Research Article - Clinical Practice (2020) Volume 17, Issue 4
Impact of COVID-19 pandemic on orthopedic practice-Results of a survey from a Covid hotspot in India
Abstract
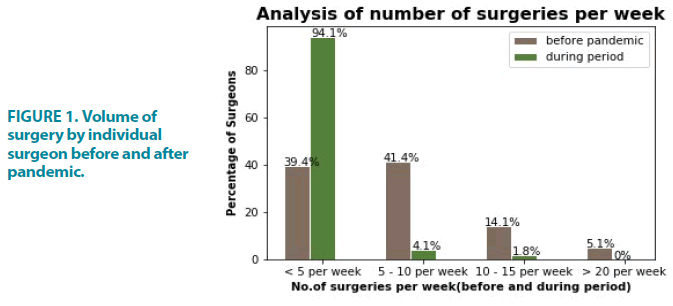
Introduction: COVID-19 pandemic has drastically affected medical practice including the specialty of Orthopedics. This study aims to analyze and quantify its actual impact on practice amongst the orthopedic Surgeons in Chennai. Materials and Methods: We did an online survey among the practicing orthopedic surgeons in Chennai. A questionnaire to assess pre-COVID and post-COVID quantum of practice, with a time frame between 23rd of March 2020 and 31st of May 2020, was done and analyzed. Results: 101 orthopedic surgeons participated in this survey with a response rate of 15%. Senior surgeons comprised the major share-45.5% of the participants of this survey. Among the surgeons who participated in the survey, 49.5% of them declared that their Outpatient practice during this pandemic dropped by more than 75%. The percentage of surgeons who operated <5 cases per week before pandemic was 39.4%, which rose to 94.1% during the pandemic. Though 76.2% of the surgeons continued to attend trauma cases during the pandemic with risk involved none of the surgeons became COVID positive during study period. Discussion: Chennai became a COVID-19 hotspot and its impact was evident in various spheres of orthopedic practice. Health manpower management underwent drastic change to adapt to the new challenges put forth. Injury and orthopedic case demographics had a major shift towards domestic injuries and geriatric health care seekers approaching hospitals. RTA’s reduced in number. OP and OR case volume during pandemic were reduced significantly in comparison to pre-COVID times showing the quantum of COVID-19 impact.
Keywords
Sars-Cov-2, COVID-19, orthopedic practice, pandemic
Introduction
In this era of technological renaissance AI was dictating terms, robotics was entering every sphere, navigation was already mastered, newer techniques and high end innovations were ruling the roost, from conventional methods all specialties widened its spectrum to sub specialties and hyper specialties.
The unprecedented bio danger, namely COVID-19, brought the world to a standstill, an uneasy calm of fear and fright engulfed the human race turning the world upside down. The invisible femtograms of Sars-Cov-2 exposed the ill prepared world to pandemic situations taking us all for a bizarre roller coaster ride into a world of uncertain future. COVID-19 drastically affected medical practice without doubt; the scenario in the orthopedic field is no exception being pushed into a state of hibernation with dormant redundancy.
Materials and Methods
We planned for a descriptive study to analyze the impact of COVID-19 pandemic on the orthopedic practice of surgeons in the metropolitan city of Chennai. An online survey among the practicing members of Madras Orthopedic Society, the official conglomeration of orthopedic surgeons of Chennai was done. A questionnaire comprising 25 questions (annexure1) was formulated using Google forms and was circulated among the members using the official Whatsapp group of this society. The questions were prepared in such a way that pre- COVID and post-COVID quantum of practice were compared and analyzed. The questions in the survey were drafted and answered based on a time frame between 23rd of March 2020 and 31st of May 2020. Participation in this survey was purely voluntary. Since this study did not involve care of patients, the need for clearance from the institutional ethical committee was unnecessary and henceforth not obtained. The survey responses were exported to spreadsheet format and statistical analysis was done using Python program in Spyder software version 4.1.3, to arrive at the results. The confidentiality of our respondents is maintained strictly.
Results
A total of 101 orthopedic surgeons participated in this survey with a response rate of 15% (Total number of members 670). The average age of the members was 44 years with a range from 30-66 years. Senior surgeons comprised the major share 45.5% of the participants of this survey. Institution affiliation stood at 51% for teaching institutions, 21% working in corporate hospitals and 28% owned their private clinic or hospital set up. With regards to job description 47.5% comprised Assistant professors/Consultants, 34.7% came under the category of senior consultants/Associate professors and 17.8% were Professors. Among the participants, the majority were involved in care of trauma patients. Arthroplasty was the subspecialty which majority of the participants opted for followed by Spine and Arthroscopy. There has been overlap of specialties with exclusive specialties being pediatric surgery and spine.
