Case Report - Interventional Cardiology (2024) Volume 16, Issue 4
Plain balloon angioplasty still has a role in small vessel coronary artery disease: A case report
- Corresponding Author:
- Abdelaziz Ahmed Abdelaziz
Department of Cardiology, Teachers Hospital, Cairo, Egypt,
E-mail: abdelaziz_1975@yahoo.co
Received date: 25-Jul-2024, Manuscript No. FMIC-24-143224; Editor assigned: 29-Jul-2024, PreQC No. FMIC-24-143224 (PQ); Reviewed date: 16-Jul-2024, QC No. FMIC-24-143224; Revised date: 23-Jul-2024, Manuscript No. FMIC-24-143224 (R); Published date: 01-Aug-2024, ![]()
Abstract
Coronary Artery Disease (CAD) remains a significant public health issue, with Small Vessel Disease (SVD) representing a challenging subtype. While Percutaneous Coronary Intervention (PCI) with Drug-Eluting Stents (DES) has revolutionized the management of CAD, its role in SVD remains debated, particularly in the context of potential complications like stent thrombosis and restenosis. This case report presents a compelling example where Plain Balloon Angioplasty (PBA) successfully treated a patient with SVD, highlighting its continued relevance in specific clinical scenarios. Patient concerns: A female patient 60 years old, suffered from Insulin-dependent Diabetes Mellitus (DM), Hypertension (HTN), and dyslipidemia and had typical chest pain for the last three months on minimal exertion. The Electrocardiogram (ECG) and Echo revealed ischemic changes and regional wall motion abnormality. Diagnoses: The coronary angiography results revealed multivessel coronary artery disease. Interventions: PCI was done using balloon angioplasty to small-sized vessels (<3 mm in diameter) and DES to Left Anterior Descending Artery (LAD) and Right Coronary Artery (RCA). Then, follow-up angiography was done that showed patent stents and excellent results for balloon angioplasty-treated small vessels. Outcomes: Two years of follow-up of small coronary artery disease vessels treated with PBA were comparable to DES. Conclusion: PBA in small-sized coronary vessels showed a stent-like effect both in immediate and long-term follow-up.
Keywords
Plain balloon angioplasty • Small vessel disease • Coronary artery disease • Case report
Abbreviations
DM: Diabetes Mellitus; DES: Drug-Eluting Stent; ECG: Electrocardiogram; HTN: Hypertension, LAD: Left Anterior Descending Artery; LCX: Left Circumflex Artery; LM: Left Main Artery; OM: Obtuse Marginal Branches; PCI: Percutaneous Coronary Intervention; RCA: Right Coronary Artery; TIMI III: Thrombolysis in Myocardial Infarction-Grade III; BVS: Bioresorbable Vascular Scaffolds; BARI: Bypass Angioplasty Revascularization Investigation; CABG: Coronary Artery Bypass Grafting; BMS: Bare-Metal Stent
Introduction
Among the therapeutic interventions, DES have revolutionized the management of CAD by substantially reducing restenosis rates and improving long-term outcomes [1]. However, the treatment of SVD, characterized by stenotic lesions in vessels less than 2.5-3.0 mm in diameter, poses unique challenges [2]. The higher restenosis rates and technical difficulties associated with stenting in small vessels have led to an ongoing debate regarding the optimal revascularization strategy for SVD.
PBA, one of the earliest percutaneous coronary interventions, has seen a resurgence of interest in certain clinical scenarios. Despite the advent and widespread adoption of DES, PBA retains a critical role in specific contexts, particularly in the management of SVD [3].
The anatomy of small coronary vessels presents significant challenges to the deployment of stents. The limited diameter not only complicates the stent implantation process but also increases the likelihood of stent-related complications such as restenosis and thrombosis. Moreover, patients with SVD often have diffuse atherosclerotic disease, making it difficult to achieve optimal stent expansion and apposition [4].
