Research Article - Clinical Practice (2017) Volume 14, Issue 2
Comparison the efficacy of three positive pressure ventilation devices used by medicine students on a neonatal resuscitation simulators
- Corresponding Author:
- Sergio Agudelo Pérez
School of Medicine, Universidad de La Sabana
Campus del Puente del Común, Chia, Cundinamarca, Colombia
E-mail: sergioap@clincaunisabana.edu.co
Abstract
Background: Positive pressure ventilation is the most frequently used intervention for the resuscitation of newborns. It should guarantee pressures and volumes in safe and effective ranges to establish appropriate pulmonary ventilation and prevent pulmonary injury. The objective of this study was to compare the efficacy of ventilation of three manual PPV devices used on a neonatal resuscitation simulator by medical students. Methods: An experimental two-factor (device and student) study design with several replications of the experiment (a ventilation cycle performed by a student in one minute with each device) was used. Students in their last year of school of medicine at the Universidad de La Sabana were included. The data were collected using a pressure sensor. The peak inspiratory pressure (PIP), the positive end-expiratory pressure (PEEP) by ventilation, and the respiratory rate per minute were recorded for each participant. Pressure in safety range was used as efficacy endpoint. Results: 30 students were included in the study. With the self-inflating bag (SIB) and the flow-inflating bag, a higher percentage of PIP and PEEP was found to be ineffective. No device exceeded the maximum PIP. The use of the disposable T-piece resuscitator resulted in PIP within the safety range 3.20 times more frequently and in PEEP within the safety range 963.8 times more frequently compared with the SIB. Conclusions: The disposable T-piece resuscitator was found to be the most efficacy device for manual ventilation, when used by inexperienced personnel for neonatal resuscitation.
Keywords
infant, newborn, resuscitation, positive-pressure respiration, resource allocation
Introduction
Approximately 10% of newborns require neonatal resuscitation at birth; positive pressure ventilation (PPV) is the most common intervention used for newborn resuscitation [1,2]. During PPV, it is recommended to use a peak inspiratory pressure (PIP) between 20 cm and 30 cm H20. Appropriate PIP establishes the functional residual capacity and generates reflexes that stimulate the onset of spontaneous breathing [1]. The application of PIP lower than these values has been associated with nonresponse to neonatal resuscitation manoeuvres [3,4]. It is recommended a positive end-expiratory pressure (PEEP) of between 5 cm and 8 cm H2O should be applied [5]. It has been reported that this PEEP improves the clinical response to the resuscitation manoeuvres, reduces the need for endotracheal intubation, improves the response to the surfactant, and decreases pulmonary injury and atelectotrauma [6]. Excessive volume and/ or pressure induce pulmonary injury, especially in the premature baby [1,7]. Therefore, VPP should be with pressures within the ranges of safety for establishing appropriate pulmonary ventilation while limiting pulmonary injury. The operator of the device must quickly and appropriately adjust the pressure and rate to the recommended ranges [1].
Different devices are available to perform positive pressure ventilation to the newborn in the delivery room. The T-piece resuscitator is designed to supply respirations with a previously adjusted PIP and PEEP. Most studies with T-pice resuscitator have been performed with the Neopufftm, and it seems to be the most effective and safest device [7]. The T-piece resuscitator is currently available in a disposable (Neo-Tee®). The availability of NeopuffTM in health centers of 1 and 2 level with limited economic resources is null. The self-inflating bag (SIB) is the most frequently used device, and its effectiveness depends on the operator’s profession and experience [8,9]. In studies using neonatal simulators, the SIB is the least safe, effective, and reliable device in terms of pressure and volume [10-12]. The flow-inflating bag its safety and effectiveness is better than that of the SIB [13]. The World Health Organization (WHO) recommends the use of the SIB in settings with limited economic resources, recognizing the need to establish neonatal resuscitation guidelines for resource-limited settings where the presence of specialized health personnel and technical resources may be insufficient to meet the International Liaison Committee on Resuscitation (ILCOR) recommendations [14].
The pressures and volumes generated by the device are operator dependent and variable, primarily when non-specialized or inexperienced personnel operate the device. In the Colombian context, the availability of specialized personnel or with experience in the care of newborns is limited in low- and medium-complexity health centers. In Colombia, trainees in their last year of medical school are the trained professionals who provide first- and second-level care health.
The objective of this study was to compare the efficacy, defined as the pressures generated for the PIP and PEEP in safety ranges, of three positive pressure ventilation devices to be used by trainees in the last year of medical school on a neonatal resuscitation simulator.