23.8% of the participants did not participate in care of trauma cases after the onset of pandemic and the remaining continued in attending trauma cases. The age group distribution of trauma cases during this pandemic arrived at 57.42% comprising of Geriatric population, 30.69% involving the middle age group, with young adults and pediatric trauma forming the remaining cases. Among trauma attended during pandemic, hip fractures were the most common followed by compound injuries. Among the 101 surgeons who participated in the survey, 49.5% of them declared that their outpatient practice during this pandemic dropped by more than 75%. The stratification based on their job description is depicted in (TABLE 1).
| Job affiliation | Nos | Percentage drop of OP practice | |||
|---|---|---|---|---|---|
| >75% | 50%-75% | 25%-50% | <25% | ||
| Assistant Prof/Consultants | 48 | 23 | 16 | 6 | 3 |
| Associate Prof/Senior consultants | 35 | 16 | 13 | 2 | 4 |
| Professors | 18 | 11 | 2 | 4 | 1 |
TABLE 1. Reduction in OP practice stratified with job description.
Reduction of Orthopedic practice did not spare any type of institutional affiliation, which is evident from (TABLE 2). Members from teaching institutions (54.9% recorded drop of >75%) and corporate hospitals (52.3% recorded drop of >75%) seemed to be more affected by the pandemic, when compared to surgeons having private clinics (37.9% recorded drop of >75%).
| Percentage of drop of OP practice | |||||
|---|---|---|---|---|---|
| Institution Affiliation | >75% | 50%-75% | 25%-50% | <25% | Total |
| Teaching Institution | 28 (52.3%) | 10 (19.6%) | 6 (11.7%) | 7 (13.7%) | 51 (100%) |
| Corporate Hospital | 11 (52.3%) | 9 (42.8%) | 1 (4.7%) | 0 | 21 (100%) |
| Private Clinic | 11 (37.9%) | 12 (41.3%) | 5 (17.2%) | 1 (4.4%) | 29 (100%) |
| Grand Total | 101 | ||||
Note: Percentage within each category expressed within brackets adjacent to actual numbers
TABLE 2. Reduction in OP practice categorized by institutional affiliations.
The reduction in volume of surgeries was also clearly evident as represented in (FIGURE 1). The percentage of surgeons who operated <5 cases per week before pandemic was 39.4%, which rose to 94.1% during the pandemic. Though 76.2% of the surgeons continued to attend trauma cases during the pandemic, all other elective surgeries including various orthopedic subspecialties were cancelled or postponed, leading to a drastic reduction in the total number of orthopedic surgeries.
FIGURE 1. Volume of surgery by individual surgeon before and after pandemic.
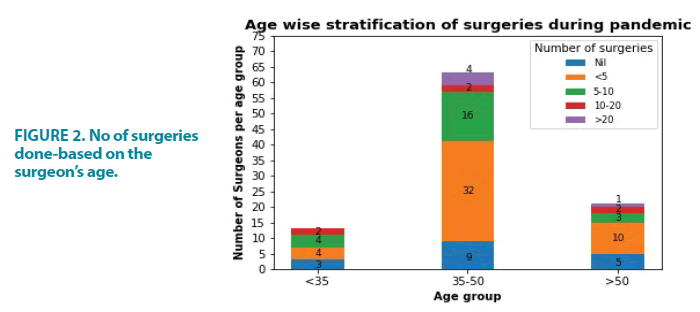
On the no of orthopedic surgeries done during the study period, 5.6% operated >20 cases, 6.7% operated on 10-20 cases, 25.6% operated about 5-10 cases, 54.4% had operated <5 cases and finally 7.8% never attended surgery during the study period. The age group between 35 to 50 years did most of the cases. This data is represented in (FIGURE 2).
The data indicated that the number of surgeries related to orthopedic subspecialties including arthroplasty, arthroscopy and spine surgeries fell drastically during the study period with >95% of surgeons operating <5 cases in the individual subspecialty during this period. The above data is represented in (TABLE 3).
| Subspecialty | Expressed as percentage of participant surgeons | ||||
| >20 surgeries | 10-20 surgeries | 5-10 surgeries | <5 surgeries | Nil | |
| Arthroplasty | 0 | 0 | 1.1 | 76.5 | 22.4 |
| Arthroscopy | 0 | 0 | 2.5 | 76.5 | 21 |
| Spine surgery | 0 | 0 | 1.2 | 78.8 | 20 |
| Others including trauma | 5.6 | 6.7 | 25.6 | 54.4 | 7.8 |
TABLE 3. Distribution of Orthopedic subspecialty surgeries.
