Case Report - Interventional Cardiology (2023) Volume 15, Issue 5
Rare occurrence of chronic thromboembolic pulmonary hypertension in adolescents: Case report
- Corresponding Author:
- Carlos Alberto Guzmán-Serrano
Clinical Research Center, Fundación Valle del Lili, Cali, Colombia,
E-mail: carlos.guzman.s@fvl.org.co
Received date: 09-Nov-2023, Manuscript No. FMIC-23-119695; Editor assigned: 10-Nov-2023, PreQC No. FMIC-23-119695 (PQ); Reviewed date: 24-Nov-2023, QC No. FMIC-23-119695; Revised date: 01-Dec-2023, Manuscript No. FMIC-23-119695 (R); Published date: 08-Dec-2023, DOI: 10.37532/1755- 5310.2023.15(5).757
Abstract
We report a 17-year-old boy with an impairment of functional class. Computed tomography by angiography shows pulmonary thromboembolism, and cardiac catheterization finds systemic pulmonary hypertension with elevated pulmonary resistance. The patient had a sudden impairment and was brought to thromboendarterectomy with multiple thrombi. Good evolution is shown with improvement in his functional class. Few reports of thromboembolic pulmonary hypertension exist in pediatrics.
Keywords
Pulmonary hypertension • Pulmonary thromboembolism • Thromboendarterectomy • PediatricReserve
Introduction
Chronic Thromboembolic Pulmonary Hypertension (CTEPH) is an uncommon yet potentially curable form of pulmonary hypertension, defined as an increase in pulmonary pressure and vascular resistance due to the presence of a chronic pulmonary thrombi [1,2]. It is characterized by rapid a progression with significant morbidity and mortality. Approximately 1%-2% of patients with acute pulmonary embolism experience CTEPH. We aim to report a rare case of chronic thromboembolic pulmonary hypertension in a 17-year-old male patient.
Case Report
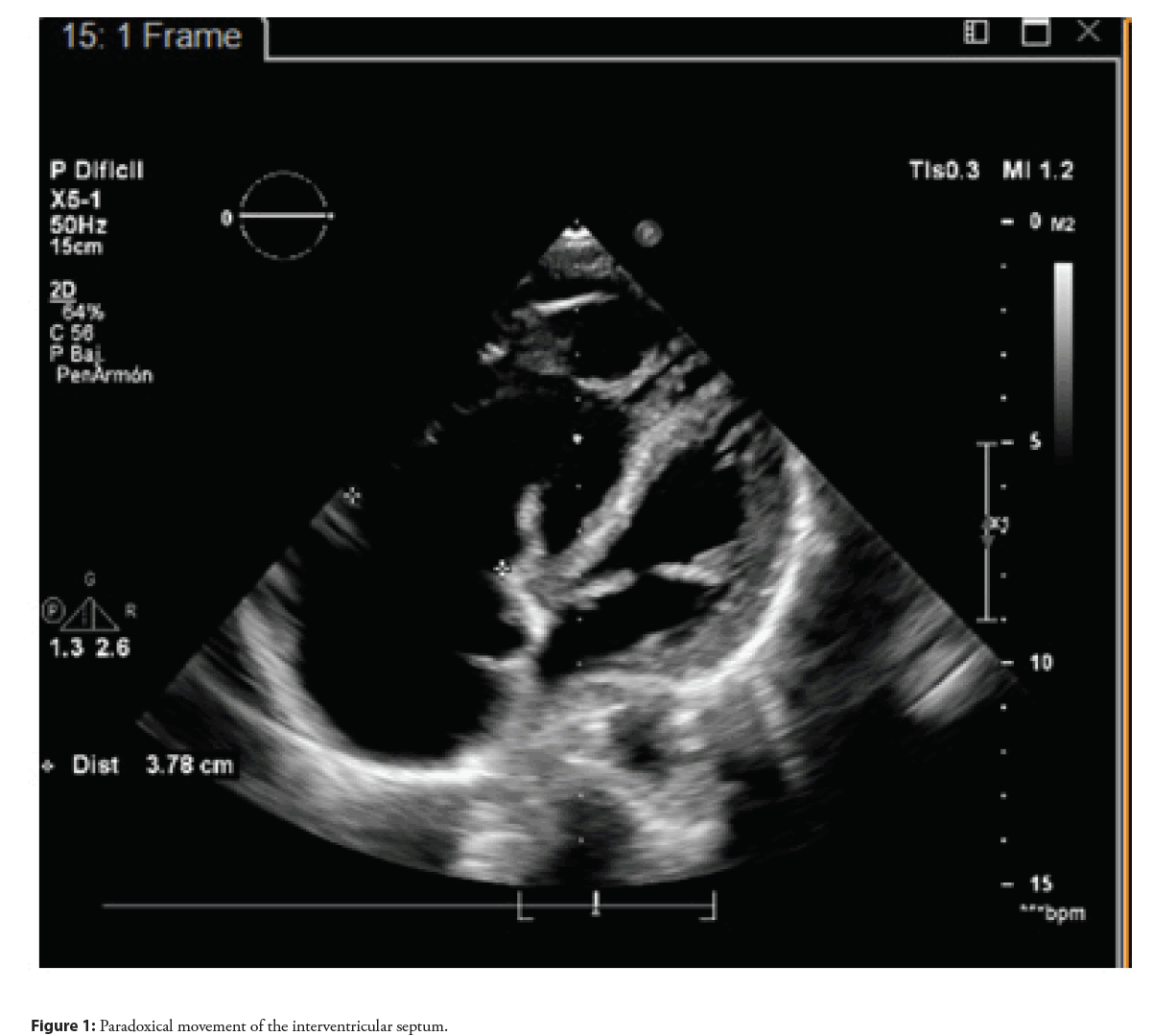