Methods
The Ethics Committee of the Universidad de La Sabana approved the study protocol. The student population signed their informed consent to participate.
An experimental two-factor study design with several replications of the experiment (a ventilation cycle performed by a student in one minute with one device) was applied. The first factor was related to the type of device, and the second was related to the student. Medical students from the Universidad de La Sabana in their last year of school and in their internship year in the Clínica Universidad de La Sabana were included.
The following devices were used: 1. AMBU® 220 ml SIB with PEEP regulator valve; 2. Flow-inflating bag (Mercury Medical 0.5 liter Hyperinflation System with pressure gauge); 3. Disposable T-piece resuscitator (Mercury Medical Neo-Tee®). A Merlin Medical triangular facemask with a padded edge and of an appropriate size for the simulator was used for all three devices. The neonatal resuscitation simulator that was employed was a PEDI® S320 model.
The data collection was performed by a pressure sensor with a flow signal acquisition system to detect the air insufflated into the neonatal simulator. The pressure sensor was placed at the site designed for the manometer of the device and connected to the pressure transducer. The system was composed of an Autonics TK45 reference control with a digital display and was configured to acquire the pressure transmitter signal of a 0-2 psi pressure gauge, ZHYQ model PT124B-216. Using an RS-485–to–USB communication interface, the data were sent to a Windows XP computer platform and were saved in a flat file. Autonics DAQMaster software was used to acquire the data for subsequent statistical analysis.
Design
Prior to the start of the study, the students took the Neonatal Resuscitation Programme course taught by certified instructors. The course consisted of two parts. The first theoretical and self-study by the students. The second practical part, where special emphasis was placed on the proper mask seal and the proper use of VPP device to ensure that this was not a factor influencing the results. Before to the data collection, the participants had time to practice with each device under the supervision of instructor, who reviewed the proper technique with a checklist. Once participant demonstrated correct use of the devices, the data collection phase began. Each student used the three devices to perform a cycle of PPV for one minute on the simulator with the mask device. They were asked to perform ventilations with a PIP of 25 cm H20 and a PEEP of 5 cm H20 at a rate 40 times per minute. A random list in Excel used to determine both the sequence of the operators and the sequence of the devices that each operator used. Each device had an analogue pressure gauge that the participants could observe while they provided ventilations. The SIB was used with the pressure release valve opened and with the PEEP regulator valve fitted. The three devices were connected to a gas source. For each participant, the PIP and PEEP for ventilation and the respiratory rate per minute was recorded for each device used.
Sample size estimation
A sample size of 30 individuals was estimated for an analysis of variance for repeated measures using the following parameters [15]: significance level (α) 0.05, power (β) 0.8, mean effect size (intraclass correlation coefficient, ICC) 0.35, correlation between measures 0.5, number of repetitions (K) 3.
Information processing and statistical analysis
Descriptive analyses were performed by calculating median for the PIP, PEEP, and respiratory rate per student per device type. The results are presented in graphs. Two dichotomous variables were established - one for PIP, and one for PEEP; these variables received a value of one when PIP or PEEP were within the safety range. The safety range for PIP was defined as a value between 20 cm and 40 cm H2O; for PEEP, the value was between 5 cm and 8 cm H2O. To determine the effectiveness of the devices for achieving appropriate ventilation, two multilevel analysis models for dichotomous variables were constructed with a random slope (device) and intercept (student): one for PIP and another for PEEP. The first level of the model represented the repetitions, and the second level represented the students. The dependent variable was whether PIP or PEEP was within the safety range for each repetition. The model used the formula Y_ij=(B_0+ a_j )+(B+ b_j )*x_ij+e_ij, where Yij is the dichotomous variable (PIP or PEEP) for repetition i of student j; B0 and B are the intercept and the average effect of the device, respectively; xij is the predictor variable (type of device); aj is the effect of the student on the intercept; and bj is the effect of the student on the slope. The information was processed using the STATA® program.
