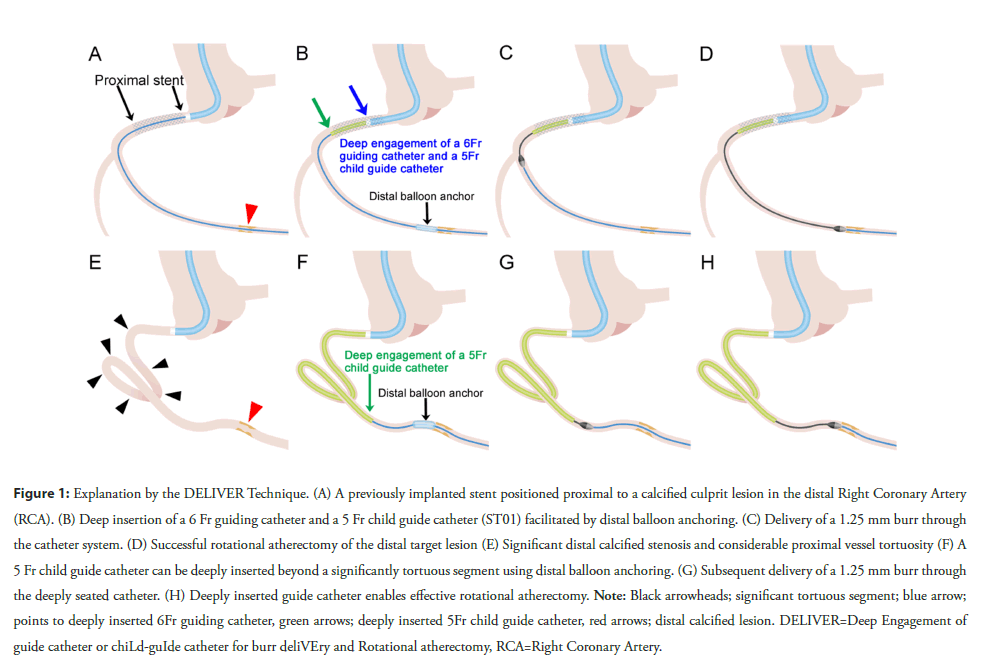
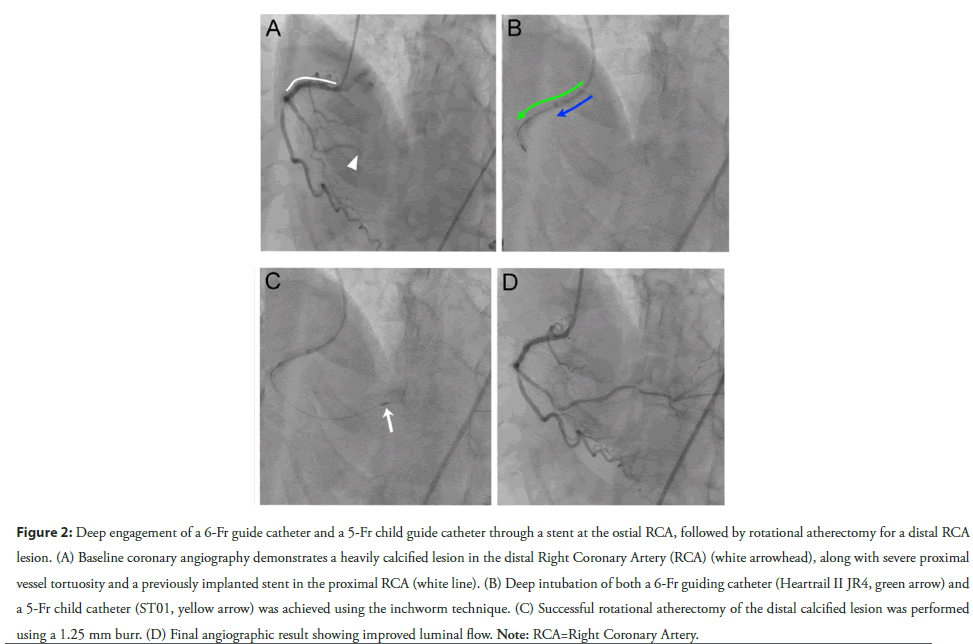
Rotational Atherectomy (RA) using the RotablatorTM system (Boston Scientific) is a well-established technique for plaque modification during Percutaneous Coronary Intervention (PCI) in heavily calcified lesions [1-5]. While burr advancement from the guiding catheter to the lesion is generally uncomplicated in straightforward proximal lesions, complex anatomical features—such as proximal vessel tortuosity, previously implanted stents, Transcatheter Aortic Valves (TAVs), or anomalous coronary origins— can severely hinder burr delivery. These challenges significantly increase the risk of serious complications including burr entrapment, fracture, coronary perforation, and vessel dissection [6-9]. To address such limitations, adjunctive techniques like larger French guiding catheters, support wires, and Guide Extension Catheters (GECs) have been proposed [10]. Nevertheless, burr delivery failure remains a major hurdle. The DELIVER technique—Deep Engagement of guide catheter or chiLd-guIde catheter for burr deliVEry and Rotational atherectomy—aims to overcome these anatomical barriers by combining deep catheter engagement with controlled advancement strategies (Figures 1 and 2). This review describes the procedural elements, clinical indications, practical considerations, and comparative advantages of the DELIVER technique in the setting of complex coronary anatomy [11].
Figure 1: Explanation by the DELIVER Technique. (A) A previously implanted stent positioned proximal to a calcified culprit lesion in the distal Right Coronary Artery (RCA). (B) Deep insertion of a 6 Fr guiding catheter and a 5 Fr child guide catheter (ST01) facilitated by distal balloon anchoring. (C) Delivery of a 1.25 mm burr through the catheter system. (D) Successful rotational atherectomy of the distal target lesion (E) Significant distal calcified stenosis and considerable proximal vessel tortuosity (F) A 5 Fr child guide catheter can be deeply inserted beyond a significantly tortuous segment using distal balloon anchoring. (G) Subsequent delivery of a 1.25 mm burr through the deeply seated catheter. (H) Deeply inserted guide catheter enables effective