Research Paper - Clinical Investigation (2023) Volume 13, Issue 4
Epidemiological aspects of the management of heart failure patients seen in cardiological consultation at the Niamey National Hospital
- Corresponding Author:
- Idrissa Hama
Abdou Moumouni University of Niamey, Faculty of Health Sciences, France
E-mail: hama_idrissa@yahoo.fr
Received: 01-March-2022, Manuscript No. fmci-22-55852; Editor assigned: 03-March-2022, Pre QC No. fmci-22-55852 (PQ); Reviewed: 14-March-2022, QC No. fmci-22-55852 (Q); Revised: 22-March-2022, Manuscript No. fmci-22-55852 (R); Published: 29-April-2023; DOI: 10.37532/2041-6792. 2023.13(4).447-451
Abstract
Introduction: Heart failure is defined as a structural or functional abnormality of the heart resulting in an inability to supply the tissues with oxygen at a rate in line with their needs.
Objective: Contribute to a better understanding of the epidemiological aspects of the management of patients with heart failure.
Methodology: This is a prospective and cross-sectional study conducted over a period of 6 months.
Results: Thus our sample consisted of 300 cases. The female sex predominated with 66.5%, the average age was 56.9 ± 13.7 with extremes ranging from 19 years to 98 years. Housewives were the most represented at 43.7%. High blood pressure and sedentary lifestyle were the main FDRs found in patients in 95% followed by obesity in 22.3%. In 61.3% of cases patients know they have heart disease but do not know the type. Unusual shortness of breath on exertion was the main sign that made patients consult with 67.7%. Only 2% weighed themselves regularly. All of our patients (99%) knew the sodium restriction recommendation and more than half (58.3%) had suitable for low sodium diet. Only 23.2% of our patients drank less than 1.5 L per day. 29.7% of our patients did not practice any physical activity. Regarding the treatment, diuretics were the most used as specific treatment 64.3% and for non-specific treatment platelet aggregation
inhibitors in 12.3% of cases.
Conclusion: Our study has highlighted educational gaps in the heart failure population. Further studies could help to initiate a therapeutic education approach for patients to finally improve their quality of life and morbidity and mortality.
Keywords
Epidemiological aspects • Management • Heart failure • HNN • NIGER
Introduction
Known to doctors since antiquity, Heart Failure (HF) is defined as a structural or functional abnormality of the heart resulting in an inability to supply the tissues with oxygen at a rate in line with their needs. The therapeutic recommendations of the European Society of Cardiology (ESC) distinguish 3 types of heart failure: heart failure with reduced ejection fraction (by contractile failure), with moderately reduced ejection fraction and with ejection fraction preserved (by insufficient relaxation of the myocardium) [1]. Heart failure is considered a major public health problem in industrialized countries. Its prevalence is estimated between 3 and 20 per 1000 and increases Known to doctors since antiquity, Heart Failure (HF) is defined as a structural or functional abnormality of the heart resulting in an inability to supply the tissues with oxygen at a rate in line with their needs.
The therapeutic recommendations of the European Society of Cardiology (ESC) distinguish 3 types of heart failure: heart failure with reduced ejection fraction (by contractile failure), with moderately reduced ejection fraction and with ejection fraction preserved (by insufficient relaxation of the myocardium) [1]. Heart failure is considered a major public health problem in industrialized countries. Its prevalence is estimated between 3 and 20 per 1000 and increases considerably with age [2]. According to the World Health Organization (WHO), the number of people suffering from heart failure in the world is estimated at twenty million and the 5-year mortality rate of these people is between 50% and 60%. In Niger, studies on heart failure in 2001 and 2013 showed a respective frequency of 10% and 35.15% of hospitalized patients, i.e. an increase in the frequency of the disease [3]. The benefit of therapeutic education (improvement in quality of life, reduction in morbidity and mortality) has made it essential for the management of heart failure, like other chronic diseases such as diabetes, chronic kidney disease, asthma or Chronic Obstructive Pulmonary Disease (COPD) [1, 4].
What is the level of prior knowledge of the patients? Do they adhere to the care proposals that the medical community offers them?