Results
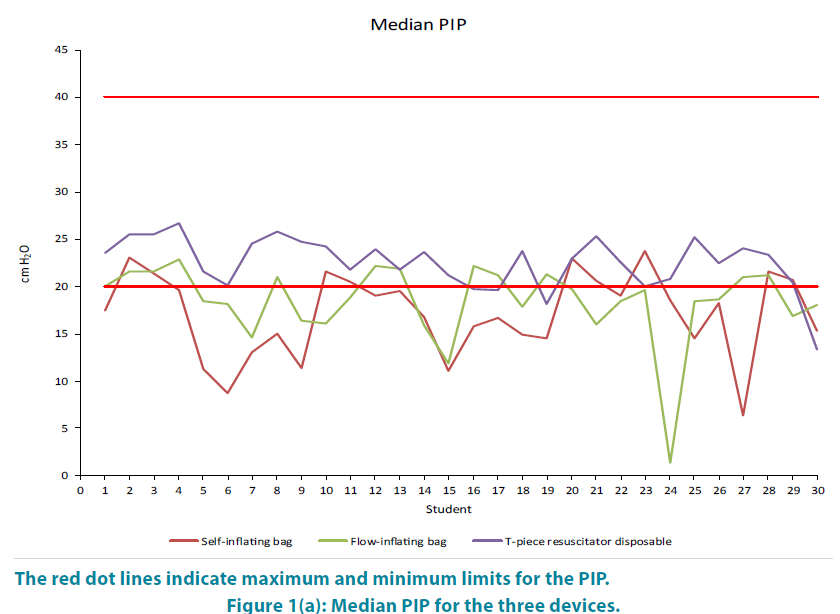
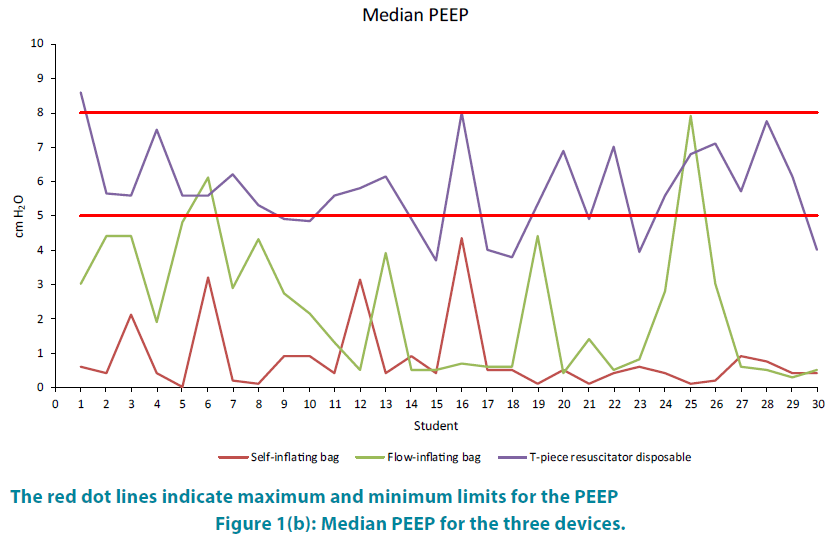
FIGURE 1A and 1B shows the median for PIP and PEEP. With the SIB and the flowinflation bag, ineffective pressure occurred a higher percentage of times. None of the devices resulted in excessive pressure.
The multilevel analysis of PIP showed the flow-inflation bag resulted in ventilation within the safety rage 1.20 times more frequently than the SIB, which was not a significant; in comparison, the disposable T-piece resuscitator was 3.20 times more frequently within the safety range than the SIB was. A comparison of the confidence interval between the flow-inflation bag and the T-piece resuscitator showed that the T-piece resuscitator did not include the interval of the flow-inflation bag and therefore was superior (TABLE 1).
| Variable | OR | 95% CI |
| PIP | ||
| Self-inflation bag Flow-inflation bag Disposable T-piece resuscitator |
1 1.20 3.19 |
1 (0.95 to 1.51) (2.49 to 4.09) |
| PEEP | ||
| Self-inflation bag Flow-inflation bag Disposable T-piece resuscitator |
1 39.98 963.82 |
1 (14.58 to 109.62) (285.71 to 3251.38) |
Table 1: Multilevel analysis of PIP and PEEP.