rotational atherectomy. Note: Black arrowheads; significant tortuous segment; blue arrow; points to deeply inserted 6Fr guiding catheter, green arrows; deeply inserted 5Fr child guide catheter, red arrows; distal calcified lesion. DELIVER=Deep Engagement of guide catheter or chiLd-guIde catheter for burr deliVEry and Rotational atherectomy, RCA=Right Coronary Artery.
Figure 2: Deep engagement of a 6-Fr guide catheter and a 5-Fr child guide catheter through a stent at the ostial RCA, followed by rotational atherectomy for a distal RCA lesion. (A) Baseline coronary angiography demonstrates a heavily calcified lesion in the distal Right Coronary Artery (RCA) (white arrowhead), along with severe proximal vessel tortuosity and a previously implanted stent in the proximal RCA (white line). (B) Deep intubation of both a 6-Fr guiding catheter (Heartrail II JR4, green arrow) and a 5-Fr child catheter (ST01, yellow arrow) was achieved using the inchworm technique. (C) Successful rotational atherectomy of the distal calcified lesion was performed using a 1.25 mm burr. (D) Final angiographic result showing improved luminal flow. Note: RCA=Right Coronary Artery.
Rationale and clinical indications
The DELIVER technique enables RA burr advancement in anatomically complex vessels by bypassing mechanical obstacles in the proximal coronary artery. It involves advancing either a standard Guiding Catheter (GC) or a 5-Fr child guide catheter (5CG; Heartrail ST01, Terumo, Japan) beyond anatomical impediments using dedicated advancement techniques. Once properly positioned, the catheter offers a stable, coaxial pathway for burr delivery, reducing the risk of vessel trauma and improving procedural success. The technique is particularly useful in the following situations:
• Proximal vessel tortuosity that impedes burr advancement or increases the risk of vessel injury
• Previously implanted stents that obstruct device passage
• TAVs that reduce catheter backup support and hinder proper guiding catheter engagement
• Anomalous coronary origins that result in poor coaxial alignment
By achieving engagement distal to these obstructions, the catheter ensures smoother burr passage and enhances overall procedural stability.
