Case Report - Interventional Cardiology (2022) Volume 14, Issue 0
Pericardectomy for constrictive pericarditis due to melioidosis
- Corresponding Author:
- Tiefenbacher CP
Abt Innere I, Kardiologie,
Marienhospital Wesel,
Pastor Janßenstrasse 8-38,
46483,
Wesel, Germany,
E-mail: christiane.tiefenbacher@prohomine.de
Received date: 17-Feb-2022, Manuscript No. FMIC-22-54801; Editor assigned: 21-Feb-2022, PreQC No. FMIC-22-54801 (PQ); Reviewed date: 28-Feb-2022, QC No. FMIC-22-54801; Revised date: 07-Mar-2022, Manuscript No. FMIC-22-54801 (R); Published date: 14-Mar-2022, DOI: 10.37532/1755-5310.2022.14(s8).194
Abstract
Here we report an interesting case of a patient with pericardial effusion due to melioidosis-to our knowledge the first case so far described in Germany. Despite of adequate antibiotic treatment, the patient deteriorated continuously and finally developed constrictive pericarditis so that pericardectomy had to be performed twice. In the end, the patient could be discharged in stable clinical condition. In the following, background and current knowledge of the infectious disease as well as available literature are discussed.
Keywords
Pericardial effusion • Melioidosis • Pericardectomy • Antibiotic treatment
Introduction
Melioidosis, or Whitmore’s disease (in German “Pseudorotz”), is an infectious disease with a potentially poor prognosis that can affect humans or animals. The disease is caused by the bacterium Burkholderia pseudomallei [1,2] which has been classified as a Category B biological weapons agent by the Center for Disease Control (CDC) and has been used as such for example in the first world war [3]. It is endemic in tropical climates, especially in Southeast Asia and northern Australia. The bacteria causing melioidosis are found in contaminated water and soil as well as on fruits and vegetables. It is spread to humans and animals through direct contact with the contaminated source, preferably via superficial skin lesions. Human-to-human transmission is very rare [3]. The incubation period usually ranges from one to twenty one days, but can eventually be as long as 20 years. Melioidosis has a wide range of signs and symptoms that can be mistaken for other diseases such as tuberculosis or more common forms of pneumonia. Apart from humans, melioidosis is found in a wide range of animals. The rare cases in the Western industrialized countries most often occur in travelers or immigrants [3]..
Case Presentation
We treated a 64 year old patient who was admitted for increasing cardiac congestion with pleural and pericardial effusion (Figure 1). The patient had been healthy so far, he was not on any medication. Blood tests showed increased levels of proBNP (3197 pg/ml), troponin T (263 ng/ml), and inflammatory markers as well as liver enzymes. Pleuracentesis as well as pericardiocentesis (1.5 l) were performed. Initially, bacteriological and cytological tests did not show a specific pathology. Daily, about 100 ml of fluid were aspirated from the pericardial space and in the course of the hospital stay, bacteria from the Burkholderia mallei/pseudomallei group were found. Material was sent for further testing to the reference lab, institution for microbiology, Bundeswehr/München which confirmed via molecular biology (realtime PCR, target genes fliC und 16S-SNP) the finding of an infection with Burkholderia pseudomallei.
Our patient reported that he had been in Thailand in 2013 for three weeks, visiting family in a rural area. Due to sunburn on his feet, he had open skin lesions when walking barefoot through some rice fields. After his return to Germany, there were no specific health problems. Five years later, in spring 2018, he was suffering from recurrent fevers up 40áµC every two to three days over several weeks. He did not see a doctor at that point and the fever disappeared. In 2020, again, fever occurred up to 39áµC and additionally, he was suffering from chest pain and chills. His family practitioner started an antibiotic therapy with cefuroxime. For ongoing fever, he was admitted to the hospital.