One of the primary advantages of PBA in SVD is its procedural simplicity and reduced risk of complications associated with stent implantation. PBA involves the inflation of a balloon catheter at the site of the lesion, leading to plaque compression and vessel dilation. This technique avoids the potential issues of stent malapposition and late stent thrombosis. Additionally, advancements in balloon technology, such as cutting balloons and scoring balloons, have improved the efficacy of PBA by enhancing lesion modification and reducing the incidence of elastic recoil. Economic considerations also play a role in the decision-making process for the treatment of SVD. PBA is generally less expensive than DES implantation, which can be a significant factor in healthcare systems with constrained resources or in patient populations where cost is a major concern. The cost-effectiveness of PBA, combined with its technical feasibility, makes it a compelling option in select cases [5].
This case report aimed to reaffirm the utility of PBA in contemporary practice, advocating for a more nuanced and patient-specific approach to the treatment of CAD.
Case Presentation
A 60-year-old Egyptian female was admitted to the cardiology department of Teachers Hospital with STEMI. The patient suffered from other co-morbidities including insulin-dependent DM, HTN, and dyslipidemia. The patient had typical chest pain on minimal exertion for the last three months. The diagnosis of the case was confirmed by the ECG that revealed ST segment elevation in lead I and aVL with inverted T wave and reciprocal ST segment depression in aVR and V4-V6. Furthermore, the echocardiography showed regional wall motion abnormality in the form of mid and basal lateral wall hypokinesia. Troponin was positive.
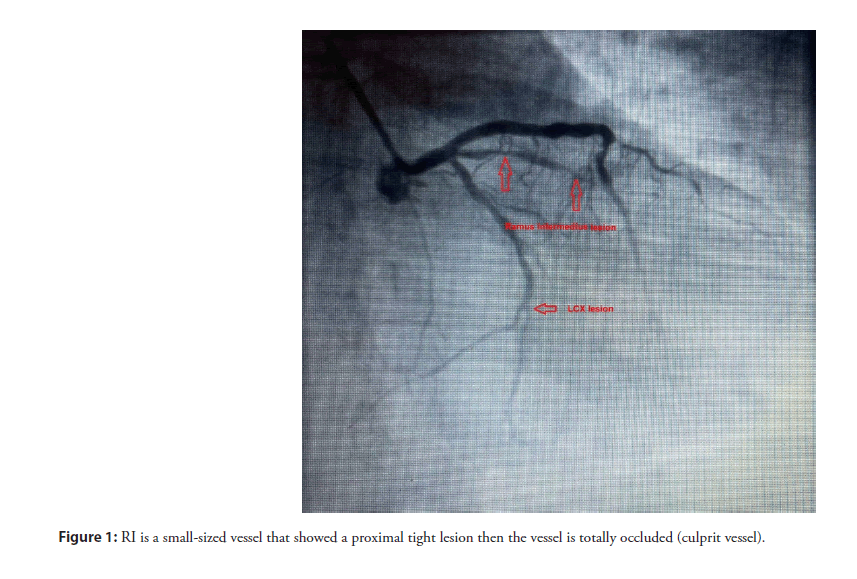
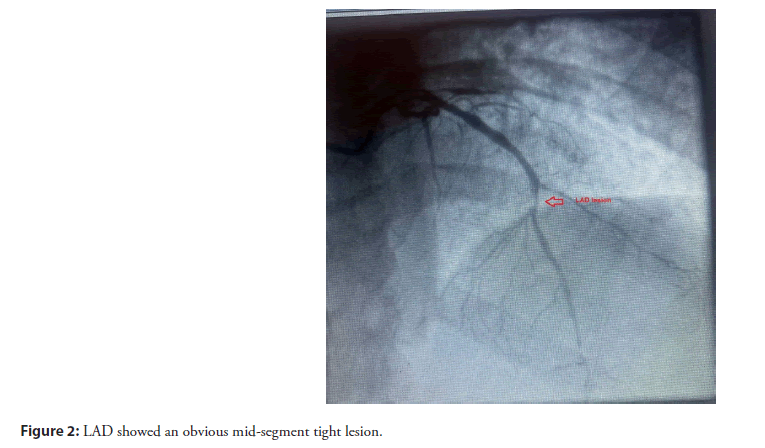
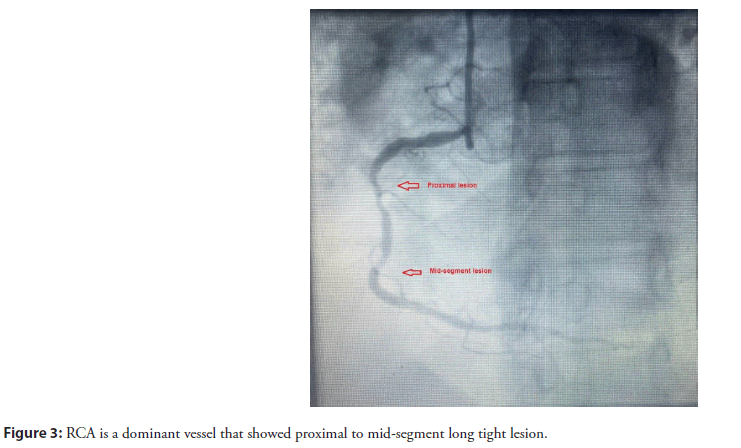
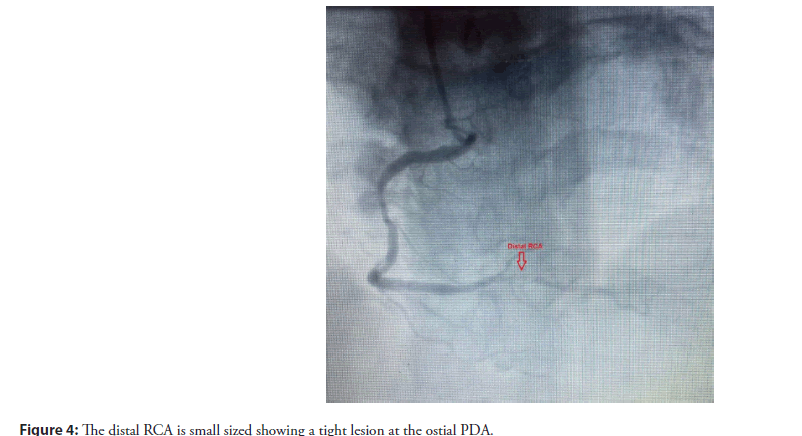
The coronary angiography was done using a trans-radial approach and revealed that LM had an average size and trifurcated into the LAD, RI and LCX arteries without any significant lesions. RI is a small-sized vessel that showed a proximal tight lesion then the vessel is totally occluded (culprit vessel) (Figure 1). Also, LCX is a small-sized vessel that showed a mid-segment lesion. LAD showed an obvious mid-segment tight lesion (Figure 2). Similarly, RCA is a dominant vessel that showed proximal to mid-segment long tight lesions (Figure 3). The distal RCA is small-sized showing a tight lesion at the ostial PDA (Figure 4).