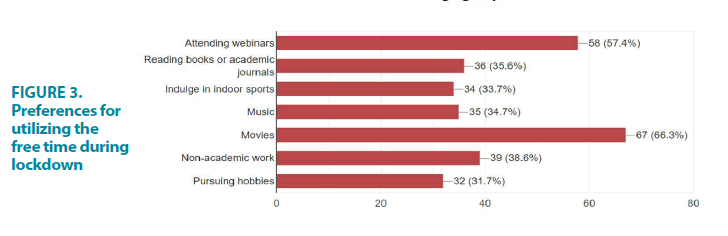
10.2% of surgeons reported that <10 patients they attended turned positive. Remaining surgeons reported that none of them nor their patients turned positive. Preferences in telemedicine among the participants were compiled and majority preferred video calls (61%) followed by Whatsapp chat (35%), third party telemedicine application providers (31%) and email communication (6%). The medium of information sharing and knowledge update for the participant surgeons stood at 68% choosing social media followed by Television 39%. Finally lockdown increased the free time of all surgeons and their preferences in utilizing this extra free time was also recorded and graphically represented in (FIGURE 3).
Discussion
Chennai is a metropolitan city in Southern India with the best medical infrastructure facilities and an established medical tourism hub. Orthopedic sector grew leaps and bounds, latest treatment is on offer in every subspecialty. Chennai being a COVID hotspot, an unexpected alteration in the dynamics of practice was witnessed by every medical specialty, orthopedics being no exception. The respondents in our study formed around 15% of the total population of orthopedic surgeons practicing in Chennai, which forms an appropriate sample to study the real impact, to precisely assess and diligently quantify the impact. Among the participants of our study group 72.9% had more than 10 years of practice. It is obvious that these seniors would have had excellent practice pre-COVID and collecting data from them will be a testimony of a clear picture of the actual impact. The impact in every aspect of Orthopedic practice is discussed.
■ Healthcare ergonomics
Hospitals divided the available doctors from all specialties, into three groups, with one third in quarantine, one third in COVID related duties and other third in department work. This obviously caused a major reduction in orthopedic related work. This was part of the Standard operating procedures issued by the Ministry of Health [1]. The shortage of staff in private clinics and corporate hospitals became unavoidable due to voluntary reduction of staff pattern, lack of transport facilities during lockdown, reduced income for hospitals needing to prune up the staff pattern.
■ Injury dynamics
The lockdown kept the public at home, drastically reducing RTA [2]. Domestic injuries continued to happen which was evident, as hip fractures were the commonest indication for surgery and geriatric population was the majority of patients seeking Orthopedic care. Though, not same in magnitude as pre-COVID times, compound injuries were the second most common injury. Screening for COVID-19 was done prior to surgery in accordance with prevalent guidelines [3].
■ OPD trends
The OP consultation suffered a major decline as per our respondents. 50% of our respondents practice reduced to a level of less than 75%. Most clinics were closed due to fear of contracting the disease and to avoid spread from their consultation areas. This definitely had a positive impact though, by the fact that none of our respondents contracted the disease. SOPs were not known initially for OP areas during the early phase of this pandemic. The advisory issued by the Indian Orthopedic association suggested restriction of OP practice [3]. There was a huge stress amongst the private practitioners, that their premises may be closed indefinitely, if any of the patients or staff contracted COVID-19. Safe OP practices like social distancing with visual cues, insisting on mask, temperature screening, regular fogging, making sanitizers available at strategic points, creating awareness amongst staff and providing them with masks and PPEs, were followed in most consultation areas.
■ (Non) surgical strike
Reversal of ratios were witnessed with 94.1% operating only less than 5 cases during a week’s time, which was 39.4% before COVID-19. None of our respondents could operate >20 cases per week. Respondents above 50 years of age had taken caution and operated a lesser number of cases. The brave-hearts who bore the brunt were between 35 to 50 years. This age group have risked their lives to alleviate the sufferings of the traumatized patients and simultaneously protect the senior colleagues from the risk of exposure.
Difficulties in manpower, optimization of available staff, lack of clear and definite knowledge on the theatre protocols, rationing of PPEs, increasing financial burden caused reduction in the number of cases. Experience from the past, that aerosol generating procedures in Orthopedics like drilling, reaming, pulse lavage, electrocautery added up to risks involved in operating on patients, also played on the minds of surgeons [4]. The efforts of all our colleagues who have been operating even during this hour of crisis deserves huge respect and they clearly are the frontline warriors fighting the pandemic.
Elective orthopedic surgeries were either postponed or cancelled in accordance with Government advisory and protocols issued by professional bodies [1,3]. 75% of our respondents operated less than 5 cases in spine, replacement and scopy surgeries. Around 20% did not operate at all and only 1 to 2% could carry out 5-10 cases in the entire period of study. Conservative management took an upper hand and most cases were treated with plaster of Paris splinting, as even casting was not advised anticipating increased frequency of visits [3].