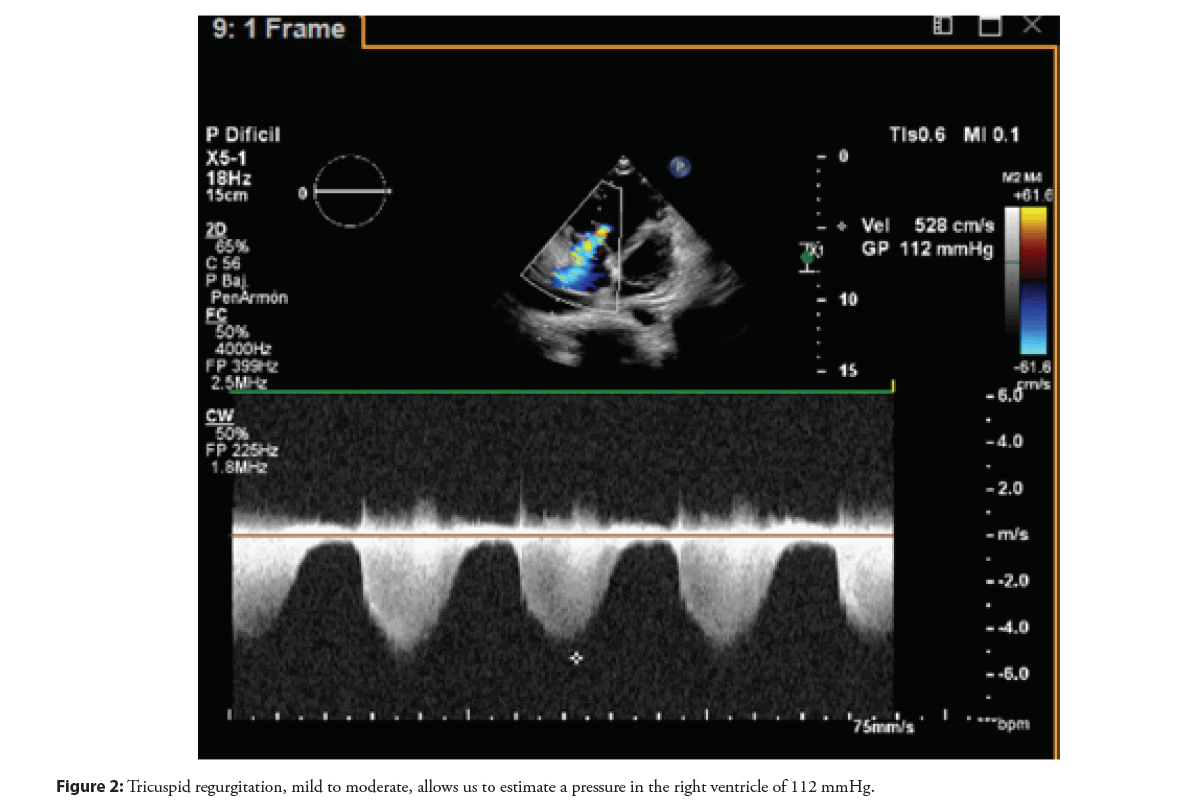
A 17-year-old male patient with no previous clinical history, two years of progressive impairment of his functional class, with dyspnea on moderate exertion (NYHA III/ IV)associated with hemoptysis and palpitations. Echocardiogram reports moderate right atrial dilation, interventricular septum deviation toward the left with dilatation of the inferior cava vein and reversed flow in the hepatic veins, with systolic flattening of the interventricular septum and paradoxical movement of the interventricular septum, mild to moderate tricuspid regurgitation, which allows estimating pressure in the right ventricle of 112 mmHg and mild pulmonary failure with estimated mean pulmonary artery pressure of 20-25 mmHg (Figures 1 and 2).
Upon these findings, Computed Tomography angiography (angioCT) of the chest was taken, which showed evidence of a chronic-appearing thrombus in the main pulmonary artery, with extension to the right and left artery and its branches. The pulmonary trunk measures 28 mm, with a pulmonary trunk/aorta ratio>1, dilating the right cardiac cavities and absence of opacification of the right subclavian vein associated with collateral circulation. Pulmonary scintigraphy evidenced bilateral multi-lobar pulmonary thromboembolism, with angiography confirmation of pulmonary thromboembolism.
In the search for the etiology, studies were conducted, discarded thrombophilia and others coagulation disorders were. It was considered initial medical management with anticoagulation due to acute thrombi.