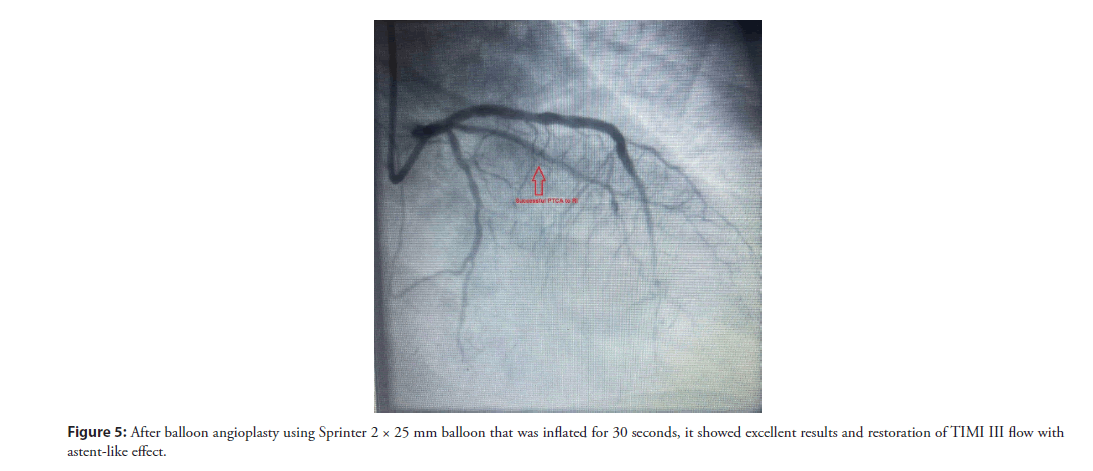
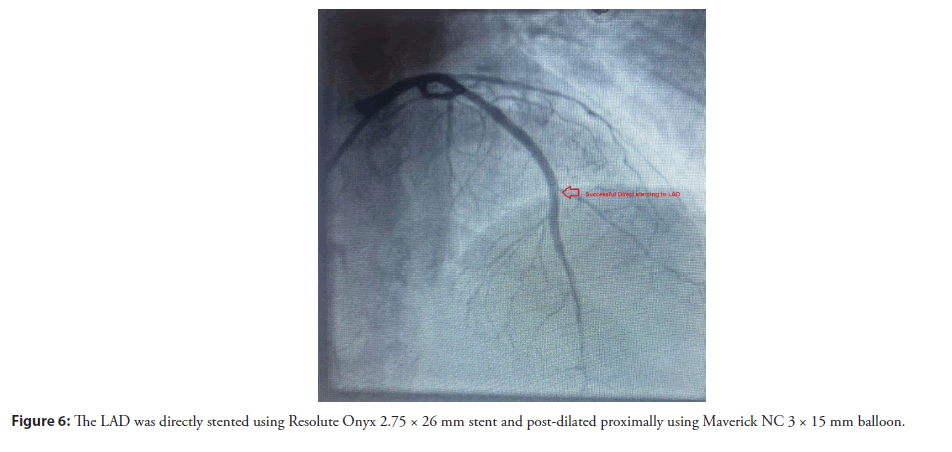
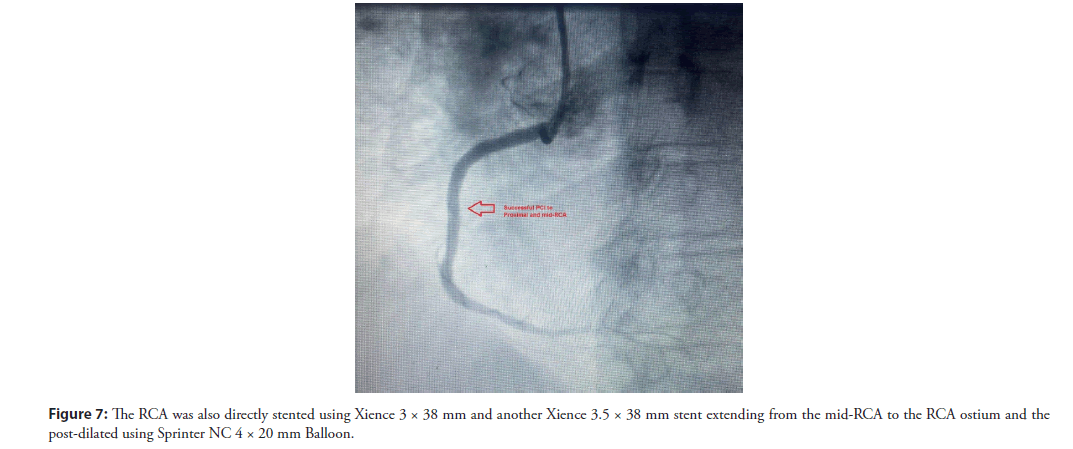
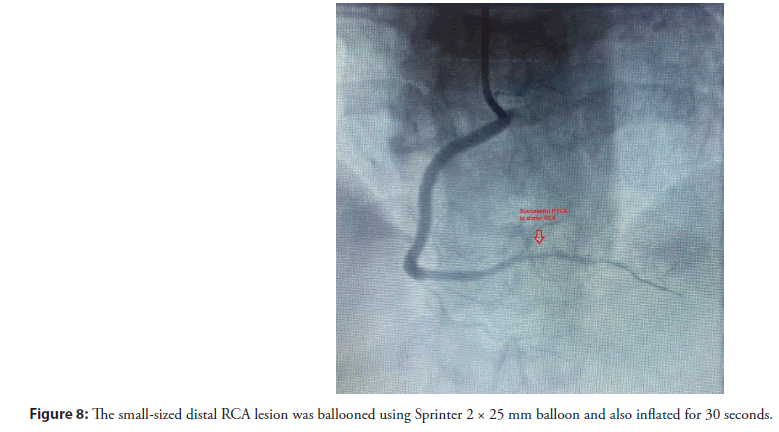
The patient underwent urgent primary coronary angioplasty. The decision was to do balloon angioplasty to RI total occlusion and then assess its size and see if stenting is possible or not. After balloon angioplasty using Sprinter 2 × 25 mm balloon that was inflated for 30 seconds, it showed excellent results and restoration of TIMI III flow with stent-like effect (Figure 5). The LAD was directly stented using Resolute Onyx 2.75 × 26 mm stent and post-dilated proximally using Maverick NC 3 × 15 mm balloon (Figure 6). The RCA was also directly stented using Xience 3 × 38 mm and another Xience 3.5 × 38 mm stent extending from the mid-RCA to the RCA ostium and the post-dilated using Sprinter NC 4 × 20 mm Balloon. The small-sized distal RCA lesion was ballooned using Sprinter 2 × 25 mm balloon and also inflated for 30 seconds.
Finally, the patient left the catheter lab with Thrombolysis in Myocardial Infarction-Grade III (TIMI III) flow and no chest pain (Figures 6-8).