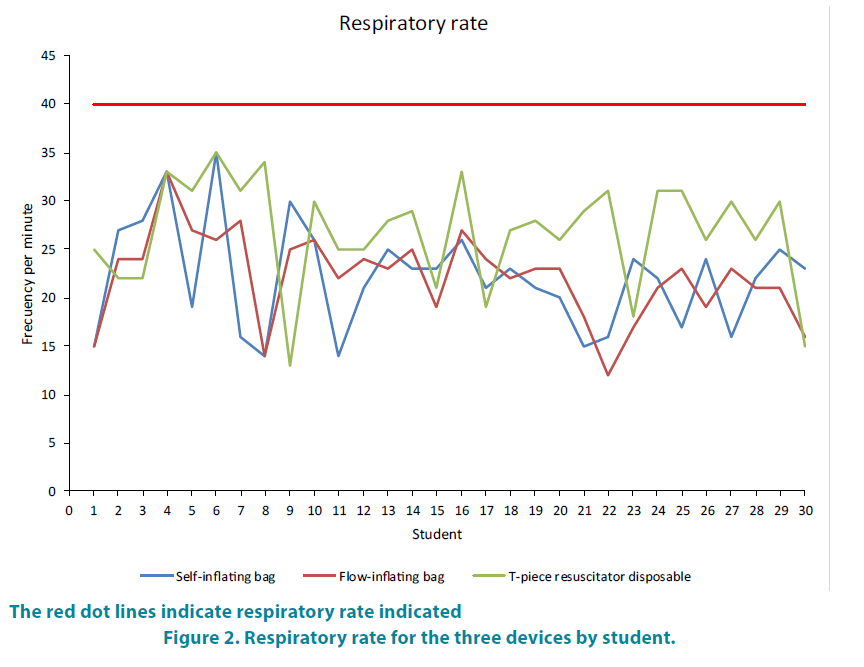
The multilevel analysis of PEEP showed that PEEP was 40 times more frequently in the safety range with the flow-inflation bag compared with the SIB and 963.8 times more frequently in the safety range with the disposable T-piece resuscitator than with the SIB. A comparison of the confidence intervals of the flow-inflation bag and the T-piece resuscitator showed that the interval of the latter did not include the interval of the flow-inflation bag and therefore was superior (TABLE 1). No student met the required 40 breaths per minute (FIGURE 2).
Discussion
We evaluated trainees in their last year of medical school and who will be performing their social service practice in level I and II health care centers in our country. Our study found that the disposable T-piece resuscitator (Neo-Tee®) delivered pressures (PIP and PEEP) within the range of safety more frequently than the other devices tested, and the results were statistically significant. These findings suggest that the use of this device by non-expert trained personnel can improve respiratory assistance for the neonate and can be a possible cost-effective alternative in level I and II health care settings with limited economic resources.
Studies using neonatal simulators have been conducted to examine the safety and effectiveness of different devices when used by personnel with experience and expertise in neonatal resuscitation at high complexity hospitals with neonatal units. Neopuff™ appears to be superior over the other devices in terms of the consistency and safety of pressure in simulation scenarios. TABLE 2 summarizes the studies comparing positive pressure devices. We found no studies comparing the use of these three devices in trainees.
| Studsy | Subjects | Devices | Intervention | MainFindings |
|---|---|---|---|---|
| Hawkes et al. (2012) [9] | Professional work in neonatal intensive care unit. | NEOPUFF Others |
Qualityreview. Emphasis on the evidence comparing the NEOPUFF to other manual ventilation devices in neonatal resuscitation. In newborn infants and simulator Measure: PIP, PEEP, Tidal Volume, Mask Leak |
T-piece resuscitator (NEOPUFF) include the delivery of inflating pressures closer to predetermined target pressures with least variation, the ability to provide prolonged inflation breaths and more consistent tidal volumes. |
| Finer et al. (2001), [10] | Neonatal Nurses Neonatal Nurse practitioners Neonatal staff Fellows Paediatric residents Neonatal Respiratory therapists |
Disposableanesthesiatype bag Jackson-Rees (JR) typeanesthesia bag Neopuff™ |
Use neonatal simulator to evaluate the use of three devices. Recorded ventilatingPressure: PIP PEEP |
Neopuff™ most consistently delivered pressures within the required ranges. PIP and the PEEP were significantly higher when respiratory therapists used the flow-inflation bag |
| Bennet et al. (2005), [13] |
Neonatologists Neonatal respiratorytherapists Neonatal fellows Pediatrician Pediatricresidents Neonatal nurse practitioners Neonatal nurses |
Neopuff™ Flow-inflation bag. Self-Inflating Bag |
Use neonatal simulator and using a continuouspressurerecordingsystem. Evaluatedtheabilitytodeliver a consistent PIP of 20 or 40 cmH2O and a PEEP of 5 cmH2O during 30 s of ventilation. |
Most accurate and reliable device for delivering pressure within safe ranges was the Neopuff™, which had a maximum PIP that was lower than the other devices, while the SIB had a lower PEEP value compared with the other devices |
| Roehr et al. (2010), [12] | Pediatricians Obstetricians Anesthesiologist Neonatal nurses Midwives |
self-inflating bag T-pieceresuscitator (Neopuff™) |
Use premature neonatal simulator and recordedpressuremeasurement: PIP Vt |
SIB generated more PIP and tidal volume (Vt) than the Neopuff™. Professional experiencehad no significantimpactonthelevel and thevariability of Vtor PIP provided. |
| Bassani et al. (2012), [17] |
