Case Report - International Journal of Clinical Rheumatology (2020) Volume 15, Issue 5
Relapsing polychondritis presenting in a patient with cryptogenic organizing pneumonia
- Corresponding Author:
- Kathlyn Camargo
Department of Internal Medicine, University of Central Florida College of Medicine, Orlando, USA
E-mail: Kathlyn.CamargoMacias@ucf.edu
Abstract
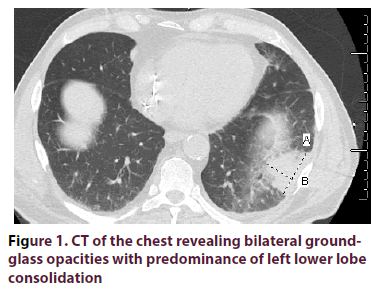
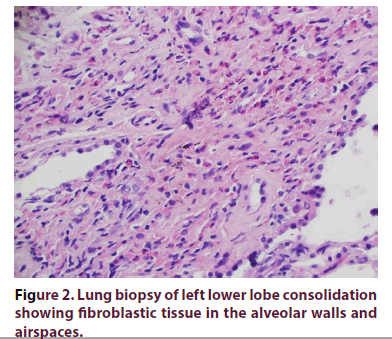
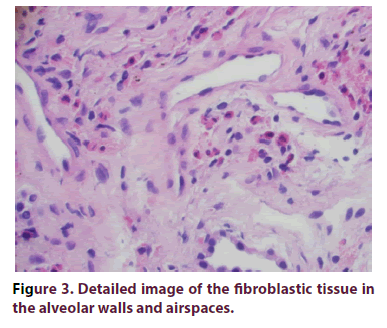
Relapsing Polychondritis (RP) is an autoimmune disease that affects cartilaginous tissues in the body, including lower respiratory tract. Involvement of the pulmonary interstitium is very rare. We present a 67-year-old Caucasian man presented to the clinic with one-year of recurrent dyspnea and dry cough along with worsening anemia and thrombocytopenia. CT of the chest demonstrated diffuse, bilateral (left > right) multifocal peribronchovascular ground glass opacities with mediastinal lymphadenopathy. All rheumatologic serology workup was negative as well as infectious workup. Lung biopsy of the left lower lobe consolidation showed plugs of fibroblastic tissue incorporated into alveolar walls and airspaces consistent with COP. No features of malignancy or granulomatous process were seen. Oral prednisone was started and tapered over the next 3 months with improvement of his respiratory symptoms. Two weeks later, he developed bilateral ear pain/redness and conjunctivitis. CT of the sinuses revealed mild prominence in the left nasopharyngeal soft tissue. Biopsy of this lesion showed inflammatory infiltrative changes and RP was diagnosed. Adalimumab was started. However, the patient developed worsening dyspnea that required supplemental oxygen and hospitalization. High dose steroids were again added, along with oral cyclophosphamide. The patient had significant clinical and radiological improvement over the next 6 months. Interstitial lung disease has been rarely associated with RP. Most of the lower respiratory track involvement is in the trachea. We present a case of cryptogenic organizing pneumonia in association with relapsing polychondritis.
Keywords
relapsing polychondritis • autoimmune disease • inflammation
Introduction
Relapsing Polychondritis (RP) is an autoimmune disease characterized by recurrent inflammation of cartilaginous tissues in the body, including the lower respiratory tract. RP can occur at any age, with reported cases ranging from pediatric to geriatric-age population [1]. This disease affects both genders with a slight female predominance [2]. The underlying pathogenesis is still unclear, however both humoral and cell-mediated mechanisms play a significant role in RP. We report a rare case of relapsing polychondritis associated with Cryptogenic Organizing Pneumonia (COP).