Step-by-Step procedural description of the DELIVER technique:
The DELIVER technique consists of five key steps.
Step 1: Catheter advancement strategy
Three dedicated strategies help navigate the catheter beyond anatomical barriers [12]:
• Distal balloon anchoring: A balloon is inflated distally, and slight traction is applied to guide the catheter forward. This technique is useful when deep intubation is limited by tortuosity or stent interference [13].
• Balloon-Assisted Tracking (BAT): A small balloon (1.5-2.0 mm) is inflated just ahead of the catheter, then partially pulled back while deflating, allowing the catheter to follow. BAT is effective in rossing stented or narrowed segments [14,15].
• Inchworm technique: Repetitive inflation/deflation of a balloon at the catheter tip facilitates incremental advancement. This method facilitates passage through previously implanted stents or TAVs.
These strategies can be used individually or in combination, depending on the specific anatomical challenge.
Step 2: Deep engagement of the catheter
Once the catheter has reached the area beyond the obstruction, it should be gently advanced to achieve stable and coaxial engagement with the distal vessel. Excessive force must be avoided to reduce the risk of vessel trauma.
Step 3: Guidewire exchange
The initial workhorse wire is exchanged for a ROTAWIRETM (Boston Scientific, USA), via a microcatheter or over-the-wire balloon. Care must be taken to ensure that the wire does not become kinked or looped during the exchange.
Step 4: Burr delivery in DynaGlideTM mode
The RA burr is then advanced through the catheter using DynaGlidTM mode to reduce friction and minimize the risk of wire dislodgement. If resistance is encountered during burr advancement, it is important to confirm that the catheter and guidewire remain properly aligned and are not kinked or deformed.
Step 5: Rotational atherectomy execution
The deeply engaged system provides robust support for effective atherectomy of distal lesions.
Catheter selection strategies
Three catheter types are used in the DELIVER technique:
1. Standard Guiding Catheters (GCs): Available in 6-8 Fr sizes, GCs offer strong backup and accommodate larger burrs (up to 2.25 mm in 8-Fr systems). GCs are preferred in cases involving large-caliber proximal vessels or when using femoral access. A soft- tip catheter with relatively gentle curves is generally recommended, such as the HeartrailTM (Terumo). Common shapes include Judkins Right (JR), Judkins Left (JL), Ikari Right (IR), and Ikari Left (IL), selected according to coronary anatomy. Use of GCs simplifies the procedure by eliminating the need for additional delivery systems such as 5CGs or GECs in many cases.
2. 5-Fr Child Guide Catheter (5CG): The 5CG (Heartrail ST01) is a 120-cm, straight, over-the-wire catheter equipped with a soft, atraumatic 13-cm tip that enables deep coronary engagement while minimizing vessel injury and myocardial ischemia. Its smooth inner lumen (inner diameter: 1.50 mm) permits reliable delivery of both 1.25 mm and 1.5 mm burrs.
3. Guide-Extension Catheter (GEC): Recently, the use of a GEC for RA—by deeply advancing the GEC and delivering the burr through it—has been reported as a promising approach [10,16,17]. Among currently available GECs, the 6-Fr GUIDEZILLATM (Boston Scientific, USA) is the only model compatible with a 1.25 mm burr, while all 7-Fr GECs can accommodate both 1.25 mm and 1.5 mm burrs [18]. However, GEC entry ports often obstruct burr passage, and even with successful engagement, burr delivery frequently fails, thereby limiting its reproducibility. While preloading the burr into the GEC outside the body and advancing both together may facilitate delivery in certain cases, this approach carries a substantial risk of proximal vessel injury or delivery failure, particularly given that the GEC needs to be inserted without an established catheter advancement technique. In contrast, the DELIVER technique allows for smoother and more consistent burr delivery, owing to the uniform, step-off-free inner lumen of the deeply engaged GC or 5CG.
Key considerations and risk management
Although the DELIVER technique improves burr deliverability and enhances procedural success in complex RA, deep catheter engagement introduces specific risks that must be proactively managed.