The patient was taken to diagnostic cardiac catheterization, finding pulmonary artery pressure at 75/46/56 mmHg with systemic pressure at 74/46/56; 56% pulmonary establishment was demonstrated with 100% normal aortic saturation and average 76% saturation of the cava vein, which allowed having a pulmonary flow/systemic flow calculation of 0.6. Pulmonary Vascular Resistance (PVR) is elevated by 15 WU, for systemic resistance of 14 WU, considering systemic pulmonary hypertension of pulmonary establishment with high pulmonary resistance.
Twenty-four hours after the procedure, the patient had sudden dyspnea and diaphoresis, hypotensive and desaturated on physical examination, with respiratory distress and fixed doubling of the second noise. The patient was taken for thromboendarterectomy, with evidence of multiple thrombi in the trunk of the pulmonary branch, both branches and the right atrium (Figure 3). After surgical management, the patient was discharged, sent home without oxygen requirement, and controlled with rivaroxaban and diuretic. Follow-up shows improvement in his functional class (NYHA II), tolerating low-intensity physical activity.
The reported case was reviewed and approved, and individual patient consent was obtained following institutional guidelines. In accordance with our institution’s policies, all protected health information was deleted.
Results and Discussion
Chronic thromboembolic pulmonary hypertension is a rare type of pulmonary hypertension. It occurs when there is damage and blockage of the pulmonary blood vessels, leading to an increase in pulmonary arterial pressure and PVR [3,4]. This, in turn, causes a gradual deterioration in the functioning of the right side of the heart and a decline in overall physical well-being. CTEPH symptoms may be vague, being exertional dyspnea the most common finding, and physical findings are also non-specific. Although patients may have atypical symptoms that are not always recognized or be asymptomatic. Delayed diagnosis (median 10 months) underscores the need for early recognition.
