Commentary - Interventional Cardiology (2013) Volume 5, Issue 5
Hybrid algorithm for chronic total occlusion percutaneous coronary intervention
- Corresponding Author:
- Elliot J Smith
Department of Cardiology
Barts Health NHS Trust, London, UK and NIHR Cardiovascular Biomedical Research Unit
London Chest Hospital, Bonner Road
London, E2 9RJ, UK
Tel: +44 208 983 2248
E-mail: elliot.smith@bartshealth.nhs.uk
Abstract
The field of percutaneous intervention for chronic total occlusion (CTO) has enjoyed a rich period of innovation in recent years. The advent of novel techniques and technologies is revolutionizing the field, such that intervention can be considered for a greater number of patients with increasing anatomical complexity. However, uptake of these novel techniques into routine clinical practice has been sporadic. In addition, the key advances, including the retrograde approach and dissection re-entry techniques, have evolved in parallel, such that the applicability of any one novel skill set may be uncertain in clinical practice. Thus, there has been a need not only for technical innovation, but also for innovation in our approach to CTO percutaneous coronary intervention (PCI) itself. The hybrid algorithm for CTO PCI represents that key step. Guided by detailed angiographic assessment, it provides a framework that integrates the available techniques to achieve reproducible procedural success in routine clinical practice. In this article, we describe the key innovations that are enhancing success rates, and the rationale for and application of the hybrid algorithm for CTO PCI.
Keywords
chronic total occlusion, dissection re-entry, hybrid algorithm, percutaneous intervention, retrograde, wire escalation
The field of percutaneous intervention for chronic total occlusion (CTO) has enjoyed a rich period of innovation in recent years. The advent of novel techniques and technologies is revolutionizing the field, such that intervention can be considered for a greater number of patients with increasing anatomical complexity. However, uptake of these novel techniques into routine clinical practice has been sporadic. In addition, the key advances, including the retrograde approach and dissection re-entry techniques, have evolved in parallel, such that the applicability of any one novel skill set may be uncertain in clinical practice. Thus, there has been a need not only for technical innovation, but also for innovation in our approach to CTO percutaneous coronary intervention (PCI) itself. The hybrid algorithm for CTO PCI represents that key step. Guided by detailed angiographic assessment, it provides a framework that integrates the available techniques to achieve reproducible procedural success in routine clinical practice. In this article, we describe the key innovations that are enhancing success rates, and the rationale for and application of the hybrid algorithm for CTO PCI.
The challenge
CTOs are particularly challenging to treat with PCI. Despite CTOs being common in patients undergoing coronary angiography; reportedly present in >50% of patients with significant coronary stenosis (defined as a >70% coronary diameter stenosis) [1], CTO PCI accounts for only 10–15% of PCI procedures [2]. The explanation for this situation is multifactorial. However, the main barriers to CTO PCI are predominantly procedure- rather than patient-related. CTO PCI has traditionally been associated with prolonged procedure times, with increased radiation dose, contrast volume and unpredictable success rates, which may adversely impact the patient, the operator and overall catheter laboratory efficiency [3]. However, procedural success is associated with significant benefits including effective angina relief [4], improved left ventricular function [5] and exercise tolerance [6], and emerging data suggest that there may also be a prognostic advantage, with a number of registries describing improved long-term survival in patients that undergo successful CTO PCI when compared with patients that had an unsuccessful CTO procedure [7,8]. Thus, achieving safe, predictable and reproducible success has been the challenge.
Innovation in CTO PCI
Until recently, CTO PCI was associated with low procedural success rates despite significant anatomical case selection. Traditionally, antegrade wire escalation (AWE) was the cornerstone of practiced technique for CTO recanalization. AWE refers to the use of guidewires of differing characteristics (usually increasing stiffness/penetration power) to cross a CTO from the proximal to the distal vessel, aiming to remain within the true vessel lumen or plaque segment. However, AWE achieves success rates of no more than 70% in selected populations [9]. Failure to recanalize the CTO vessel is usually a consequence of the guidewire tracking into the subintimal space. Parallel or ‘see-saw’ wire techniques may be used to recross the CTO segment using the first wire as a marker; however, distal true lumen re-entry remains unpredictable. Two key innovations are improving procedural success rates in a wider population of CTO patients: retrograde wiring via collateral channels and utilization of the subintimal space either retrogradely or antegradely to deliver equipment across long or calcific CTO segments.