1. Loss of wire position: Friction within narrow-lumen catheters, such as the 5CG, may result in unintentional withdrawal of the ROTAWIRETM. To mitigate this risk, it is essential to activate DynaGlideTM mode during burr advancement and to avoid bending or kinking of the catheter or guidewire, both before and during the procedure.
2. Coronary ischemia and hemodynamic instability: Deep catheter engagement may compromise antegrade coronary flow, particularly in small, tortuous, or diffusely diseased vessels, leading to myocardial ischemia and hemodynamic instability. If signs of ischemia are detected, the catheter should be retracted slightly to restore perfusion. In high-risk patients, hemodynamic support devices may be considered.
3. Dissection: Non-coaxial catheter positioning or the application of excessive forward force may injure the vessel wall, resulting in dissection. The use of 5CG, or soft-tip GCs with relatively gentle curves—such as JR, JL, IR, or IL—combined with three catheter advancement techniques, reduces the need for excessive manual force and promotes smoother device delivery.
4. Stent deformation: Pre-existing stents in proximal segments are susceptible to deformation, especially when the catheter is advanced forcefully or without proper coaxial alignment. Intravascular imaging—using intravascular ultrasound or optical coherence tomography—should be performed prior to deep catheter engagement to assess stent expansion and apposition, and to confirm that the guidewire remains within the stent lumen. During catheter advancement, techniques such as BAT or the inchworm method are recommended to preserve coaxiality and reduce mechanical interaction with the stent.
5. Stability of a deeply engaged catheter: Careful attention should be paid to the positioning and stability of the deeply engaged catheter, the GC ("mother" GC), and the ROTAWIRETM throughout the RA procedure. Accidental withdrawal of a deeply engaged catheter can make re-engagement extremely challenging without the aid of the previously described catheter advancement techniques. To minimize this risk, careful burr manipulation, selection of smaller burr sizes, use of extra support wires, and higher rotational speeds are recommended.
Comparison with other calcium modification techniques
The Diamondback 360° Coronary Orbital Atherectomy (OA) System (Cardiovascular System) is now widely used for the treatment of calcified lesions. The efficacy of GEC-assisted OA has been reported for treating a tortuous and heavily calcified distal lesion [19]. However, the OA system often encounters resistance at the entry port of the GEC, resulting in delivery failure—a significant limitation similarly observed with GEC-assisted RA. In such cases, deep engagement of a 5CG or GC, as utilized in the DELIVER technique, may provide a more dependable strategy for successful OA delivery [20].
Intravascular Lithotripsy (IVL) with the Shockwave C2 catheter (Shockwave Medical, Fremont, California) offers a distinct advantage over RA or OA by enabling the disruption of both superficial and deep calcium. This is achieved with a low risk of slow or no reflow and coronary perforation, irrespective of guidewire bias. Nevertheless, the relatively bulky profile of the IVL balloon (tip profile: 0.58 mm; crossing profile: 1.07 mm) frequently restricts its deliverability to distal lesions, even with GEC support. For these challenging scenarios, RA, especially when employing the DELIVER technique, can effectively modify the lesion and enhance subsequent IVL balloon delivery (Table 1) [21].