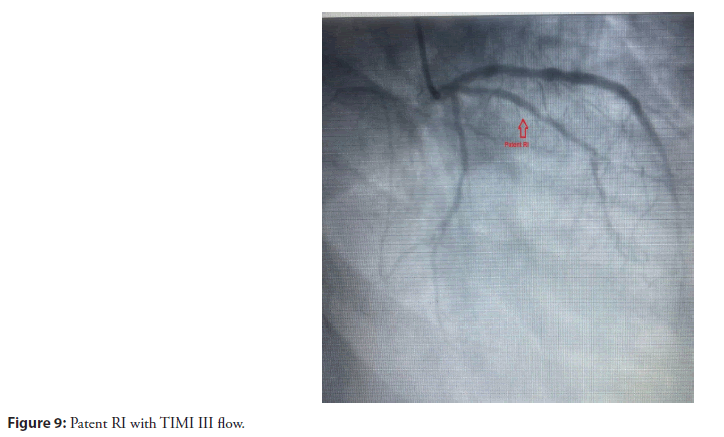
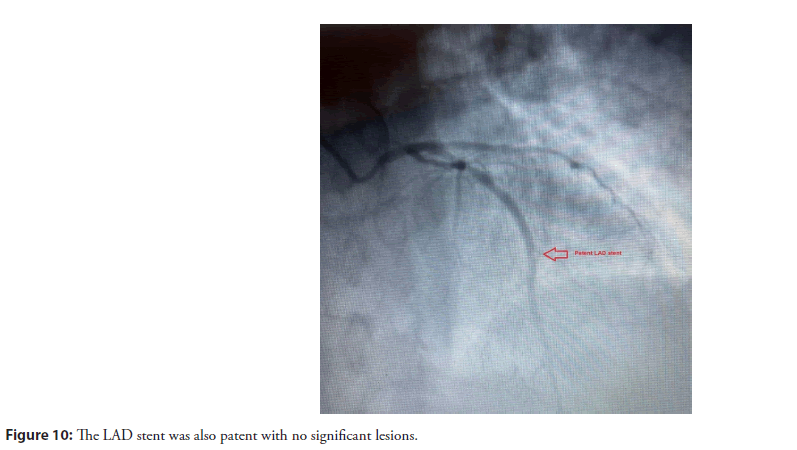
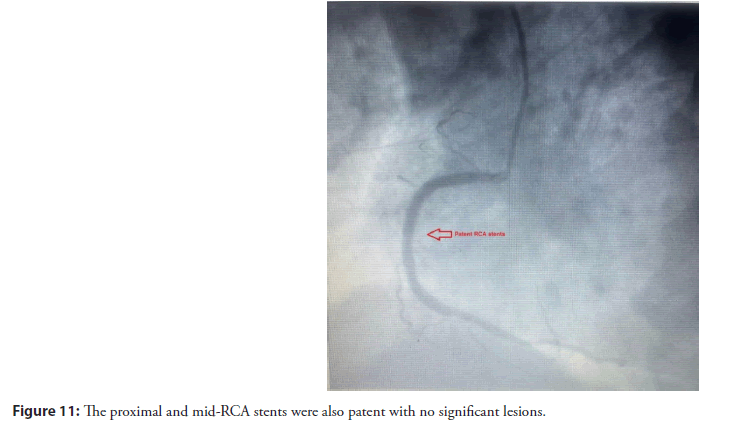
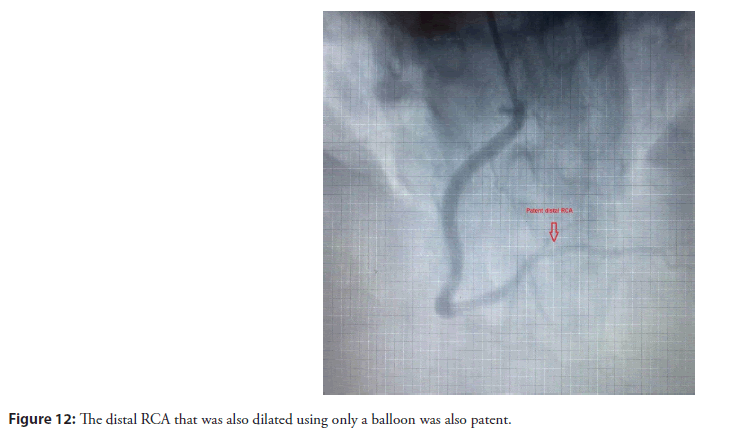
The patient was followed up for 2 years with strict anti-ischemic treatment and strict anti-diabetic measures to prevent the progression of atherosclerosis and avoid restenosis. But, despite that, she started to suffer from shortness of breath on exertion. The decision was to do a follow-up angiogram for her. The follow-up coronary angiogram showed patent RI with TIMI III flow (Figure 9). The LAD stent was also patent with no significant lesions (Figure 10). The proximal and mid-RCA stents were also patent with no significant lesions (Figure 11). The distal RCA that was also dilated using only a balloon was also patent (Figure 12).
Results and Discussion
PCI has undergone significant advancements in recent years, with the DES and BVS. However, in certain clinical scenarios, particularly in Small Vessel Coronary Artery Disease (SVD-CAD), PBA may still have a role to play. This case report aims to highlight the potential benefits of PBA in the management of SVD-CAD and encourage further discussion among cardiovascular specialists.
PBA, also known as plain old balloon angioplasty, was the first percutaneous revascularization technique introduced in the late 1970s [6]. While DES and BVS have become the standard of care for most coronary lesions, their use in small vessels (≤ 2.5 mm) remains controversial due to the increased risk of stent thrombosis, restenosis, and impaired vascular healing. PBA, on the other hand, avoids the potential complications associated with permanent or temporary implants, while still achieving adequate revascularization in selected cases [7].
Several studies have demonstrated favorable outcomes with PBA in SVD-CAD. The BARI trial reported similar long-term survival rates between PBA and CABG in patients with SVD-CAD [8]. Additionally, the BESMART (Bare-metal Stent vs. PBA for Small Vessel Coronary Artery Disease) trial showed no significant difference in Major Adverse Cardiac Events (MACE) between PBA and BMS implantation in small vessels at two-year follow-up [9].