▪ Retrograde techniques
Retrograde CTO PCI offers an alternative when anatomical considerations make approaches to anterograde CTO recanalization unfavorable – for example, a blunt proximal cap with an associated side branch or ambiguous proximal cap anatomy. More commonly, septal collaterals (and less commonly epicardial collaterals) are used to access the distal true lumen of a CTO vessel, and facilitate retrograde recanalization of the vessel. Retrograde wire escalation through a CTO is achieved only in the minority of cases [10]. As with AWE, the guidewire will often track into the subintimal space and access to the proximal true lumen cannot be achieved without a re-entry technique.
▪ Subintimal dissection and re-entry
The ability to utilize the subintimal space in a controlled manner has been a major step in improving success in CTO PCI, whether operating antegradely or retrogradely.
“The hybrid approach to chronic total occlusion integrates the available contemporary techniques and technologies into an understandable, reproducible and teachable algorithm.”
Antegrade dissection and re-entry describes the use of a guidewire and/or microcatheter to advance antegradely around the CTO segment with blunt dissection through the subintimal tissue (inside the vessel wall but outside the true lumen and thus the CTO). This can be achieved using a knuckled polymer jacketed wire as described in the subintimal tracking and reentry technique (STAR) [11] or the specifically designed CrossBoss® catheter (Boston Scientific, MA, USA) [12]. The latter is an over-the-wire microcatheter with a nonpenetrative rounded tip that can rapidly traverse the subintimal space maintaining a small controlled dissection plane. When a subintimal position beside the distal true lumen is achieved, then re-entry into the true lumen can be performed with a dedicated crossing technology (the Stingray® balloon and wire system, Boston Scientific). This consists of a 2.0 × 1.0 mm (flat) balloon with two exit ports located 180° apart, such that when deployed in the subintimal space adjacent to the distal true lumen, one port is oriented pointing toward the lumen and the other to the adventitia. The Stingray guidewire, which has a short penetrative barb at its distal tip, can then be advanced through the luminal exit port of the balloon until the wire crosses into the distal true lumen [12].
Retrograde dissection and re-entry is most commonly achieved using the reverse controlled antegrade retrograde tracking technique (reverse CART) [13]. In this technique a retrograde microcatheter is advanced over a guidewire via a collateral vessel and positioned within the CTO segment (either luminal or subintimal). An antegrade wire is then advanced into the CTO segment adjacent to the retrograde microcatheter and balloon dilatation performed. Before balloon dilatation the antegrade balloon and retrogade microcatheter may both lie in the subintimal space, both within the true vessel lumen, or a combination. Balloon dilatation facilitates the colocalization of both systems within the vessel structure. A guidewire can then be passed from the retrograde microcatheter into the proximal true vessel lumen. This guidewire is commonly externalized via the antegrade guiding catheter and angioplasty and stenting are then performed antegradely in the usual fashion [14].
Hybrid algorithm for CTO PCI
Although novel CTO PCI techniques offer the opportunity to achieve procedural success in a greater proportion of patients, there has been debate as to the optimal strategy for any individual case. The perceived wisdom has been that AWE is the optimal approach in almost all cases, and that only if this approach proves unsuccessful, the options of continued medical therapy, surgery or a repeat attempt by a specialist retrograde operator could be considered. Meanwhile the optimal successful strategy among operators with a subspecialist interest in CTO has not been certain. The hybrid algorithm for CTO PCI was conceived by a group of experienced CTO operators during a workshop that took place in Bellingham (WA, USA) in January 2011 [15]. The goal was to establish an algorithm that could provide CTO operators with a safe, reproducible, efficient and, most importantly, effective methodology for approaching CTO PCI. In total, 17 complex CTO cases were performed over a period of 3 days (all successful). Five operators undertook the interventions, with the remaining participants observing, supporting and advising in real-time. Simultaneously the group learned from each case and each other. The cases underwent detailed angiographic review by the group preprocedure, and consensus was sought as to the most effective initial approach based on a broad range of clinical experiences and the available evidence at that time. Each case was analyzed during and after the procedure, and then decision trees mapped. From this, an outline algorithm was born.
The key principles of the hybrid algorithm can be summarized as follows. First, once the clinical decision to perform PCI has been made, the coronary anatomy dictates the interventional strategy. Second, multiple techniques may be utilized during a single case, switching early from a failing strategy to optimize the likelihood of success. Third, where multiple interventional strategies are equally applicable, the most efficient with respect to radiation, contrast utilization and procedure time should be employed first.