Case
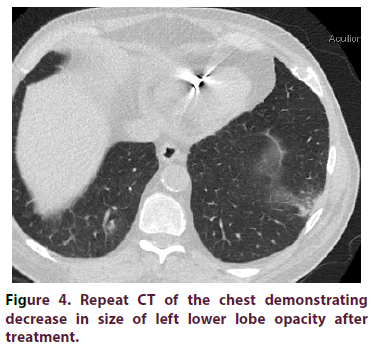
A 67-year-old Caucasian man with a past medical history of hypertension and diabetes mellitus (type II) presented to our clinic with a one-year history of recurrent dyspnea and dry cough along with worsening anemia and thrombocytopenia. The patient did not have any previous personal or family history of rheumatologic disease. In the year prior to presentation, he received multiple antibiotic treatments for suspected pneumonia. Review of Systems (ROS) was negative for fatigue, night sweats, weight loss, joint pain, joint swelling or rash. Recent Computer Tomography (CT) of the chest demonstrated diffuse, bilateral (left > right) multifocal peribronchovascular ground glass opacities with mediastinal lymphadenopathy (Figure 1). All of the following serologic workup was negative/ within normal limits: Antinuclear antibody with immunofluorescence assay (ANA with IFA), Rheumatoid Factor (RF), anti-CCP, angiotensin converting Enzyme (ACE) level, Antineutrophil Cytoplasmic Antibodies (ANCA) panel, and quantiferon gold. Serum Protein Electrophoresis (SPEP) showed an IgG-kappa monoclonal protein, however bone marrow biopsy exhibited polyclonal lymphoplasmacytosis. Erythrocyte sedimentation rate was markedly elevated >120 mm/hr. Preceding infectious workup was negative, including an unremarkable bronchioalveolar lavage culture. Lung biopsy of the left lower lobe consolidation via transthoracic needle aspiration represented plugs of fibroblastic tissue incorporated into alveolar walls and airspaces consistent with COP (Figures 2,3). Biopsy did not reveal any histopathologic features of malignancy or a granulomatous process. The patient was subsequently started on oral prednisone 60mg/day for three months, which was then tapered over the next three months. The patient markedly improved after prednisone, with complete resolution of dyspnea and dry cough. Two weeks after prednisone discontinuation, he developed a pressure sensation over his left nostril accompanied with bilateral ear pain/redness, and bilateral conjunctivitis. CT of the sinuses revealed mild prominence in the left nasopharyngeal soft tissue. Biopsy of the left nasopharynx showed inflammatory infiltrative changes and a diagnosis of relapsing polychondritis was made. Adalimumab was initiated. Despite therapy, the patient developed worsening dyspnea that required supplemental oxygen. Adalimumab was discontinued, and the patient was resumed on high dose steroids. Cyclophosphamide (oral) was started. Ensuing labs demonstrated improvement of anemia and thrombocytopenia coinciding with significant clinical improvement (supplemental O2 was no longer required). Follow-up CT of the chest 1 month later showed a decrease in the size and number of the patchy ground-glass opacities (Figure 4).
Discussion
Relapsing polychondritis is a rare autoimmune disorder characterized by recurrent and chronic inflammation of cartilaginous tissues, such as the elastic cartilage of ear/nose and fibrocartilage of the tracheobronchial tree [1,2]. Bilateral auricular chondritis is the most common clinical manifestation and it can be observed in up to 90% of RP patients. Lower respiratory tract involvement arises in about 50% of patients and characteristic CT-findings include thickening of the tracheal wall with destruction of the cartilaginous rings [2,3]. After extensive literature review, Involvement of pulmonary interstitium was not well-described [1] however a small cohort study by Lin, et.al showed that approximately 30% of RP patients had CT findings consistent with interstitial lung disease and that half of patients had mediastinal lymphadenopathy [4]. Initial treatment of RP with high-dose steroids is required to achieve symptom control and sometimes long-term use is required to prevent relapses [2]. Cyclophosphamide, cyclosporine, azathioprine and methotrexate have been used, alone or in-addition to steroids, for lifethreatening disease [2]. Literature regarding response to Tumor Factor Necrosis (TNF) inhibitors such as infliximab, adalimumab and etanercept are not conclusive, however biologics are reserved for refractory cases [2]. Our patient adequately responded to corticosteroids and cyclophosphamide. To our knowledge, there are no reported cases in the literature of COP associated with RP. It is imperative to recognize this unusual presentation, as early diagnosis of RP and prompt initiation of immunosuppressive therapy can prevent long-term complications.
Conclusion
Relapsing polychondritis is a rare autoimmune disorder characterized by recurrent and chronic inflammation of cartilaginous tissues. It is imperative to recognize interstitial lung disease such as cryptogenic organizing pneumonia as part of relapsing polychondritis, as early diagnosis of RP and prompt initiation of immunosuppressive therapy can prevent long-term complications.
References
- Rafeq S, Trentham D, Ernst A. Pulmonary manifestations of relapsing polychondritis. Clin. Chest. Med. 31(3), 513–518 (2010).
- Borgia F, Giuffrida R, Guarneri F et al. Relapsing Polychondritis: An Updated Review. Biomedicines. 6(3) (2018).
- McAdam LP, O'Hanlan MA, Bluestone R et al. Relapsing polychondritis: prospective study of 23 patients and a review of the literature. Medicine (Baltimore). 55(3), 193–215 (1976).
- Lin ZQ, Xu JR, Chen JJ et al. Pulmonary CT findings in relapsing polychondritis. Acta Radiol, 51(5), 522–526 (2010).