Short Communication - Interventional Cardiology (2025) Volume 17, Issue 2
Isolated External Iliac Artery Aneurysms: Recognizing the Rare and Acting Early
- Corresponding Author:
- Patrick D. Conroy
Department of Vascular and Endovascular Surgery, Cooper University Hospital, Rowan University Medical School, Camden, United States of America
E-mail: patrickdconroy@gmail.com
Received date: 03-Mar-2025, Manuscript No. FMIC-25-165409; Editor assigned: 05-Mar-2025, PreQC No. FMIC-25-165409 (PQ); Reviewed date: 19-Mar-2025, QC No. FMIC-25-165409; Revised date: 26-Mar-2025, Manuscript No. FMIC-25-165409 (R); Published date: 05-Apr-2025, DOI: 10.37532/1755-5310.2025.17(2).976
Abstract
Isolated External Iliac Artery (EIA) aneurysms are exceptionally rare vascular anomalies, often discovered incidentally and lacking clear management guidelines. In this study, we present a case of an asymptomatic 68-year-old man with a true isolated EIA aneurysm successfully treated with endovascular repair using a Viabahn stent graft. We discuss the diagnostic challenges, rationale for early intervention, and procedural considerations unique to this vascular territory. This case highlights the importance of maintaining a high index of suspicion, leveraging incidental imaging findings, and considering endovascular options in anatomically suitable patients. We also emphasize the urgent need for data registries to inform future clinical practice and guideline development.
Keywords
EIA aneurysm . Endovascular . Asymptomatic . Stent graft . Stent compression
Description
The field of interventional vascular medicine often advances through the study of common pathologies abdominal aortic aneurysms, femoropopliteal disease, carotid stenosis but every now and then, we’re reminded that uncommon presentations can be just as critical, especially when they slip beneath the diagnostic radar. Our recently published case in JVS-CIT described a 68-year-old man with an incidentally discovered, EIA aneurysm, asymptomatic and without any evidence of systemic or segmental vascular disease [1]. Given the size and concern for risk of rupture, the decision was made to perform a preventative intervention. The lesion was successfully treated with endovascular repair using a Viabahn stent graft. This case offers a rare clinical scenario that challenges current guidelines and reinforces the need for individualized treatment strategies, particularly in anatomically and pathophysiologically uncommon presentations.
Generally, when treating pathologies of the external iliac artery, an open procedure is the gold standard. Endovascular interventions are typically avoided given the risk of compression between the inguinal ligament and the bony structures of the hip and pelvis [2]. After extensive discussions of risks and benefits with the patient, he was adamant to avoid an incision associated with an open procedure and elected to undergo minimally invasive endovascular repair of his EIA aneurysm. Due to the high mobility of the vessel and the risk of compression, a self-expanding stent graft was the best choice for treatment. Pre-procedural imaging confirmed an adequate distal landing zone in the common femoral artery, and the patient's relatively preserved arterial compliance further supported the feasibility of an endovascular approach.
Though iliac artery aneurysms are generally thought of as common, isolated iliac artery aneurysms are rare (estimated at <0.03% incidence) [3], the majority involve the common iliac artery and are often associated with aortic aneurysms or generalized atherosclerosis. In contrast, true isolated aneurysms of the external iliac artery are almost unheard of, with fewer than 10 cases clearly documented in the literature many of which were symptomatic, ruptured, or associated with cystic medial necrosis [4-10]. Moreover, there appears to be no consensus on screening strategies for patients at potential risk, as most cases, including ours, are diagnosed serendipitously.
This case stands out for multiple reasons:
• The patient was completely asymptomatic.
• There was no concomitant vascular pathology, no trauma, no prior access, no inflammatory markers, and no relevant family history.
• The aneurysm was found on routine MRI done for an elevated Prostate-Specific Antigen (PSA), emphasizing how nonvascular imaging may be the only window of opportunity to detect such silent lesions.
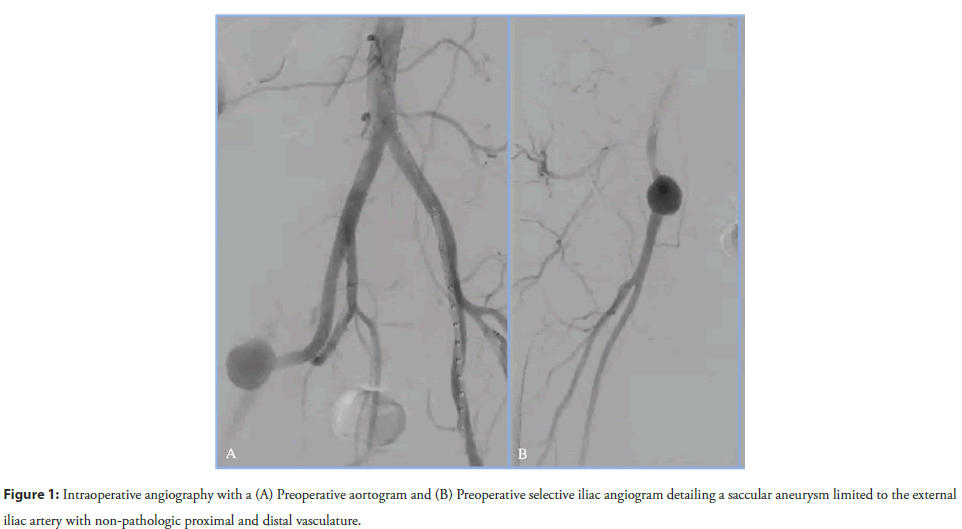
The pathology's rarity raises diagnostic and management questions. When should we intervene? Current vascular guidelines provide aneurysm size thresholds for repair of common and internal iliac aneurysms [11], but none specifically address isolated EIA aneurysms. In our literature review, the majority of reported isolated EIA aneurysms were repaired at diameters of 2 cm-4 cm, with most patients being male and in their sixth decade of life. Given the risk of rupture reported as high as 75% in some older studies and the often insidious course until that catastrophic event we argue for early elective repair of isolated EIA aneurysms =2 cm, especially when the anatomy is favorable for endovascular treatment [12]. While some might consider watchful waiting in asymptomatic patients, we believe the potential morbidity and mortality associated with rupture justifies a more proactive stance, particularly in fit individuals with suitable anatomy (Figure 1).