| Rotational atherectomy | Orbital atherectomy | Intravascular lithotripsy | |
|---|---|---|---|
| Device | Rotablator with ROTAPRO™ system (Boston Scientific, Natick, MA) | Diamondback 360 (Cardiovascular Systems Inc. St. Paul, MN) | Shockwave C2 (Shockwave Medical, Fremont, CA) |
| Guide catheter system | ≥ 6-Fr | ≥ 6-Fr | ≥ 6-Fr |
| Guide catheter compatibility | 5CG: ≤ 1.5 mm burr | ≥ 6-Fr GC or 5CG: Available | ≥ 6-Fr GC or 5CG: Available in full spec |
| 6-Fr GC: ≤ 1.75 mm burr | |||
| 7-Fr GC: ≤ 2.0 mm burr | |||
| 8-Fr GC: ≤ 2.25 mm burr | |||
| Guide extension catheter compatibility | 6-Fr GEC: Only 1.25 mm burr compatible; crpssomg often unsuccessful (limited to certain products). 7-Fr GEC: ≤ 1.5 mm burr compatible |
≥ 6-Fr GEC: Compatible, but crossing often unsuccessful | ≥ 6-Fr GEC: Available in full spec |
| Reproducibility of device passage within the GEC | Very low | Very low | High |
| Device delivery through the catheter | Slightly resistant | Easy | Resistant |
| Guidewire | ROTAWIRE™ Drive: Slightly difficult to manipulate | ViperWire: Slightly difficult to manipulate | 0.014″ conventional guidewire of choice |
| Direction of ablation | Forward only | Bidirectional (Forward and backward) | No plaque ablation |
| Effect of ablation | Very strong | Moderate | None (no plaque ablation) |
| Factors affecting ablation effect | Guidewire bias, minimal lumen area, rotational speed, and burr size | Guidewire bias, minimal lumen area, and rotational speed | No plaque ablation |
| Prediction of ablation effect | Intentional and directional ablation can be achieved in case of favorable guidewire bias for the calcified lesion | Sometimes unintentional or unpredictable, irrespective of guidewire bias | Not directly feasible; however, circumferential calcium modification may still be achieved |
| Impact of guidewire bias on calcium modification | Mainly dependent on guidewire bias | Moderately dependent on guidewire bias; however, sometimes unintentional or unpredictable | Circumferential calcium modification, independent of guidewire bias |
| Impact on superficial and deep calcium | Ablates superficial calcium only | Ablates superficial calcium only | Modifies superficial and possibly, deep calcium |
| Coronary perforation | 0.5%–2.0% | 0.7%–1.8% | <1% |
| Note: 5CG: 5-Fr Child-Guide catheter; GC: Guide Catheter; GEC: Guide Extension Catheter | |||
Table 1: Comparison of rotational atherectomy, orbital atherectomy, and intravascular lithotripsy assisted by guiding catheters, 5-Fr child catheters, or guide extension catheters in the treatment of distal calcified coronary lesions.
Conclusion
The DELIVER technique offers a practical and effective approach to overcoming anatomical challenges during RA. By combining deep catheter engagement with controlled and reproducible advancement strategies, it facilitates consistent burr delivery while minimizing the risk of proximal vessel injury.
Limitations
The DELIVER technique may not be feasible in very small, extremely angulated, or severely calcified segments where deep catheter engagement carries excessive risk. In such cases, alternative strategies or hybrid approaches should be considered. Furthermore, structured training, including simulation-based education or proctoring, is crucial for operators learning this method. This review is based on procedural experience and selected case applications; therefore, further prospective studies are warranted to validate its safety, reproducibility, and long-term outcomes.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
Umihiko Kaneko, Yoshifumi Kashima and Shoichi Kuramitsu have served as a proctor for Rotablator for Boston Scientific. The other authors have no conflicts of interest to declare.
References
- Ayoub M, Tajti P, Ferenc M, et al. Feasibility and outcome of the Rotapro system in treating severely calcified coronary lesions: The Rotapro study. Cardiol J. 30(4):526-533 (2023).
[CrossRef] [Google Scholar] [PubMed]
- Mankerious N, Richardt G, Allali A, et al. Lower revascularization rates after high-speed rotational atherectomy compared to modified balloons in calcified coronary lesions: 5-year outcomes of the randomized PREPARE-CALC trial. Clin Res Cardiol. 113(7):1051-1059 (2024).
[CrossRef] [Google Scholar] [PubMed]
- Sakakura K, Ito Y, Shibata Y, et al. Clinical expert consensus document on rotational atherectomy from the Japanese association of cardiovascular intervention and therapeutics: Update 2023. Cardiovasc Interv Ther. 38(2):141-162 (2023).
[CrossRef] [Google Scholar] [PubMed]
- Sharma SK, Tomey MI, Teirstein PS, et al. North American expert review of rotational atherectomy. Circ Cardiovasc Interv. 12(5):e007448 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Iannopollo G, Gallo F, Mangieri A, et al. Tips and tricks for rotational atherectomy. J Invasive Cardiol. 31(12):E376-E383 (2019).