■ Evolving strategies
To reduce physical contact, the need for an online platform for consultations has been well brought out by our respondents, with video calls being the desired choice of 60%, Whatsapp chat was chosen by 35%. Non visual forms like emails are not much preferred.
Most of our respondents had used PPE’s in accordance with the current guidelines [3,5,6]. None of our respondents have intimated that they contracted COVID-19 even though 2 of them had a COVID positive immediate family member. 10.2% of the respondents declared that they had treated patients who turned COVID positive during the treatment period. This shows they adhered to the safety guidelines and protected themselves effectively [1,3,4,6,7]. Implementation of guidelines recommending COVID testing of all patients posted for surgery, could be another reason for reduced incidence of infection among respondents [3,8,9]. The risk involved has been well quantified by Guo et al. from Wuhan, where the risk for orthopedic surgeons to get infected ranged from 1.5 to 20.7% [10].
■ Rekindling interests
With time aplenty, interests were reactivated and some freshly learnt. The talent in them resurfaced and to many it was a revelation that helped them tide over this phase of professional inactivity. The movie buffs were plenty with 67% enjoying the comfort of home and convenient time to indulge in movies. Webinars were offered on a platter, in all specialties and was willingly attended by 58%. In future, zoom meetings, online conferences may be the way to share knowledge. This period has definitely exposed most of our respondents to online platforms.
■ Study limitations
Very few publications have been reported from India analyzing the COVID-19 situation in Orthopedics [6,11,12]. We aimed only to quantify the impact of COVID-19 pandemic on orthopedic practice and we did not analyze or interpret any disease pattern, management protocol or practice guidelines.
Conclusion
COVID-19 is here to stay and its impact on Orthopedic practice is clearly evident and immense. The problem of continuing OP consultations and orthopedic surgeries amid risk of infection needs awareness and proper implementation of personal safety protocols. Reservation of hospital supplies and ICU beds for COVID care has to be kept in mind while strategy planning to judiciously continue orthopedic practice. The wellbeing of both the surgeon and health care seeker must be upheld in all levels of planning to tide over the crisis caused by COVID-19 pandemic. Our study and emerging scenario only prove that orthopedic practice will suffer in COVID times. Let us tread cautiously prioritizing community safety and be patient for a vital break-through to emerge. As a healthcare provider we need to play our role in educating the public and create awareness about preventive measures. Till the end of the pandemic a harmonious coexistence with the invisible enemy is all that can be possible. There is always light at the end of the tunnel.
References
- Advisory for hospitals and medical education institutions. [Available from: https://www.mohfw.gov.in/pdf/AdvisoryforHospitalsandMedicalInstitutions.pdf].
- COVID-19 lockdown: Accidents dipped in Chennai, say traffic police. (2020) [Available from: https://www.thehindu.com/news/cities/chennai/COVID-19-lockdown-accidents-dipped-in-chennai-say-traffic-police/article31515730.ece].
- Sandeep Kumar, Rajesh Arora, IOA Advisory update 5th May.
- Park J, Yoo SY, Ko JH, et al. Infection prevention measures for surgical procedures during a middle east respiratory syndrome outbreak in a tertiary care hospital in South Korea. Sci Rep. 10: 325 (2020).
- Jain VK, Vaishya R. COVID-19 and orthopedic surgeons: The Indian scenario. Trop Doct. 50: 108-110 (2020).
- Hirschmann MT, Hart A, Henckel J, et al. COVID-19 coronavirus: Recommended personal protective equipment for the orthopaedic and trauma surgeon. Knee Surg Sports Traumatol Arthrosc. 28: 1690-1698 (2020).
- Wee LE, Conceicao EP, Sim XYJ, et al. Minimizing intra-hospital transmission of COVID-19: The role of social distancing. J Hosp Infect. 105: 113-115 (2020).
- Neradi D, Hooda A, Shetty A, et al. Management of orthopedic patients during COVID-19 pandemic in India: A Guide. Indian J Orthop. 54: 402-407 (2020).
- Kumar A, Kumar A, Das S. Perioperative COVID-19 testing for orthopaedic patients: Current evidence. J Clin Orthop Trauma. 11: 296-297 (2020).
- Guo X, Wang J, Hu D, et al. Survey of COVID-19 disease among orthopedic surgeons in Wuhan, People’s Republic of China. J Bone Jt Surg. 102: 847-854 (2020).
- Modi HN, Shrestha U, Desai YJ, et al. Evaluating the strategies for orthopedic and spine surgeries during COVID-19 pandemic in India-A retrospective analysis of 24 patients in a multispecialty hospital-are we heading to a new normal? Orthopedics. (2020).
- Haleem A, Javaid M, Vaishya R, et al. Effects of COVID-19 pandemic in the field of orthopaedics. J Clin Orthop Trauma. 11: 498-499 (2020).