Case Report - Clinical Practice (2023) Volume 20, Issue 4
Sling surgery for pelvic organ prolapse in low setting resources: A case series
- Corresponding Author:
- Uzma Kausar
Department of Obstetrics and Gynecology, Government Medical College, Ambedkar Nagar, UP, India
E-mail: kong2@uk.ac.in
Received: March 09, 2023, Manuscript No. FMCP-23-91145; Editor assigned: March 14, 2023, PreQC No. FMCP-23-91145 (PQ); Reviewed: March 29, 2023, QC No. FMCP-23-91145; Revised: May 10, 2023, Manuscript No. FMCP-23-91145 (R); Published: May 18, 2023, DOI: 10.37532/ 2044-9038.2023.20(4).1-6
Abstract
Background: India has the largest prevalence of nulliparous prolapse and it is no surprise that Indian gynecologists have devised most of the conservative operations for genital prolapse. It is important to look at certain important aspects of the supporting sling Virkrud 14 classification of sling operations. This study was undertaken to assess the procedures of modified abdominal sling itself and its results.
Material and methods: Modified abdominal sling operation for conservative surgery for uterocervical descent is performed in twenty women of M.R.A. medical college Ambedkar nagar. The procedure is difficult and bold but is the perfect anatomical solution to strengthen weak uterosacral ligaments with the help of a mercelene. We have performed 25 cases of modified abdominal sling surgeries in obstetrics and gynaecology department from 2015 to 2022 of MRA medical college, Ambedkar nagar, India. Of these, 1 (04%) patient were nulligravida, 7 (35%) were primipara and 12 (48%) were multigravida. Four (16%) women had associated infertility. Additional surgeries like tubectomy were performed in 2 (08%) women, ovarian drilling in 4 (16%) and myomectomy in 1 (12.2%).
Results: All 25 patients were analyzed for intraoperative and postoperative complications. All were followed up for mean duration of 12 months. Out of 4 infertile women, 2 conceived spontaneously 6 months after the surgery and 6 primipara were conceived spontaneously within a year. There was no recurrence of prolapse.
Conclusions: Nulliparous prolapse can be treated by various surgical procedures, each having their own merits and de merits. Modified abdominal sling is the real corrective solution to weekend uterosacral ligaments. It is the perfect anatomical solution for conservatives’ approach to uterocervical descent.
Keywords
POP (Pelvic Organ Prolapse), Nulligravida, Multiparity, Infertility Proline mesh, Mercelene tape
Introduction
Prolapse is loosely defined in medical terms as the slipping forward or down of an anatomical structure in relation to its normal position. In the specific case of POP, it is defined by the International Urogynecological Association (IUGA) in the terminology guidance as “the descent of one or more of the anterior vaginal walls, posterior vaginal wall, the uterus (cervix) or the apex of the vagina (vaginal vault or cuff scar after hysterectomy)” [1]. Pelvic Organ Prolapse (POP) is a highly prevalent condition reported to affect 40% of women over the age of 42 [2]. The term refers to the downward displacement of the pelvic organs, namely the uterus, bladder, and/or bowels into the vagina [3]. Uterine prolapse specifically is reportedly found in over 14% of postmenopausal women on clinical examination [4]. Following failed conservative measures such as Pelvic Muscle Floor Therapy (PFMT) and the use of vaginal pessaries, some women will undergo surgery for which there is a reported lifetime risk of between 11% and 19% [5].
In India, nulliparous prolapse cases constitute 1.5%–2% of genital prolapses; the incidence is even higher (5%–8%) for young women who have just delivered one or two children making it one of the highest in the world [6]. The prevalence is very high in India because Indian women, especially those with poor socioeconomic status, are anemic and malnourished (‘maternal depletion syndrome’) with poorly developed pelvic floor tissues and the additional insult of one or more vaginal deliveries at home is sure to bring down the cervix and uterus. Increasing birth weight, instrumental delivery, fetal malposition and length of labor have all been identified in these studies as further risk factors. It must be noted however, that POP is observed in nulliparous women as well as those delivering by caesarean section only, and therefore other risk factors do need consideration [7,8]. A link between intrapartum trauma at vaginal delivery leading to denervation of the pelvic floor muscles is also well established [9].