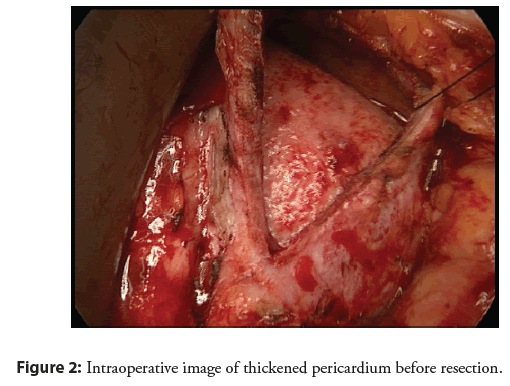
After diagnosis, the patient has been isolated and treated with adequate antibiotic therapy. Clinically, there was continuous improvement and inflammatory markers were regredient. Via CT, there was suspicion for hepatic manifestation with multiple small lesions within the liver. The patient was discharged in clinically stable condition with continued treatment with trimethoprimsulfamethoxazole for 20 weeks. After ten days, the patient was again admitted to the hospital for increasing dyspnea with pleural and pericardial effusion as well as ascites. Again, a pericardial drainage had to be performed finding B. pseudomallei in the pericardial fluid. Antibiotic therapy was continued, but due to worsening renal and hepatic function, antibiotic treatment had to be stopped. Diuretic therapy had been intensified, but the patient could not be stabilized so that hemofiltration was initiated on the intensive care unit. Due to increasing organization of the pericardial fluid with fibrous deposits, we started an experimental approach with fibrinolytic therapy via instillation of urokinase and alteplase intrapericardially without improvement. A pericardectomy was discussed with the heart surgeons. Preoperatively, obstructive coronary artery disease was ruled out by coronary angiogram. Via intracardial pressure monitoring, a typical picture of constrictive pericarditis was found with identical end diastolic pressure values in left and right ventricle. Due to clinical deterioration, partial pericardectomy was performed. Intraoperatively, heavy calcareous shells had to be removed (Figure 2). A reoperation with additive inferior pericardectomy was necessary due to the development of a large encapsulated pericardial effusion with partial compression of the right and left ventricle. Antibiotic treatment with ceftazidime intravenously was continued. Under ongoing intensive diuretic therapy, both patient and renal function slowly improved. Echocardiographically, the presence of pericardial effusion was ruled out. Left ventricular function was slightly decreased. Inflammatory markers improved and remained near normal. The patient could be discharged in good clinical condition. A rehabilitation measure was initiated. Continuation of antibiotic treatment with doxycycline 200 mg bid was recommended until March 2021.
Results and Discussion
An infection with B. pseudomallei can be asymptomatic over a long time [2,3]. About 90% of infected patients are acutely ill, 10% show a chronic course of the disease. Recurrencies can occur after many years. Dependent on the way of infection, symptoms can vary from localized Infection to pulmonary Infection, bloodstream infection or disseminated infection with poor prognosis. There can be formations of granuloma in liver, spleen, lymph nodes and bones. Although healthy people may also get melioidosis, there are risk factors such as diabetes or chronic disease of the lung, liver or kidney.
The diagnosis of melioidosis and detection of B. pseudomallei in the lab is challenging. Diagnostic tools include:
(1) Cultivation and identification in sputum, blood, and deductions
(2) Examination of preparations by light microscopy after staining with methylenblue
(3) Determination of specific antibodies.
Treatment generally starts with intravenous antimicrobial therapy with a combination of ceftazidime and cotrimoxazole for ten to fourteen days (alternatively carbapenems such as imipenem or meropenem), followed by three to six months of oral antimicrobial therapy with cotrimoxazole, trimethoprim-sulfamethoxazole or amoxicillin/clavulanic acid [3,4].