Careful preprocedural angiographic review is mandatory. In order to fully understand CTO anatomy at the time of the procedure, it is essential to perform dual coronary injections into the CTO PCI vessel and the donor vessel that collateralizes the distal target vessel. Dual injections allow visualization of four key anatomical features that guide intervention:
▪ The nature of the proximal cap: this refers to the ability to accurately localize the angiographic proximal entry point to the CTO;
▪ The length of the occlusion: lesion lengths <20 mm are associated with a high chance of crossing with a guidewire in the majority of cases. Longer lesions are associated with lower success rates and longer procedure times when approached using standard AWE strategies [9]. Thus, in the hybrid algorithm, longer lesions are best approached using dissection re-entry techniques, either antegradely or retrogradely;
▪ The nature of the target distal vessel: this refers to the size of the distal vessel, whether the vessel is diffusely diseased or has a bifurcation at the planned landing zone, and the degree to which the distal vessel can be visualized;
▪ The presence of suitable interventional collateral options for the retrograde technique: optimal collateral vessels for retrograde CTO PCI are those that can be accessed safely with wires and microcatheters, have minimal tortuosity and enter the distal vessel beyond the distal cap of the CTO.
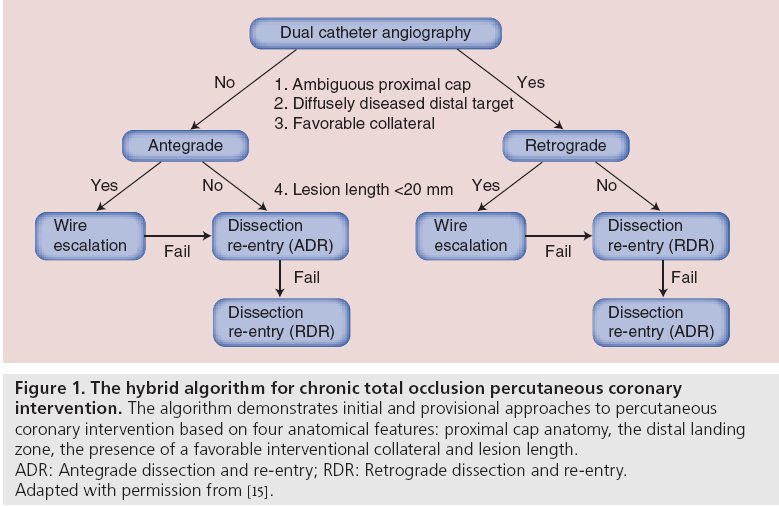
Using the hybrid algorithm the initial strategy for CTO recanalization is directed by the coronary anatomy based upon these four anatomical features. However, all strategies for CTO recanalization may be considered during the index procedure as required. The emphasis is on procedural efficiency, recommending an early switch from a failing strategy to maximize the chance of procedural success. Therefore, if progress was not made with an intial antegrade wiring approach (even where the angiographic assessment may have appeared favorable), a change to either antegrade dissection re-entry or a retrograde procedure would be made at the time of intervention based on intraprocedural review of the anatomy. Persistence with the same intial stragety and/or returning for a repeat procedure would be avoided where possible. Figure 1 demonstrates the initial and provisional approaches to a CTO PCI using the hybrid algorithm. Figure 2 demonstrates the algorithm in practice.
Figure 1: The hybrid algorithm for chronic total occlusion percutaneous coronary
intervention. The algorithm demonstrates initial and provisional approaches to percutaneous
coronary intervention based on four anatomical features: proximal cap anatomy, the distal landing
zone, the presence of a favorable interventional collateral and lesion length.
ADR: Antegrade dissection and re-entry; RDR: Retrograde dissection and re-entry.
Adapted with permission from [15].