In the evaluation of patients with chronic thromboembolic pulmonary hypertension, it is essential to assess for coagulation disorders [5]. Further tests may be warranted based on the patient’s family history and medical background, primarily to identify and exclude potential associated risk factors. About one third of patients have a positive family history of thromboembolism or a known hypercoagulable condition. Other risk factors include antiphospholipid syndrome, splenectomy, sickle cell disease, thyroid replacement therapies, and a history of malignancies, among others [6]. Our patient had no family history of clotting disorders or previous symptoms that suggest some pathology or thromboembolism risk factors. All available studies were made, but there is still no clarity about the exact etiology, and we consider that it is idiopathic chronic thromboembolic pulmonary hypertension.
Concerning treatment, there have been developments in specific therapies that have enhanced the survival of pediatric patients [7]. Currently approved medical therapies target one of three endothelium-based pathways [8]. However, when medical treatment fails, pulmonary thromboendarterectomy is an important curative therapeutic option in selected patients, reporting lower morbidity and mortality than lung transplants [9]. The most significant case series of pediatric patients with chronic thromboembolic pulmonary hypertension comprised 17 patients aged 18 or younger who underwent pulmonary thromboendarterectomy surgery at a single institution. The study reported favorable outcomes, including improved functional status, cardiopulmonary hemodynamics, and a long-term survival rate of 87.5%. However, it also noted a higher rethrombosis rate in pediatric patients compared to adults (38% vs. 1-4%). Additionally, over half of the patients did not exhibit any clear signs of acute embolism or deep venous thrombosis. This, as seen in our patient, underscores the importance of maintaining a high level of suspicion for pulmonary vascular disease in children experiencing exercise intolerance or exertional dyspnea. Performing a ventilation-perfusion scan in these children to detect chronic thromboembolic pulmonary hypertension is imperative, as a routine scan will not completely rule out thromboembolic pulmonary hypertension [10].
Conclusion
In our case, a successful pulmonary thromboendarterectomy was performed, and the patient is now asymptomatic and recovering well. Few cases of thromboembolic pulmonary hypertension in children have been reported, but thromboendarterectomy has proven to be feasible and well tolerated. Despite its apparent low frequency, it is essential to have a high suspicion index and identify the proper risk factors that might be involved in the disease so they can be eliminated or given specific treatment and thus change the patient’s prognosis.
References
- Mulchrone A, Kellihan HB, Forouzan O, et al. A large animal model of right ventricular failure due to chronic thromboembolic pulmonary hypertension: A focus on function. Front Cardiovasc Med. 5:189 (2019).
- Viswanathan G, Kirshner HF, Nazo N, et al. Single-cell analysis reveals distinct immune and smooth muscle cell populations that contribute to chronic thromboembolic pulmonary hypertension. Am J Respir Crit Care Med. 207(10):1358-1375 (2023).
- Humbert M, Guignabert C, Bonnet S, et al. Pathology and pathobiology of pulmonary hypertension: State of the art and research perspectives. Eur Respir J. 53(1):1801887 (2019).
- Teerapuncharoen K, Bag R. Chronic thromboembolic pulmonary hypertension. Lung. 200(3):283-299 (2022).
- Madani MM, Wittine LM, Auger WR, et al. Chronic thromboembolic pulmonary hypertension in pediatric patients. J Thorac Cardiovasc Surg. 141(3):624-630 (2011).
- Spencer R, Valencia VG, Takeda K, et al. Chronic thromboembolic pulmonary hypertension in a child with sickle cell disease. Front Pediatr. 8:363 (2020).
- Rajpurkar M, Biss T, Amankwah EK, et al. Pulmonary embolism and in situ pulmonary artery thrombosis in paediatrics. A systematic review. Thromb Haemost. 117(6):1199-1207 (2017).
- Kim JS, McSweeney J, Lee J, et al. Pediatric cardiac intensive care society 2014 consensus statement: pharmacotherapies in cardiac critical care pulmonary hypertension. Pediatr Crit Care Med. 17(3 Suppl 1):S89-S100 (2016).
- Johnson JN, Driscoll DJ, McGregor CGA, et al. Pulmonary thromboendarterectomy in adolescents and young adults. Pediatr Pulmonol. 45(6):614-618 (2010).
- Verbelen T, Cools B, Fejzic Z, et al. Pulmonary endarterectomy in a 12‐year‐old boy with multiple comorbidities. Pulm Circ. 9(4):1-4 (2019).