In a prospective trial in North Australia over ten years [5], 252 patients with melioidosis were described and characterized. 46% of the patients had a bacteremia, 19% died. Patients with septic shock had a very high mortality (86%) despite adequate antibiotic treatment. 50% of the patients had a pneumonia, 15% urogenital infections, 18% abscess of the prostate. Rare manifestations were abscesses of the skin (13%), osteomyelitis and/or septic arthritis (4%), abscesses of the soft tissue (4%), and encephalomyelitis (4%). 37% of patients had risk factors including excessive alcohol consumption (39%), chronic pulmonary disease (27%), and chronic kidney disease (10%). Only one patient without risk factors died. Antibiotic therapy decreased mortality. Cardiac manifestations have not been described in this trial.
systematic literature search in 2019 (PubMed/Web of Science) with respect to melioidosis cases in Europe between 2000-2018 reports 77 cases of imported melioidosis [6], mostly in men (73%) and following a stay in Thailand for less than four weeks (53%). Treatment in a hospital occurred mostly within the first four weeks after returning home (58%). There were less comorbidities than usually present in patients with melioidosis (16%, mostly diabetes in 19%). Clinical presentation was heterogenous: most frequently, there was pneumonia (52%), cardiovascular manifestations (45%) and alterations of skin and soft tissue (35%). The diagnosis was most frequently obtained by culture (92%), supported by morphological, biochemical and molecular tests (23%). False diagnosis was frequent (21%). More than half of the patients were treated adequately (56%). Mortality in this cohort was lower than usually described (6%).
Pericardial manifestation of melioidosis is rare (about 1%) [6]. Only a few cases have been reported in the literature [7,8], to our best knowledge none so far in Germany. The course of disease is mostly subacute or chronic and difficult to differentiate from pericarditis in tuberculosis. In a retrospective trial over ten years in Thailand from 2010 [7], patients with pericarditis and pericardial effusion due to melioidosis (n=12) or tuberculosis (n=33) were analyzed. In contrast to patients with tuberculous pericarditis, the causative pathogen could be established in the pericardial fluid of nine patients with pericarditis due to melioidosis. Histologically, there was a picture of subacute to chronic fibrinous pericarditis. Ten patients developed constrictive pericarditis; nine of them were treated via surgical pericardectomy in the course of the disease.
Conclusion
The authors therefore recommend consequent drainage and removal of the pericardial effusion to prevent development of constrictive pericarditis. However, it is unclear if constrictive pericarditis can be prevented by prolonged pericardial drainage.We here describe an unusual clinical case of a patient with pericardial effusion due to melioidosis acquired in Thailand 20 years ago. Only after prolonged antibiotic treatment and pericardectomy could the patient be stabilized and finally be discharged.
References
- Whitmore A, Krishnaswami CS. An account of the discovery of a hitherto undescribed infective disease occurring among the population of Rangoon. Ind Med Gaz. 47(7): 262-267 (1912).
[Google Scholar] [Pubmed]
- Göbel K, Teichmann D, Richter J, et al. Diagnose: Melioidose. Dtsch Arztebl. 102(31-32): A-2166/B-1826/C-1729 (2005).
- RKI: Melioidose. Biologische Gefahren II
- Lipsitz R, Garges S, Aurigemma R, et al. Workshop on treatment of and postexposure prophylaxis for Burholderia pseudomallei and B. mallei infection, 2010. Emerg Infect Dis. 18(12): e2 (2010).
[CrossRef] [Google Scholar] [Pubmed]
- Currie BJ, Fisher DA, Howard DM, et al. Endemic melioidosis in tropical northern Australia: A 10-year prospective study and review of the literature. Clin Infect Dis. 31(4): 981-986 (2000).
[CrossRef] [Google Scholar] [Pubmed]
- Le Tohic S, Montana M, Koch L, et al. A review of melioidosis cases imported into Europe. Eur J Clin Microbiol Infect Dis. 38(8):1395-1408 (2019).
[CrossRef] [Google Scholar] [Pubmed]
- Chetchotisakd P, Kaen K, Anunnatsiri S. Melioidosis pericarditis mimicking tuberculous pericarditis. Clin Infect Dis. 51(5) e46-e49 (2010).
[CrossRef] [Google Scholar] [Pubmed]
- Raff MJ, Lamkin N Jr, Braun J, et al. Melioidosis complicated by pericarditis. Chest. 69(2): 227-229 (1976).
[CrossRef] [Google Scholar] [Pubmed]