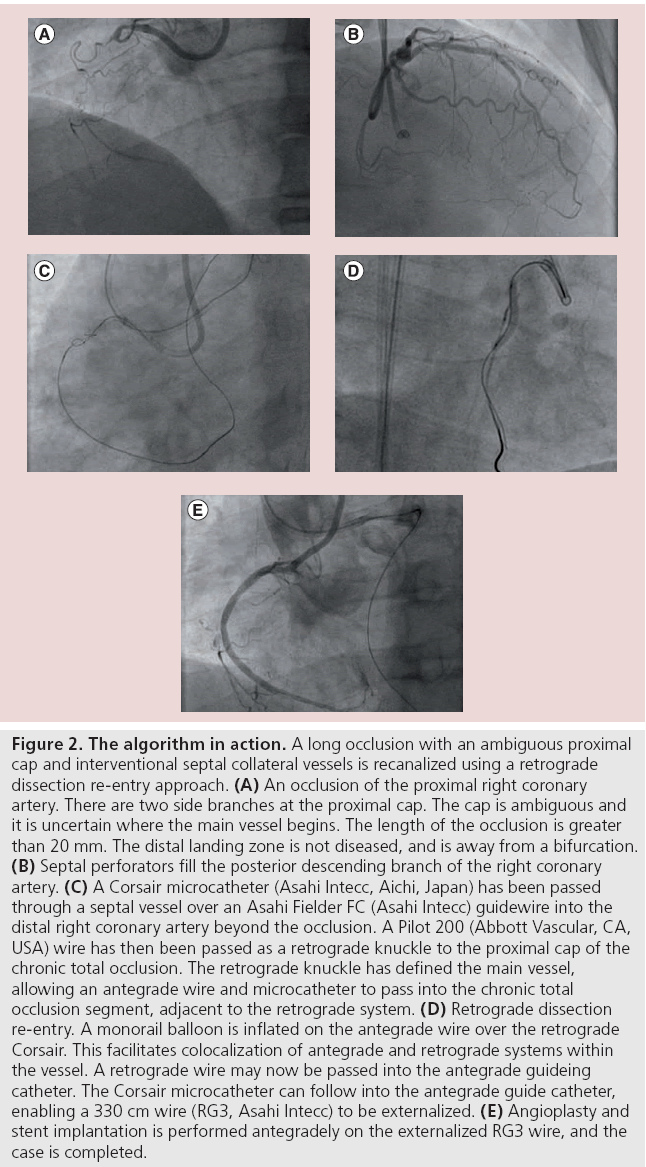
Figure 2: The algorithm in action. A long occlusion with an ambiguous proximal cap and interventional septal collateral vessels is recanalized using a retrograde dissection re-entry approach. (A) An occlusion of the proximal right coronary artery. There are two side branches at the proximal cap. The cap is ambiguous and it is uncertain where the main vessel begins. The length of the occlusion is greater than 20 mm. The distal landing zone is not diseased, and is away from a bifurcation. (B) Septal perforators fill the posterior descending branch of the right coronary artery. (C) A Corsair microcatheter (Asahi Intecc, Aichi, Japan) has been passed through a septal vessel over an Asahi Fielder FC (Asahi Intecc) guidewire into the distal right coronary artery beyond the occlusion. A Pilot 200 (Abbott Vascular, CA, USA) wire has then been passed as a retrograde knuckle to the proximal cap of the chronic total occlusion. The retrograde knuckle has defined the main vessel, allowing an antegrade wire and microcatheter to pass into the chronic total occlusion segment, adjacent to the retrograde system. (D) Retrograde dissection re-entry. A monorail balloon is inflated on the antegrade wire over the retrograde Corsair. This facilitates colocalization of antegrade and retrograde systems within the vessel. A retrograde wire may now be passed into the antegrade guideing catheter. The Corsair microcatheter can follow into the antegrade guide catheter, enabling a 330 cm wire (RG3, Asahi Intecc) to be externalized. (E) Angioplasty and stent implantation is performed antegradely on the externalized RG3 wire, and the case is completed.
The implication of this approach is that in order to be successful, operators require training in all the key skill sets of antegrade wiring, antegrade dissection–re-entry and retrograde CTO PCI. Intial setup with dual arterial access and guiding catheters is essential in the vast majority of cases (including those with a dominant collateral circulation arising from an ipsilateral donor artery). The skill sets are accessible to any trained interventionist, but high procedural success rates will be best achieved by a small number of designated operators per center in order to ensure sufficient case volume to develop proficiency. Thus, operators wishing to perform CTO PCI should approach this collaboratively with support from the non-CTO operators within their institutions. Ideally, collaborations should also extend across local networks of PCI centers to enhance access of all CTO operators to appropriate training and education. Live case courses and major national and international meetings are valuable in showcasing the available techniques and technologies, but are not sufficient in isolation to provide a platform for reproducible success. Local and regional CTO days with visiting trainers or proctors for more complex cases have been effective in enhancing the wider application and success of the approach. This style of training has similarities with structural programs, such as transcatheter aortic valve implantation, with the main difference being that CTO cases may require more than one enabling technique or technology.
Increasing adoption of the hybrid algorithm has resulted in a wider population of patients with more complex anatomy being offered CTO PCI. In a recent study, success rates of 85% were achieved in a population of which 37% had previously undergone bypass surgery [16], a traditional risk factor for procedural failure. However, while this level of success is impressive, we are still not yet approaching 100% (as with non-CTO cases). The inference, therefore, is that further innovations in the CTO space are needed. Current challenges remain, including calcification and vessel tortuosity, which are independent predictors of failure (and both of which appear in the Multicenter CTO Registry of Japan score of lesion complexity) [9].