A further vaginal approach to managing uterine prolapse surgically is the Manchester-Fothergill procedure, first described in 1888 and then modified in 1915. It involves amputation of the cervix, with plication of the uterosacral ligaments and fixation to the remaining cervico uterine body. The procedure was commonly used for many years; however, it fell out of routine use over the last two decades. This has resulted in there being limited available efficacy data, and the ICS to deem the procedure as having a limited role in contemporary practice. The manchester operation was later modified by VN Shirodkar who described uterosacral advancement operation; in this modification, cervix is not amputated.
In the evolution of conservative operations for prolapse, many sling operations were described in India that soon became very popular because of their simplicity and effectiveness. Initially body tissues like fascia lata and rectus sheath were used, but later given up. Native fascia was replaced by synthetic slings that produce minimal tissue reaction and remain unabsorbed giving lifelong support. Surgical treatment of genital prolapse in young women creates two problems:
• The repair method can jeopardize future
childbearing.
• There can be recurrence of prolapse following
subsequent vaginal delivery.
This is what happens with the traditional fothergills operation. The inert slings, however, do not create these problems. There has been a paradigm shift in the type of material used to create new support for the prolapsed uterus. Traditional operations like fothergills use native fascia for repair, the same endopelvic fascia that was the cause of the prolapse: This falls over time resulting in recurrence, whereas modern sling operations use a prosthetic material like mersilene which gives lifelong support. This is also the reason why the rectus sheath used in original cervicopexy was replaced by prosthetic tape. Thus, in modern gynecology, native fascia has been abandoned in favor of prosthetic materials.
Since India has the largest prevalence of nulliparous prolapse, it is no surprise that Indian gynecologists have devised most of the conservative operations for genital prolapse. It is important look at certain important aspects of the supporting sling: Virkrud 14 classification of sling operations is based on the following criteria:
• Position of support: Whether the support is coming
from the anterior aspect or posterior aspect or is
neutral or both anterior and posterior. Anterior
support will cause retroversion which is bad whereas
posterior support is good because it anteverts the
uterus.
• Type of support: Whether it static like the sacral
promontory/anterior superior iliac spine or dynamic
like the anterior abdominal wall (comes into action
only when required).
• Type of loop formed: Whether it is closed loop sling
operation or open sling operation. Closed loop sling
has one drawback: Should the loop be very narrow,
there is a potential risk of postoperative intestinal
obstruction; hence, open sling is better.
Based on these criteria, VIRKRUD classified sling operations and summarized in TABLE 1.
| Shirodkar's sling | Static, closed loop, posterior sling operation |
| Purandare's cervicopexy | Dynamic, closed loop, anterior sling operation |
| Khanna's sling | Static, open, neutral sling operation |
| Virkud's composite sling | Static+dynamic, open, anterior+posterior sling operation |
| Sonawala's sling | Static, open and unilateral posterior sling |
| Joshi's sling | Static, closed loop, anterior sling operation |
Table 1. Virkud classification of sling operations.
With the above background this study was undertaken to assess the procedures of modified abdominal sling operation and its results.
Materials and Methods
∎ Study setting
Women who attended the gynecology department of the M.R.A. Medical college, Ambedkar Nagar with complaints of uterine prolapse were selected.
In order to decide which patient is suitable for a sling operation, certain selection criteria for must be followed. These are:
• Young women with second or third degree
uterocervical prolapse.
• Uterocervical length of less than five inches.
• Absent or minimal cystocele/rectocele.
• If moderate to large cystocele/rectocele is present, it
should be repaired from below at the same sitting
before performing the sling.
• Not suitable for hypertrophied, lacerated, and
infected cervix.