Figure 1: Intraoperative angiography with a (A) Preoperative aortogram and (B) Preoperative selective iliac angiogram detailing a saccular aneurysm limited to the external
Histologically, the EIA’s unique lamellar and elastin-rich media may explain its resistance to aneurysmal degeneration compared to the rest of the iliac system, which makes its failure all the more intriguing when it does occur [13]. Inflammatory, genetic, or mechanical stressors remain speculative etiologies in most of these idiopathic cases [14]. Until we have large-cohort data or registrydriven studies, clinical vigilance and individual judgment remain paramount. Further investigation into potential biomarkers or connective tissue disorders may help elucidate underlying mechanisms in future cases.
From a procedural perspective, this case underscores the value of endovascular techniques in managing aneurysms in anatomically challenging or traditionally surgical zones. Using careful preoperative planning, a percutaneous, contralateral transfemoral approach allowed for successful exclusion of the aneurysm with preservation of distal perfusion and minimal morbidity. The patient was discharged the same day, and follow-up imaging confirmed durable exclusion without endoleak. This rapid recovery and positive mid-term outcome underscore the growing role of minimally invasive options in scenarios previously dominated by open surgical repair, though long term follow-up should elucidate if this is a durable option given the risk of stent compression.
In an era where device options and imaging modalities continue to evolve, we believe this case supports expanding the interventionalist’s awareness of isolated EIA aneurysms, not just as academic curiosities but as real, actionable pathologies. When encountered, even incidentally, they warrant deliberate evaluation and likely early repair, given their potential for sudden deterioration. Education and awareness among both vascular specialists and general practitioners are essential to ensuring that rare but serious conditions like this are not missed or undertreated. This case also highlights an opportunity: the need for a multiinstitutional registry or case series to gather more data on true isolated iliac aneurysms. Until then, each case report builds the bridge between mystery and evidence.
References
- Conroy PD, Li J, Hamdan A, et al. Isolated external iliac artery aneurysm in a patient without any concomitant vascular disease. J Vasc Surg Cases Innov Tech. 11(1):101682 (2025).
- Schanzer A, Belkin M. Direct surgical repair of aneurysms of the infrarenal abdominal aorta and iliac arteries. Atlas of vascular surgery and endovascular therapy. Anatomy and technique. Philadelphia, PA: Elsevier Saunders. 2014.
- Brunkwall J, Hauksson H, Bengtsson H, et al. Solitary aneurysms of the iliac arterial system: An estimate of their frequency of occurrence. J Vasc Surg. 10(4):381-384 (1989).
- Priddle HD. Rupture of an aneurysm of the left external iliac artery during pregnancy. Am J Obstet Gynecol. 63(2):461-463 (1952).
- Crivello MS, Porter DH, Kim D, et al. Isolated external iliac artery aneurysm secondary to cystic medial necrosis. Cardiovasc Intervent Radiol. 9:139-141 (1986).
- Mohan IV, Adam DJ, Kurian KM, et al. Isolated external iliac aneurysm associated with hyperhomocysteinaemia. Eur J Vasc Endovasc Surg.14(6):506-508 (1997).
- Kato T, Takagi H, Kawai N, et al. Ruptured isolated external iliac artery true aneurysm associated with cystic medial necrosis: Report of a case. Surg Today.39(8):705-709 (2009).
- van de Luijtgaarden KM, Brehm V. External iliac artery aneurysm causing severe venous obstruction. Eur J Vasc Endovasc Surg. 57(5):739 (2019).
- Hussain AS, Aziz A. Giant external iliac artery aneurysm. Ann Vasc Surg 58:386.e1-386.e3 (2019).
- Chatzantonis G, Schmoll L, Strübing F, et al. A surprising diagnosis in a young patient with intermittent claudication: Symptomatic isolated external iliac artery aneurysm associated with cystic media necrosis. J Vasc Surg Cases Innov Tech. 6(3):352-356 (2020).
- Wanhainen A, Van Herzeele I, Goncalves FB, et al. Editor's choice--European Society for Vascular Surgery (ESVS) 2024 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 67(2):192-331 (2024).
- Schuler J, Flanigan D. Iliac Artery Aneurysms.1982.
- Tang GL, Kohler TR. Chapter 3: Anatomy, Physiology, and pharmacology of the vascular wall. In: Moore WS, editor.
- Garland HG. The pathology of aneurysm: A review of 167 autopsies. J Pathol Bacteriol. 35(3):333-350 (1932).