However, it is crucial to carefully select patients who may benefit from PBA. Factors such as lesion characteristics (focal, noncalcified, and non-ostial), vessel size, and clinical presentation should be taken into consideration. Additionally, proper lesion preparation and adequate balloon sizing are essential for successful PBA outcomes [10].
Conclusion
In carefully selected cases of SVD-CAD, PBA may offer a viable treatment option, particularly when the risks associated with permanent or temporary implants outweigh the potential benefits. This case report serves as a reminder that while technological advancements are essential, traditional techniques like PBA should not be overlooked in the armamentarium of interventional cardiologists. A tailored approach, considering patient and lesion characteristics, is paramount in achieving optimal clinical outcomes.
Limitations and Future Perspectives
While this case report highlights the potential role of PBA in SVD-CAD, it is important to acknowledge its limitations as it represents a single case experience, and larger prospective studies are needed to validate the findings. Future research should focus on identifying specific subgroups of patients with SVD-CAD who may benefit most from PBA, as well as exploring potential adjunctive therapies (e.g., drug-coated balloons, and intravascular imaging guidance) to enhance procedural outcomes. Additionally, the development of dedicated small-vessel stent platforms with improved deliverability and conformability may further expand the treatment options for this challenging patient population.
References
- Koźlik M, Harpula J, Chuchra PJ, et al. Drug-eluting stents: Technical and clinical progress. Biomimetics (Basel). 8(1):72 (2023).
[CrossRef] [Google Scholar] [PubMed]
- Wybraniec MT, BaÅka P, Bochenek T, et al. Small vessel coronary artery disease: How small can we go with myocardial revascularization? Cardiol J. 28(5):767-778 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Chaivanit T, Chaivanit P, Bumrungrachapukdee P, et al. Comparison of primary patency rate between drug-coated balloon and plain balloon angioplasty in hemodialysis access. Siriraj Med J. 74:388-3894 (2022).
- Matsukawa R, Kozai T, Tokutome M, et al. Plaque modification using a cutting balloon is more effective for stenting of heavily calcified lesion than other scoring balloons. Cardiovasc Interv Ther. 34(4):325-334 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Bonaventura K, Leber AW, Sohns C, et al. Cost-effectiveness of paclitaxel-coated balloon angioplasty and paclitaxel-eluting stent implantation for treatment of coronary in-stent restenosis in patients with stable coronary artery disease. Clin Res Cardiol. 101(7):573-584 (2012).
[CrossRef] [Google Scholar] [PubMed]
- Barton M, Grüntzig J, Husmann M, et al. Balloon angioplasty-the legacy of andreas grüntzig, M.D. (1939-1985). Front Cardiovasc Med. 1:15 (2014).
[CrossRef] [Google Scholar] [PubMed]
- Jeżewski MP, Kubisa MJ, Eyileten C, et al. Bioresorbable vascular scaffolds-dead end or still a rough diamond? J Clin Med. 8(12):2167 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Hueb WA, Soares PR, Almeida de Oliveira S, et al. Five-year follow-op of the Medicine, Angioplasty, or Surgery Study (MASS): A prospective, randomized trial of medical therapy, balloon angioplasty, or bypass surgery for single proximal left anterior descending coronary artery stenosis. Circulation. 100:Ii107- Ii113 (1999).
[CrossRef] [Google Scholar] [PubMed]
- Agostoni P, Biondi-Zoccai GG, Gasparini GL, et al. Is bare-metal stenting superior to balloon angioplasty for small vessel coronary artery disease? Evidence from a meta-analysis of randomized trials. Eur Heart J. 26(9):881-889 (2005).
- Giannini F, Khokhar AA, Albani S, et al. Percutaneous intervention in small-vessel coronary disease: Time to clear the fog? JACC Cardiovasc Interv. 13(7):805-807 (2020).
[CrossRef] [Google Scholar] [PubMed]