∎ Exclusion criteria
Obese women, women having uterine pathology, and cervical pathology, previous surgical procedure were not included in the study.
Written informed consent was taken from all the participants.
Sample size distribution and duration of the study.
A total of 25 women are included in the study. They had no other chronic disease. All these women were operated on from June 2015 to June 2022 in the department of obstetrics and gynaecology M.R.A. medical college, Ambedkar Nagar, UP, India.
Women were examined and were submitted to all investigations for major surgery. Performa included name, age, detail address, parity, menstrual history, local examination, pap smear, PV, P/S, and investigations.
A thorough examination was done for utero cervical descent, utero cervical length, cystocele, enterocoele, and rectocele.
Pre operating preparation was done as usual for spinal anesthesia. The procedure performed is modified abdominal sling surgery for prolapse. Women were operated on within seven days of menstruation.
∎ Procedure
This procedure was done laparoscopically by using merceline tape for prolapse. But we did this procedure abdominally (open) by using merceline tape or proline mesh in strip form (when mercelene tape was not available).
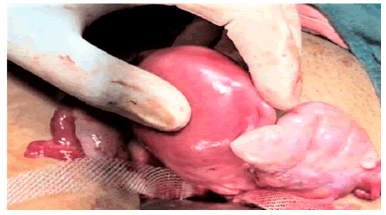
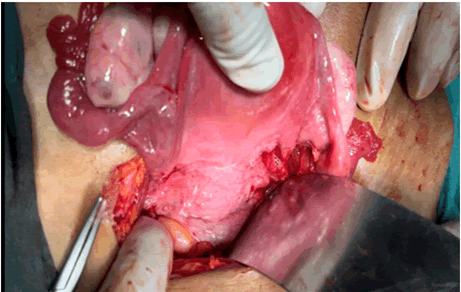
Abdomen was opened in layers by Pf annenstiel incision. Uterus was exteriorized, posterior surface of uterus was exposed and peritoneum over utero sacral ligament (attached at post surface of uterus) was incised and exposed. The length of merceline tape or prolene mesh tape was prepared so that it can pass both side of uterus accurately (around 16-20 cm), after that tape was passed below the both ends of uterosacral ligament and take out anteriorly at the level of junction of fallopian tube and uterus retro peritoneally with the help of long artery forceps (FIGURE 1). Further it is passed up to the ring of inguinal ligament retro peritoneally through the tunnel of round ligament, excess tape is excised and fixed at rectus sheath with prolene no 1 suture (ant abdominal wall) (FIGURE 2). Same procedure was also done on another side of uterus. Hemostasis secured and peritoneum over post surface and anterior openings are closed. After mop and instruments counts abdomen closed in layers.
Prophylactic antibiotics and anti-inflammatory drugs were prescribed for seven days. Postoperative management as usual as in any major surgery. Stitches were removed on the eighth day women were discharged on a ninth day. Follow up was recorded after one month. All women were called for follow up. Many women came; their story is included as long term follow up.
∎ Statistical analysis
The recorded data was compiled and entered in a spreadsheet computer program (Microsoft Excel 2007) and then exported to the data editor page of SPSS version 15 (SPSS Inc., Chicago, Illinois, USA). For all tests, confidence level and level of significance were set at 95% and 5% respectively.
Results
The average age at the time of operation ranged from 24 to 37 years (mean age 30.5 years) (TABLE 2).
All 25 patients underwent modified abdominal sling operation. Out of 20 women, 1 (04%) were nulligravida, 12 (48%) were primiparas and 11 (44%) were multigravida (TABLE 3).
88% of women had come with symptom of mass per vagina. Of the others, 20 patients (80%) had discharge per vagina, 18 patients (72%) had backache, 8 patients (32%) had pain abdomen and 4 patients (16%) had infertility (TABLE 4).
Mean duration of occurrence of prolapse after delivery was 4 years. 8% of the prolapse occurred within one year of child birth, 76% occurred within 3 years of child birth (TABLE 5).
