Brief Report - International Journal of Clinical Rheumatology (2021) Volume 16, Issue 5
Severe coronal re-infection and issues of mechanisms, monitoring and therapy
- *Corresponding Author:
- Rozin Alexander P
B. Shine Rheumatology Institute, Rambam Health Care Campus and Technion, Haifa, Israel
E-mail: a_rozin@rambam.health.gov.il
Abstract
Recurrent COVID-19 infection with severe lung disease and periarthritis presented. Possible mechanisms for recurrent disease, periarthritis, and treatment options discussed.
Keywords
recurrent COVID-19 infection • venous blood gases monitoring • hypersensitivity • reactive periarthritis • insistant-complex therapy
Do we feel invincible after COVID-19 vaccination or recovering from COVID-19 disease? Our experience is not testimony for this statement. A 45-year-old man, economist and lecturer at university, treated with metformin from diabetes melllitus, felt respiratory disease with sore throat, cough and mild fever on December 2020. RT-PCR was positive for COVID-19. His disease course was mild, unremarkable, with home follow-up without any respiratory distress and without saturation control. Complete recovery followed for ten days. He got green certificate of recovery. He has not had a time to get vaccine. Three month before for similar respiratory disease, his RT-PCR was negative for COVID-19. 40 days later after his COVID-19 serology test for antiviral antibodies showed lower level (27 AU). Two months later, he developed high fever 39.6, which lasted two weeks with severe respiratory distress, lower oxygen saturation (80%), cough, sore throat, severe myalgia and exhaustion. RT-PCR for COVID-19 was again positive. He admitted to our hospital.
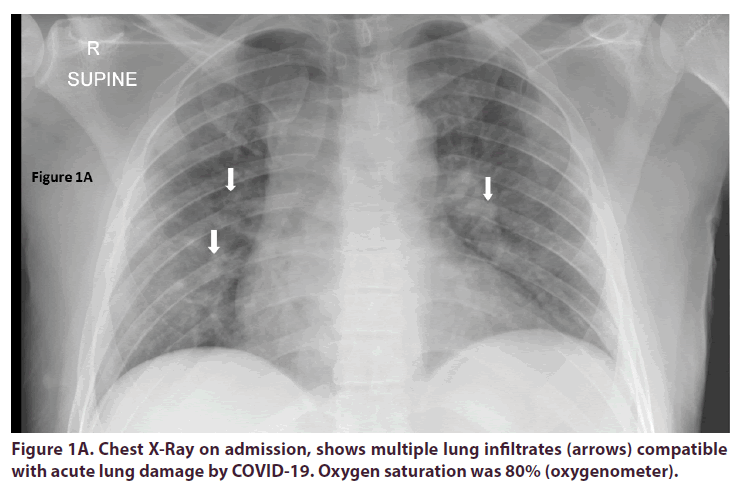
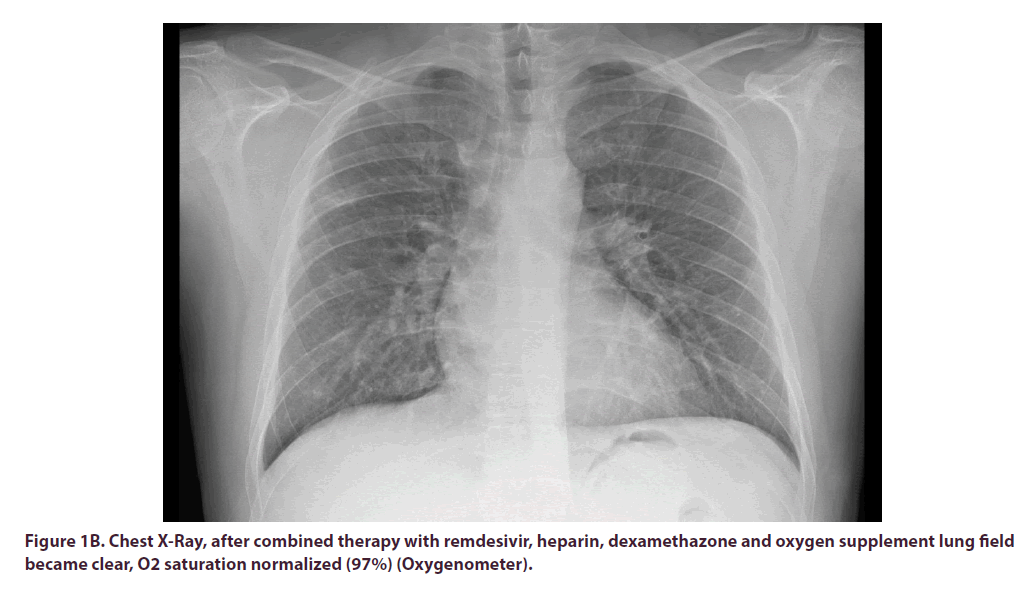
Data of venous blood gases dynamic presented in Table 1. Unfortunately, we rarely use venous blood gases. One can see severe hypoxemia and very valuable dynamic.It is necessary to be familiar with normal values of venous blood gases and to use it for dynamic assessment of oxygenation [1,2]. There were many bilateral lung infiltrates (Figure 1A) on admission explaining severe respiratory distress, which are compatible with COVID-19 infection. Remdesivir IV, heparin subcutaneously, dexacort per os and oxygen supplement were initiated and rapid improvement followed (Table 1 and Figure 1B). On discharge, 6 days after admission COVID-19 IgG-Architect 6.89 (positive above 1.4), COVID-19 19S IgG-Architect was of 11345 AU (50-150: norm for recovery or vaccinated). Three days later RT-PCR was negative for COVID-19 (23 days after the second disease initiation).