Professional work in neonatal intensivecare: Physicians Residentphysicians Physiotherapists Nurses Nursingtechnicians |
Self-inflating bag | Use a test lung (adjustedtosimulatethelungs of anintubatedtermnewborn. Use 5 differenthandlingtechniques. Evaluatedwhetherthe manual technique and theuser’sprofessionaffected positive pressureventilation in terms of PIP, Vt, and ventilatoryfrequency. |
Profession had an influence on the Vt and respiratory rate. Therapists delivered significantly greater values for these parameters than the other professionals did. Most of the professionals delivered pressures and volumes that exceeded recommendations, combined with insufficient respiratory rates. |
| Szyld et al. (2012), [18] |
Professional work in neonatal intensivecare: divided in twogroupsaccordingtoexperience:
Group 1 (experts): professionalswithlessthan 5 years in practice. Group 2: (Beginners) Includedprofessionalswithlessthan 5 years of experience. |
Self-inflating bag Neopuff™ |
Neonatal reanimationsimulator. Evaluatedtheprecision of thepressureadministeredbyprofessionals and itsrelationshipwiththeoperator'sexperience. |
Significantdifferences in therespiratoryrate, whichwashigherthanrequiredwhenventilationwasprovidedbytheinexperiencedstaff. The T-pieceprovidedlower PIP whileboth SIB, higherthan the target. Both SIB and noviceparticipantswere associatedwithhigher VR. |
| Prado et al. (2013), [19] |
Trained and non-trained medical professionalswerestudied. | Self-inflating bag T-pieceresuscitatorBabypuff™ |
Comparedtheinfluence of professionalexperience and training onthevariability and effectiveness of manual ventilation. Abilitytoperform a sustainedinflation Lung. Use intubatedmannequin and recordeddeliveredpressure: PIP and PEEP and Vt. |
No influence of professional training on the effectiveness of the ventilation. |
Table 2: Summary of comparative studies including the positive pressure ventilation devices.
Unlike these studies, which generally included neonatal care unit staff and with expertise in neonatal resuscitation, we evaluated the devices when used by students with no experience in neonatal care. Similar to these studies, we found that the SIB did not generate PEEP in reliable ranges, even with the use of the PEEP valve. However, we did not find excessive PIP at hazardous levels with any of the devices evaluated, unlike the studies mentioned above. The studies have not included alternatives to NEOPUFF such as the disposable T-piece resuscitator. We found, that the disposable T-piece resuscitator (Neo-Tee®) was the safest and most effective device in terms of pressures compared with the SIB and the flow-inflation bag.
In our study, as in some of the mentioned, we found problems with the required respiratory rate; regardless of the device used, none of the evaluated practitioners administered frequencies in the required ranges, and all rates were well below recommendations. The literature indicates that the user’s profession, experience, and expertise influence the respiratory rate administered during neonatal resuscitation. Morley and his team [16] found that PEEP in self-inflating resuscitation bag with PEEP valve varied in relation to the respiratory rate. At a respiratory rate of fewer than 20 per minute, PEEP decreased more frequently than when respirations were administered at 60 times per minute since the pressure drops over time. The PEEP delivered was unrelated to the gas flow into the device. Dawson and his team [17] when comparing SIB, flow-inflating bag and T-piece resuscitator, found that each device was able to provide PEEP, but this in relation to the correct use of the device; but the device that provide most accurate PEEP was the T-piece resiscitator. Given the findings of our study and others with respect to operator experience, we recommend strengthening the training of first-level personnel in the use of the devices, particularly in terms of the frequency with which the respirations are administered, to improve the PPV technique.