Women with second and third degree of prolapse were operated. 60% had third degree prolapse (TABLE 6). 60% patients had concomitant cystocele, 8% patients had enterocele and 10% had concomitant rectocele (TABLE 7).
Average duration of the surgery was 1 hour 30 minutes to 2 hours (mean 1 hour and 50 minutes). Additional surgeries like tubectomy was performed in 2 (8%), tubal patency test in 4 (16%), ovarian drilling in 4 (16%), and cystocele repair in 15 (60%) patients (TABLE 8).
According to availability of synthetic material available we used proline mesh in 17 (68%) of patients and Mercelene tape in 8 (32%) of patients and result was satisfactory in all cases (TABLE 9).
| Age (years) | Number | Percent |
|---|---|---|
| <20 | 0 | 0 |
| 21-30 | 12 | 48 |
| 31-40 | 13 | 52 |
| >41 | 0 | 0 |
| total | 25 |
Table 2. Age distribution of the patients.
| Parity | Number | Percent |
|---|---|---|
| Nulligravida | 1 | 4 |
| One | 12 | 48 |
| Two | 8 | 32 |
| Three | 3 | 12 |
| Four and above | 0 | 0 |
Table 3. Parity of the patients.
| Complaints | Number | Percent |
|---|---|---|
| Mass per vaginum | 22 | 88 |
| Discharge per vaginum | 20 | 80 |
| Backache | 18 | 72 |
| Pain in abdomen | 8 | 32 |
| Infertility | 4 | 16 |
Table 4. Presenting complaints.
| Duration between delivery and prolapse | Number | Percent |
|---|---|---|
| <1 | 2 | 8 |
| 1 | 6 | 24 |
| 2 | 8 | 32 |
| 3 | 5 | 20 |
| 4 or more | 4 | 16 |
Table 5. Distribution of patients according to duration between delivery and prolapse.
| Degree of prolapse | number | percent |
|---|---|---|
| Second degree | 10 | 40 |
| Third degree | 15 | 60 |
Table 6. Distribution according to degree of genital prolapse.
| Number | Percent | |
|---|---|---|
| Cystocele | 15 | 60 |
| Rectocele | 10 | 40 |
| Enterocele | 2 | 8 |
Table 7. Concomitant organ prolapse.
| Additional surgery performed | Number | Percent |
|---|---|---|
| Tubectomy | 2 | 8 |
| Tubal patency test | 4 | 16 |
| Ovarian drilling | 4 | 16 |
| Cystocele repair | 15 | 60 |
Table 8. Additional surgeries performed.
| Synthetic material used | No of patient | percent |
|---|---|---|
| Proline mesh | 17 | 68 |
| Mercelene tape | 8 | 32 |
Table 9. Distribution on the basis of synthetic material.
Discussion
In summary, there are many different surgical treatment options in women with a prolapse of the middle compartment. No guidelines currently exist to guide the choice of technique. Procedures’ including removal of the uterus comes with a higher rate of serious complications and trends are turning to uterus preserving procedures in women with uterine decent [10]. Sacrohysteropexies have the highest reported success rates but require high technology operating facilities and experienced surgeons. This procedure also comes with higher costs, longer operation times and a low but yet existing risk of mesh erosions. The Manchester fothergill operation is a minimally invasive procedure with satisfactory results and low complication rates as compared to VH and should be considered a valid option.
Next in the evolution of conservative surgery for prolapse many sling surgeries were described which soon became popular because of their simplicity and effectiveness. Initially, native fascia like fascia lata and rectus sheath was used which later got replaced by synthetic slings that produce minimal tissue reaction and remain unabsorbed giving lifelong support [11]. Failure of conservative surgeries like traditional fothergill’s or sling surgeries was because of the use of native fascia for repair, the same endopelvic fascia that has caused prolapse. The use of synthetic materials like merselene tape and mesh in modern sling surgeries has decreased the failure rates and gives lifelong support.