A key advantage of the hybrid approach is its flexibility. As novel interventional options emerge and evolve, these can ultimately be integrated into the algorithm. The presence of a wider online CTO community is already contributing to that process [101]. If an operator faces (or indeed overcomes) a specific technical problem, the case can be uploaded for review and discussion for advice.
Conclusion
The field of CTO PCI has evolved significantly in recent years. The hybrid approach to CTO integrates the available contemporary techniques and technologies into an understandable, reproducible and teachable algorithm. The algorithm offers the opportunity to treat more complex anatomy successfully and, therefore, meet the needs of a wider patient population. Support for new CTO operators should be available to the majority of interventional cardiologists. However, our aim must be to further enhance success rates in even the most complex cases. As this process takes place, and more innovative therapies emerge, the algorithm will provide a framework within which successful treatments may be integrated, and the algorithm will itself evolve.
Financial and competing interests disclosure
EJ Smith received speaker honoraria from Boston Scientific, and is a proctor for Hybrid CTO PCI with support from Boston Scientific. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
- Christofferson R, Lehmann K, Martin G, Every N, Caldwell J, Kapadia S. Effect of chronic total coronary occlusion on treatment strategy. Am. J. Cardiol. 95, 1088–1091 (2005).
- Grantham J, Marso S, Spertus J, House J, Holmes DJ, Rutherford B. Chronic total occlusion angioplasty in the United States. JACC Cardiovasc. Interv. 2, 479–486 (2009).
- Bell M, Berger P, Menke K, Holmes DJ. Balloon angioplasty of chronic total coronary artery occlusions: what does it cost in radiation exposure, time, and materials? Cathet. Cardiovasc. Diagn. 25, 10–15 (1992).
- Grantham J, Jones P, Cannon L, Spertus J. Quantifying the early health status benefits of successful chronic total occlusion recanalization: results from the FlowCardia’s Approach to Chronic Total Occlusion Recanalization (FACTOR) Trial. Circ. Cardiovasc. Qual. Outcomes 3, 284–290 (2010).
- Baks T, Van Geuns RJ, Duncker D et al. Prediction of left ventricular function after drug-eluting stent implantation for chronic total coronary occlusions. J. Am. Coll. Cardiol. 47, 721–725 (2006).
- Finci L, Meier B, Favre J, Righetti A, Rutishauser W. Long-term results of successful and failed angioplasty for chronic total coronary arterial occlusion. Am. J. Cardiol. 66, 660–662 (1990).
- Jones D, Weerackody R, Rathod K et al. Successful recanalization of chronic total occlusions is associated with improved long-term survival. JACC Cardiovasc. Interv. 5, 380–388 (2012).
- Joyal D, Afilalo J, Rinfret S. Effectiveness of recanalization of chronic total occlusions: a systematic review and meta-analysis. Am. Heart J. 160, 179–187 (2010).
- Morino Y, Abe M, Morimoto T et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc. Interv. 4, 213–221 (2011).
- Yamane M, Muto M, Matsubara T et al. Contemporary retrograde approach for the recanalisation of coronary chronic total occlusion: on behalf of the Japanese Retrograde Summit Group. EuroIntervention 9, 102–109 (2013).
- Colombo A, Mikhail G, Michev I et al. Treating chronic total occlusions using subintimal tracking and reentry: the STAR technique. Catheter. Cardiovasc. Interv. 64, 407–411; discussion 412 (2005).
- Whitlow P, Burke M, Lombardi W et al. Use of a novel crossing and re-entry system in coronary chronic total occlusions that have failed standard crossing techniques: results of the FAST-CTOs (Facilitated Antegrade Steering Technique in Chronic Total Occlusions) trial. JACC Cardiovasc. Interv. 5, 393–401 (2012).
- Brilakis E, Grantham J, Thompson C et al. The retrograde approach to coronary artery chronic total occlusions: a practical approach. Catheter Cardiovasc. Interv. 79, 3–19 (2012).
- Joyal D, Thompson C, Grantham J, Buller C, Rinfret S. The retrograde technique for recanalization of chronic total occlusions: a step-by-step approach. JACC Cardiovasc. Interv. 5, 1–11 (2012).
- Brilakis E, Grantham J, Rinfret S et al. A percutaneous treatment algorithm for crossing coronary chronic total occlusions. JACC Cardiovasc. Interv. 5, 367–379 (2012).
- Michael T, Karmpaliotis D, Brilakis E et al. Procedural outcomes of revascularization of chronic total occlusion of native coronary arteries (from a Multicenter United States Registry). Am. J. Cardiol. 112(4), 488–492 (2013).
▪ Website
- CTO Fundamentals. www.ctofundamentals.org