Goals
Contribute to a better understanding of the epidemiological aspects of the management of heart failure patients at the HNN.
Material and Methods
Our study is prospective and cross-sectional conducted over a period of 6 months, from February 2020 to October 2020. We suspended 2 months due to the Corona Virus (Covid 19). Were included in our study: Patients without distinction of sex received in cardiology consultation. Any patient who has presented symptoms or signs of heart failure at least once in their history (exertional dyspnea, orthopnea, peripheral oedema, jugular turgor, etc.). A functional heart abnormality was known or strongly or suspected (old or poorly controlled hypertension). Patients who did not give their consent and who were not considered to have heart failure were excluded from the survey. The data was collected on a survey form which has 5 pages with the parameters: patient identity, cardiovascular risk factors, evaluation on knowledge of the diagnosis, evaluation on the monitoring of warning signs, evaluation on knowledge and adherence to treatment. The advent of COVID 19 and the non-consent of certain patients. Data collection was manual through a survey form. The data was entered and analyzed using Epi info software in version 7.2.2.3 and Microsoft Word and Microsoft Excel. This was a prospective and crosssectional survey derived from the WHO method which took place from November 15, 2019 to January 15, 2020, i.e. a period of 2 months. We collected 1000 respondents.
Results
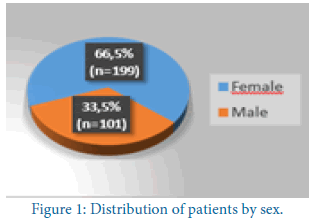
We collected 300 respondents of which the female sex represented 66.5%. The average age of the patients was 56.9 years with a standard deviation of 13.7 years and extremes of 19 years and 98 years. The age group of 46 years to 75 years was the most represented with 74.7% of patients. Patients came from Niamey in 68.3% of cases. The patients were housewives in 43.7% of cases (Figure 1).
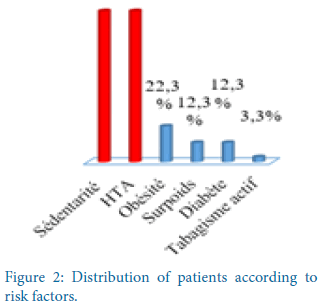
The Zarma ethnic group was the most represented 53.7% of cases. The mean body mass index was 25.9 kg/m² ± 4.9 kg/m². 22.3% of our patients were obese (Figure 2).
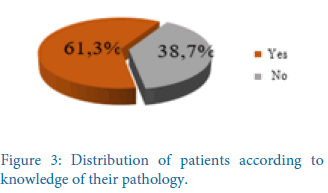
Patients were sedentary and hypertensive in 95% of cases. In 61.3% of cases, patients admitted to having heart disease but without knowing the type. Patients measured their weight less than once a week in 98% of cases. Unusual shortness of breath on exertion and fatigue were signs that would prompt medical attention in 67.7% and 51.7% of cases, respectively. According to 99.7% of there is no connection between shortness of breath and fluid retention. The patients followed a diuretic treatment in 64.3% of the cases (Figure 3).
Patients claimed to have never failed to take their treatment in 88.7% of cases. Heart failure should limit their salt intake according to 99% of patients. Patients could not estimate their daily water consumption in 77% of cases. For patients who were able to estimate their daily water consumption, 23.2% estimated it at less than 1.5 litres. Seasoning spices and commercial soup were high in salt according to the patients in 98.7% and 96% of cases respectively. Patients said that physical activity is recommended for heart failure in 93% of cases. The patients practiced a physical activity of more than one hour thirty minutes in 48.6% of the cases. 2/3 of our patients engage in physical activity per week. Walking was the physical activity practiced by all the patients. More than half of the patients consumed about 5 g of salt per day. None of our patients have knowledge of the exact amount of salt consumed per day by a heart failure patient. Heart failure requires lifelong treatment according to 61.7% of patients. The measurement of blood pressure was necessary for the follow-up of patients with heart failure according to 99.3% of patients (Table 1).