One limitation of the study was that it did not include the NEOPUFF device, which according to the literature seems to be the safest and most reliable option in neonatal resuscitation in the delivery room. With the methodology proposed in the present study it was possible to accurately measure the quality of the ventilation pressures of the evaluated devices. Measured pressures for the disposable T-piece resuscitator are similar to those measured in the NEOPUFF studies. In addition, the NEOPUFF for the 1 and 2 level care centers is not available in our environment and therefore was beyond the scope of the study, which was to compare available devices in first-level care. Adapting neonatal resuscitation recommendations to settings with limited resources, especially in poor countries, where approximately 90% of neonatal deaths occur, would decrease neonatal morbidity and mortality.
Conclusion
The disposable T-piece resuscitator is safe and effective for the ventilation of newborns when it is used by trainees who are inexperienced in handling critical newborns and are evaluated using a simulator; and can be used as an alternative ventilation device in firstand second-level settings. The respiratory rate achieved is related to the personnel’s training and expertise. The adaptation of the ILCOR recommendations to the contexts of countries with limited resources should be continued as a cost-effective measure in neonatal care.
Acknowledgements
We gratefully acknowledge the assistance of the medical students, the paediatrics service, and the Clínica Universidad de La Sabana.
Sources of Funding
None
Disclosures
None
What is already known on this topic?
Approximately 10% of newborns require neonatal resuscitation at birth; positive pressure ventilation (PPV) is the most common intervention used for newborn resuscitation.
Neopufftm it the most effective and safest device. The availability of Neopuff in health centers of 1 and 2 levels with limited economic resources is null.
The self-inflating bag is the most frequently used device, and its effectiveness depends on the operator’s profession and experience.
What this study adds
Disposable T-piece resuscitator delivered pressures (PIP and PEEP) within the range of safety.
The use of this device by non-expert trained personnel can improve respiratory assistance for the neonate.
Can be a possible cost-effective alternative in level I and II health care settings with limited economic resources.
References
- Polin RA, Fox WW, Abman SH. Fetal and Neonatal Physiology. Fourth Edition Vol 1. Philadelphia: Elsevier Saunders (2011).
- Wyckoff MH, Aziz K, Escobedo MB, et al. Neonatal Resuscitation 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation.132 (18), 543-560 (2015).
- Perlman JM, Risser R. Cardiopulmonary resuscitation in the delivery room: Associated clinical events. Arch Pediatr Adolesc Med 149(1), 20-25 (1995).
- Carbine DN, Finer NN, Knodel E, et al. Video Recording as a Means of Evaluating Neonatal Resuscitation Performance. Pediatrics 106(4), 654-658 (2000).
- Kattwinkel J, Perlman JM, Aziz K, et al. Neonatal Resuscitation: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 122(18), 909-919 (2010).
- Hooper S, Pas TA, Lewis R, et al. Establishing functional residual capacity at birth. Neo Reviews 11(9), 474-483 (2010).
- Leone TA, Finer NN, Rich W. Delivery Room Respiratory Management of the Term and Preterm Infant. Adv Respir Care Newborn 39(3),431-440 (2012).
- Augustine JA, Seidel DR, McCabe JB. Ventilation performance using a self-inflating anesthesia bag: Effect of operator characteristics. Am J Emerg Med 5(4),267-270 (1987).
- Finer NN, Rich W, Craft A, et al. Comparison of methods of bag and mask ventilation for neonatal resuscitation. Resuscitation 49(3),299-305 (2001).
- Hussey SG, Ryan CA, Murphy BP. Comparison of three manual ventilation devices using an intubated mannequin. Arch Dis Child Fetal Neonatal Ed 89(6), 490-493 (2004).
- Roehr CC, Kelm M, Fischer HS, et al. Manual ventilation devices in neonatal resuscitation: Tidal volume and positive pressure-provision. Resuscitation 81(2),202-205 (2010).
- Bennett S, Finer NN, Rich W, et al. A comparison of three neonatal resuscitation devices. Resuscitation 67(1), 113-118 (2005).
- Kanter RK. EValuation of mask-bag ventilation in resuscitation of infants. Am J Dis Child 141(7), 761-763 (1987).
- http://www.who.int/maternal_child_adolescent/documents/basic_newborn_resuscitation/en/
- Barcikowski RS, Robey RR. Sample Size Selection in Single Group Repeated Measures Analysis (1985).
- Morley CJ, Dawson JA, Stewart MJ, et al. The effect of a PEEP valve on a Laerdal neonatal self‐inflating resuscitation bag. J Paediatr Child Health 46(1‐2),51-56 (2010).
- Dawson JA, Gerber A, Kamlin COF, et al. Providing PEEP during neonatal resuscitation: Which device is best? J Paediatr Child Health 47(10), 698-703 (2011).