∎ Post-operative period
23 women had an uneventful postoperative period. They were discharged on the 8th or 9th day. One woman developed pain in the left iliac fossa on the third day, she was switched over higher antibiotic and anti-inflammatory and became alright. One woman had deep gaping on stitch removal which was resutured. All women reported after one month as per our advice all were fine.
∎ Long term follow up
• 8 women came for an antenatal check-up and all
were delivered by caesarean section sling was intact
in all cases on follow up.
• Two women came for infertility, after evaluation
bilateral tubes were blocked, so they were send for in vitro fertilization.
• One woman attended our outdoor for urinary tract
infection after two years.
• 10 woman was lost in follow up.
• Woman had abdominal sling operation with bilateral
tubal ligation (family completed at young age 28, 30
years) were alright without any complains.
The limitation of the study was, findings of the present study cannot be generalized to the whole population.
Conclusion
Modified abdominal uterine sling suspension is a novel way of maintaining uterine support for those women specifically requesting for uterine conservation and surgical management of uterine prolapse. For many women, uterine conservation is an absolute necessity to retain future reproductive potential. For others, it remains a matter of personal choice. Newer techniques are being introduced that respond to patient’s desires for such conservative surgery and their desire for minimally invasive techniques.
References
- Haylen BT, Maher CF, Barber MD, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female Pelvic Organ Prolapse (POP). Neurourol Urodyn. 35, 137-168 (2016).
[Crossref] [Google Scholar] [PubMed]
- Hove MCST, Goudzwaard ALP, Eijkemans MJ, et al. The prevalence of pelvic organ prolapse symptoms and signs and their relation with bladder and bowel disorders in a general female population. J Int Urogynecol. 20, 1037-1045 (2009).
- Haylen BT, Maher CF, Barber MD, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female Pelvic Organ Prolapse (POP). Neurourol Urodyn. 35, 137-168 (2016).
[Crossref] [Google Scholar] [PubMed]
- Hendrix SL, Clark A, Nygaard I, et al. Pelvic organ prolapse in the women's health Initiative: Gravity and gravidity. Am J Obstet Gynecol. 186, 1160-1166 (2002).
[Crossref] [Google Scholar] [PubMed]
- Smith FJ, Holman CA, Moorin RE, et al. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 116, 1096-1100 (2010).
[Crossref] [Google Scholar] [PubMed]
- Mant J, Painter R, et al. Epidemiology of genital prolapse: Observations from the Oxford family planning association Study. Br J Obstet Gynaecol. 104, 579-585 (1997).
[Crossref] [Google Scholar] [PubMed]
- Harris RL, Cundiff GW, Coates KW, et al. Urinary incontinence and pelvic organ prolapse in nulliparous women. Obstet Gynecol. 92, 951-954 (1998).
[Crossref] [Google Scholar] [PubMed]
- Rortveit G, Brown JS, Thom DH, et al. Symptomatic pelvic organ prolapse: Prevalence and risk factors in a population based, racially diverse cohort. Obstet Gynecol. 109, 1396-1403 (2007).
[Crossref] [Google Scholar] [PubMed]
- Allen RE, Hosker GL, Smith AR, et al. Pelvic floor damage and childbirth: A neurophysiological study. Br J Obstet Gynaecol. 97, 770-779 (1990).
[Crossref] [Google Scholar] [PubMed]
- Busacchi P, Perri T, Paradisi R, et al. Abnormalities of somatic peptide-containing nerves supplying the pelvic floor of women with genitourinary prolapse and stress urinary incontinence. Urol. 63, 591-595 (2004).
[Crossref] [Google Scholar] [PubMed]
- Marshall KW, Walsh DM, Baxter GD. The effect of a first vaginal delivery on the integrity of the pelvic ‘oor musculature. Clin Rehabil. 16, 795-799 (2002).
[Crossref] [Google Scholar] [PubMed]