Table 1: distribution of patients according to follow-up for heart failure
| Follow-up of heart failure | Number | Percentage |
|---|---|---|
| Cardiologist | 296 | 98.70% |
| General practitioner | 95 | 31.70% |
| Diabetologist | 40 | 13.30% |
| Nurses | 39 | 13% |
As background treatment, diuretics were the most used at 64.3% followed by beta-blockers in 53.7% of patients and ACE inhibitors in 53% of patients. The most frequently used non-specific treatment was platelet aggregation inhibitors in 12.3% of cases, followed by statins (Table 2).
Table 2: Distribution of patients according to the type of drug used in specific treatment
| Type of disease-modifying drug | Number | Percentage(%) |
|---|---|---|
| Diuretic | 193 | 64.30% |
| Beta blockers | 161 | 53.70% |
| IEC | 159 | 53% |
| IC | 154 | 51.30% |
| Antialdosterone | 53 | 17.70% |
| Digoxin | 5 | 1.70% |
Discussion
Our study showed a predominance of women received in cardiology consultation for heart failure. 66.5% of cases against 33.5% of male sex with a sex ratio of 0.5. This frequency is higher than that in 2001 [5]. In 2020 Niger who found 58.9% and 58.3% respectively. Our results are contrary to those of in 2013 Niger who found a male predominance of 53.6%. This female predominance may be linked to the fact that certain etiologist of heart failure is not found in men, such as postpartum cardiomyopathy. In our series, the age group between 46 years and 75 years is the majority with 74.7%. Our results agree with those in 2017 in Morocco who found 80% for the age group of 50 years to 79 years. On the other hand, in 2018 in Mali found lower results up to 44.1% [6]. This could be explained by the fact that heart failure is a pathology of the elderly.
The patients came from Niamey in 68.3% and from Tillabery in 13%. Our results are similar to those of Salifou S in 2014 in Niger who found 65.9% for Niamey and 19.5% for Tillabéry. On the other hand, Mahamane D found a preponderance of patients coming from the Tillabery region (47.59%) and from Niamey (24.10%). This could be explained by the fact that patients living in Niamey and Tillabery are closer to the National Hospital of Niamey.
In our series, 43.7% of patients were housewives. Our results are similar to those of Salifou S and Hawa J who found 62.1% and 39% respectively [7, 8]. This could be explained by the female predominance in our study and especially the low rate of schooling of women/girls in our country. The Zarma are the most represented with 53.7%. Our results are comparable to those of Hamza B in 2018 in Niger which found 60% zarma [9]. In our study, hypertension was found in 93% of patients. Our results are superior to those of Hawa J and Salifou S with 42.2% and 63.4% respectively. Other CVRF such as tobacco, diabetes and obesity are less encountered in our patients. The first question asking the patient if he has heart disease, 61.3% or 184 cases answered having heart disease but without knowing the type. Our results are lower than those of Guillaume L in 2017 in France who found that 71.37% of patients said they had heart disease. In our study, only 2% of patients reported weighing themselves once or twice a week compared to 98% who weighed themselves less than once a week. Our results are lower than those of Guillaume L and Bruni V who found 48.2% and 61% respectively. This could be explained by the fact that the majority of our patients have no education.
In our series, patients consulted more for unusual shortness of breath on exertion up to 66.8% compared to other symptoms. Our results agree with those of Maire-Edlinger A in 2011 in France and Guillaume L who found 90% and 90.6% respectively [10]. In our study, the treatment of 64.3% of our patients contained a diuretic. This is comparable to the results of Guillaume L who found 53.1%.
In our sample, 93% of patients recognized that physical activity is recommended in patients with heart failure. Our results are similar to those of Guillaume L. who recovered 93.8%. Patients who practiced physical activity represented 70.3% of our sample. Our results agree with those found by Bruni V. in 2012 in France which had recovered 72% [11]. The most practiced type of activity is walking at 69.4%. In our study, 97.1% of patients said that heart failure should limit their salt intake. Guillaume L found lower height results of 81.3%. In our series, 58.3% of our patients had adapted a low-sodium diet. Our results are lower than those found by Maire-Edlinger A and Bruni V with 76% and 83% respectively.