[Google Scholar] [PubMed]
- Kaneko U, Kashima Y, Sugie T, et al. Rotablator driveshaft fracture due to significant proximal tortuosity and enlargement causing massive coronary perforation. Korean Circ J. 50:1048-1050 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Kaneko U, Kashima Y, Sugie T, et al. Fracture of rotational atherectomy burr: Preâfracture signs, mechanisms, and management strategies. Catheter Cardiovasc Interv. 105(7):1608-1615 (2025).
[CrossRef] [Google Scholar] [PubMed]
- Tomasiewicz B, Kubler P, Zimoch W, et al. Acute angulation and sequential lesion increase the risk of rotational atherectomy failure. Circ J. 85(6):867-76 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Morita Y, Kashima Y, Yasuda Y, et al. Burr entrapment in a percutaneous coronary intervention during rotational atherectomy: An experience with 3195 cases. J Invasive Cardiol. 35(10): (2023).
[Google Scholar] [PubMed]
- Derbas LA, Iskandar MH, Kavinsky LJ, et al. Utility of guide extension catheter for rotational atherectomy through a LIMA graft. JACC Cardiovasc Interv. 15(1):e1-e2 (2022).
[CrossRef] [Google Scholar] [PubMed]
- Kaneko U, Kashima Y, Kuramitsu S, et al. The DELIVER Technique: Deep engagement of guide or ChiLd-guIde Catheter for Burr DeliVEry and rotational atherectomy. JACC Case Rep. 30(5):103177 (2025).
[CrossRef] [Google Scholar] [PubMed]
- Garbo R, Iannaccone M, Werner GS, et al. Utility of guiding catheter extensions for recanalization of chronic total occlusions: A EuroCTO club expert panel report. JACC Cardiovasc Interv. 16(15):1833-1844 (2023).
[CrossRef] [Google Scholar] [PubMed]
- Ali M, Yagoub H, Ibrahim A, et al. Anchor-balloon technique to facilitate stent delivery via the GuideLiner catheter in percutaneous coronary intervention. Future Cardiol. 14(4):291-299 (2018).
[CrossRef] [Google Scholar] [PubMed]
- Patel T, Shah S, Pancholy S, et al. Balloonâassisted tracking: A mustâknow technique to overcome difficult anatomy during transradial approach. Catheter Cardiovasc Interv. 83(2):211-220 (2014).
[CrossRef] [Google Scholar] [PubMed]
- Elbarouni B, Moussa M, Kass M, et al. GuideLiner Balloon Assisted Tracking (GBAT): A new addition to the interventional toolbox. Case Rep Cardiol. 2016(1):6715630 (2016).
[CrossRef] [Google Scholar] [PubMed]
- Kato T, Fujino M, Takagi K, et al. The rotational atherectomy with a guide extension catheter for calcified and tortuous lesions in left anterior descending artery: A case report. BMC Cardiovasc Disord. 21:1-4 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Costanzo P, Aznaouridis K, Hoye A, et al. GuideLiner-facilitated rotational atherectomy in calcified right coronary artery: the "child" makes the difference. JACC Cardiovasc Interv. 9:e47-e48 (2016).
- PawÅowski T, Modzelewski P, Stachura M, et al. Guiding catheter extension compatibility for high speed rotational atherectomy. Postepy Kardiol Interwencyjnej. 17(2):210-213 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Kobayashi N, Yamawaki M, Hirano K, et al. Use of the orbital atherectomy system backed up with the guide-extension catheter for a severely tortuous calcified coronary lesion. SAGE Open Med Case Rep. 8:2050313X20921081 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Kawamura Y, Yoshimachi F, Murotani N, et al. Coronary orbital atherectomy using a five-French guiding catheter. Cardiovasc Interv Ther. 37(3):498-505. (2022).
[CrossRef] [Google Scholar] [PubMed]
- Nakamura M, Kuriyama N, Tanaka Y, et al. Dual-Prep registry: Atherectomy devices and intravascUlAr lithotripsy for the PREParation of heavily calcified coronary lesions registry. Cardiovasc Interv Ther. 40(3):553-564 (2025).
[CrossRef] [Google Scholar] [PubMed]