Figure 1B. Chest X-Ray, after combined therapy with remdesivir, heparin, dexamethazone and oxygen supplement lung field became clear, O2 saturation normalized (97%) (Oxygenometer).
| O2 parameter | Day 2 | Day 6 | Normal value [2] |
|---|---|---|---|
| So2 (POC) (%) | 24.7 | 55.4 | 60-85 |
| Po2 (POC) (mmHg) | 12 | 37 | 30-50 |
Table 1. Venous Blood Gases' Dynamic of patient with active COVID-19 infection and lung involvement during combined therapy: Remdesivir, Heparin, Dexamethazone, Oxygen.
The targeting genes for RT-PCR of both diseases were N NUCLEAR CAPSID, RdRP, E GENE, S GENE. The test protocol adopted was ALLPLEX 2019 n-COV 2019. During first infection patient had home quarantine and follow-up by special coronal service of outpatient clinic. Second infection treated at specialized coronal intensive therapy unit isolated from other departments. There was not any travel or contact history between two events.
Due to urinary tract infection caused by enterococcus sensitive to Ciprofloxacin, patient continued therapy on outpatient basis. Seven days thereafter-bilateral ankle pain and swelling developed. X-Ray and ultrasound showed only soft tissue swelling consistent with reactive periarthritis. Short course of dexamethasone and etoricoxib followed with rapid revival.
RT-PCR positive twicely, antibodies to COVID-19 twicely, characteristic respiratory symptoms and severe morphological and functional lung impairment confirm two cases of unrelated coronal infection separated by three months. The question is as follows: where was the immune system? Survivals of smallpox preserved immunity to this disaster disease forever! What about immunity to COVID-19, which has affected 130 millions-people overworld and 3 million, have dead? Was the immune system incompetent? May be we faced virus mutated? Second event was very serious, dangerous and life threatening.Second event should be much easier and smoother. After formation of immunity due to the first meeting with virus. With antibodies and cell-mediated immunity and memory lymphocytes!
Where is it everything? Hypersensitivity? Second event is hypersensitivity to repeated meeting of viral antigens!
May be vaccination after first event was able to prevent second infection? Is a need to perform vaccination after second infection? With very high level of antibodies? I does not look so. Who knows?
Physicians of our hospital worked wonders. Standard regime including anticoagulant, dexamethasone, remdesivir and oxygen proved to be very effective and saved out patient for 5 days! We took attention for interesting behavior of corona virus! It respects medical skills and insistence! It see it, retreats, and gives up. Most of severe complications of corona infection are reversible! Cardiac tamponade due to virus or vaccination is reversible [3,4]. Give chance to personal to fight, to use its skill and knowledge; do not put down your hands and your thought! Do not stop to try another chance.
Severe life threatening white lung condition or cardiogenic shock due to myocarditis Kawasaki like – do not hesitate to include early five-component therapy:
1. Anti-cytokine tocilizumab
2. Immunomodulation: pulse methylprednisolone 1g/day for 3 days and further 100mg/day IV until stabilization
3. Anticoagulant therapy early: subcutaneous enoxaparin or heparin in case of renal failure
4. Oxygen supplement or ECMO (Extra-Corporal Membrane Oxygenation)
5. Early wide range of antibiotic in order to prevent secondary infection.
We observed heroic efforts of ECMO for 3m to4 msuccessful, multiple consilium group decision and successes and, sorry, losses.
Repeated coronal infection during3 months is outstanding event. We should unravel this enigma!
References
- Tavakol K, Ghahramanpoori B, Fararouei M. Prediction of Arterial Blood pH and Partial Pressure of Carbon dioxide from Venous Blood Samples in Patients Receiving Mechanical Ventilation. J. Med. Signals. Sens. 3, 180(2013).
- Byrne AL, Bennett M, Chatterji R et al. Peripheral venous and arterial blood gas analysis in adults: are they comparable? A systematic review and meta-analysis. Respirology. 19, 168 (2014).
- Dabbagh MF, Aurora L, D’Souza P. Cardiac Tamponade Secondary to COVID-19. JACC. 2, 1326–1330 (2020).
- Rozin AP, Yalonetsky S. Images of COVID-19 Vaccination. Int. J. Case. Rep. Clin. Image. 3(1), 144 (2021).