For 26.6% of patients, heart failure must limit their cholesterol intake, 16.4% for sugar intake and only 2.3% for water intake. This could be explained by the fact that in society, heart diseases such as hypertension and heart failure are considered saltrelated diseases. Of the patients who were able to estimate their daily water consumption, only 23.2% were able to estimate it to be less than 1.5 l. The results are lower than those of Guillaume L who found 78.1%. In our series, 60.9% of patients said they were aware that heart failure required lifelong treatment. Guillaume L found superior results up to 87.5%. In our study, 99.8% of patients considered that better knowing their disease would help them live better. Our results are comparable to those of Guillaume L who found 93.8%.
The most frequently associated non-specific treatment for heart failure was platelet aggregation inhibitors (12.3%) followed by statins (7%) and anticoagulants in 4% of cases. Unlike Guillaume L who found a predominance of anticoagulants at 50% followed by statins at 43.8% and antiplatelet drugs at 34.4%. For the specific treatment of heart failure, diuretics were the most used (64.3%) followed by beta-blockers (53.7%) then ACE inhibitors (53%). Our results are contrary to those found by Theo P in France in 2020, which found a predominance of betablockers (81.6%) then diuretics (75.5%) then ACE inhibitors (71%) [12].
Conclusion
Heart failure is a chronic disease with very high morbidity and mortality. Its diagnosis remains difficult, its treatment rarely optimized. The multitude of efforts made have not made therapeutic education accessible to all patients. At the end of this study, it appears that the population was mainly made up of elderly people around their sixties who mostly resided in urban areas. More than half of our patients had knowledge of their heart disease but without knowing the type and all of our patients know that heart failure must limit their salt intake.
Thus it results that half of the patients had a misunderstanding of the disease, its mechanisms, the usefulness and the importance of the treatment. Further studies could help to initiate a therapeutic education process for patients to finally improve their quality of life and morbidity and mortality.
References
- Guillaume L. Evaluation of the level of therapeutic education of patients with heart failure in general practice based on a Rapid Educational Diagnostic Test in heart failure: Medicine thesis. Claude Bernard Univ. (2017).
- Nouracham A. Epidemiological, clinical and evolutionary aspects of cardiovascular diseases in women in tropical African environments in Niger. Niamey med. thesis. (2014).
- Mahaman B. Heart failure at the National Hospital of Niamey: Epidemiological, clinical, paraclinical and therapeutic aspects. Niamey. (2001).
[Google Scholar] [Cross ref]
- Moctar M. Heart failure epidemiology, clinic, diagnosis and treatment: Medicine thesis. Niamey. (2013).
- Garba F. Cardiovascular risk factors in the department de Say: medical thesis. Abdou Moumouni Univ. (2020).
- Ghita K. Drug treatment of heart failure: evaluation of the degree of compliance with international recommendations. Marrakech med thesis. (2017).
[Google Scholar] [Cross ref]
- Hawa J. Epidemiological, clinical and therapeutic study of heart failure in adults at the Nianankoro Fomba hospital in SEGOU. Med thesis. (2018).
- Salifou S. Evaluation of the management of acute coronary syndromes: medicine thesis. Abdou Moumouni Univ. (2014).
- Hamza B. Epidemiological and etiological profile of heart failure: prospective cross-sectional study on 12 cases collected at the cardiology center of the HNN in Niamey from August 2, 2017 to February 2, 2018: medical theses. Abdou Moumouni Univ. (2018).
- Maire EA. Patient and therapeutic education: perception by the patient of the management of the patient with heart failure: medicine thesis. Henri Poincare Univ.. (2011).
- Bruni V, Loll AC, Guiader J, et Al. Therapeutic education of patients in heart failure: evaluation of a program. Ann Cardiol Angeology. 61(2):74-80(2012).
- Theo P, Emmanuel B, Jean G, et al. Epidemiological characteristics and therapeutic management of patients with chronic heart failure who use smartphones: potential impact of a dedicated smartphone application( report from the OFICSel Study). Arch Cardiovasc Dis. 79(6):546-54(2020).