Research Article - Clinical Practice (2021) Volume 18, Issue 6
Comparison of Mulligan SNAG's and neural tissue mobilization in patients with lumbar radiculopathy: A randomized controlled trial
- Corresponding Author:
- Saad Shafiq
University institute of Physical Therapy
University of Lahore Islamabad Campus, Pakistan
E-mail: saadshafiq11@gmail.com - Anderson PA, McCormick PC, Angevine PD. Randomized controlled trials of the treatment of lumbar disk herniation: 1983-2007. J Am Acad Orthop Surg. 16, 566-573 (2008).
- Machado LAC, Maher CG, Herbert RD, et al. The McKenzie method for the management of acute non-specific low back pain: design of a randomized controlled trial. BMC Musculoskelet Disord. 6, 50 (2005).
- Koes BW, van Tulder MW, Peul WC. Diagnosis and treatment of sciatica. BMJ. 334, 1313-1317 (2007).
- Schoenfeld AJ, Weiner BK. Treatment of lumbar disc herniation: Evidence-based practice. Int J Gen Med. 3, 209-214 (2010).
- Atlas SJ, Keller RB, Chang Y, et al. Surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: five-year outcomes from the Maine lumbar spine study. Spine. 26, 1179-1187 (2001).
- Kreiner DS, Hwang SW, Easa JE, et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J. 14, 180-191 (2014).
- Atlas SJ, Chang Y, Kammann E, et al. Long-term disability and return to work among patients who have a herniated lumbar disc: the effect of disability compensation. J Bone Joint Surg Am. 82, 4-15 (2000).
- Airaksinen O, Brox JI, Cedraschi C, et al. Chapter 4 European guidelines for the management of chronic non-specific low back pain. Eur Spine J. 15, s192-s300 (2006).
- Vicenzino B, Paungmali A, Teys P. Mulligan's mobilization-with-movement, positional faults and pain relief: Current concepts from a critical review of the literature. Man Ther. 12, 98-108 (2007).
- Schafer A, Hall T, Muller G, et al. Outcomes differ between subgroups of patients with low back and leg pain following neural manual therapy: a prospective cohort study. Eur Spine J. 20, 482-490 (2011).
- Davidson M, Keating JL. A comparison of five low back disability questionnaires: reliability and responsiveness. Phys Ther. 82, 8-24 (2002).
- Pfirrmann CW, Dora C, Schmid MR, et al. MR image-based grading of lumbar nerve root compromise due to disk herniation: reliability study with surgical correlation. Radiology. 230, 583-588 (2004).
- Moorthy, Pradnya. ~ 24 ~ Efficacy of mulligan snag technique for the management of spondylogenic referred low back pain. Indian J Phys Ther. 3, 24-28 (2015).
- Hussien HM, Abdel-Raoof NA, Kattabei OM, et al. Effect of mulligan concept lumbar SNAG on chronic nonspecific low back pain. J Chiropr Med. 16, 94-102 (2017).
- Boyd BS, Wanek L, Gray AT, et al. Mechanosensitivity of the lower extremity nervous system during straight-leg raise neurodynamic testing in healthy individuals. J Orthop Sports Phys Ther. 39, 780-790 (2009).
- Efstathiou MA, Stefanakis M, Savva C, et al. Effectiveness of neural mobilization in patients with spinal radiculopathy: a critical review. J Bodyw Mov Ther. 19, 205-212 (2015).
Abstract
Background: Radiculopathy usually comes from sciatic origin; if the sciatic nerve gets irritated due to compression then it causes pain in course of the nerve called sciatic radiculopathy. Disc herniation of L4-L5 and L5-S1 segments is the most common and sometimes irritates the sciatic nerve a condition known as Sciatica. The sign symptoms of sciatic radiculopathy have radicular pain in the lower leg following the course from the low back, buttock area and back of thigh followed by weakness of muscle and sensory involvement may be deep tendon reflex are diminished. Objective: The objectives of the study were to compare the effectiveness of two nonsurgical treatment strategies in patients with lumbar radiculopathy; to enhance the evidence-based treatment. Methodology: The study was a Randomized Control Trial (RCT), conducted in the Outpatient Department of Jinnah teaching hospital Gujranwala and LifeCare Physiotherapy and Rehabilitation Center from February 2017 to December 2017. The sample of the study consisted of 48 patients male (n=16) and female (n=32). Patients with diagnosed L4-L5/ L5-S1 disc pathology and radicular pain and confirmed from MRI were recruited for this study. An ethical approval letter was received from an institution for study. The sample size was estimated with 90 percent power and effect size of 1.01 at a significance level of 0.05 (α) came out to be 48 i.e. 24 patients in each group. Groups included in the study were: Group A: Mulligan SNAG’s Technique plus Ultrasound and Short Wave Diathermy. Group B: Neural mobilization technique plus Ultrasound and Short Wave Diathermy. Tools used for data collection are the Numeric Pain Rating Scale (NPRS), Lumber Range of Motion (ALROM), and Modified Oswestry Disability Index (MODI) questionnaire. Results: The mean change across NPRS in a group of mulligan mobilization was 6.167 as compared to 5.583 in the neural mobilization group. The mean change across MODI in a group of mulligan mobilization was 47.667 as compared to 49.667 in the neural mobilization group. Conclusion: Neural mobilizations are more effective as compared to mulligan techniques in reducing pain while mulligan mobilization seems to be more beneficial for the improvement of disabilities.%.
Keywords
mulligan mobilization, neural mobilization, lumbar radiculopathy, MODI, NPRS
Introduction
In the age group of young and middle-aged people, spinal issues are most common, in these issues commonest issue is disc herniation. The lumbar Intervertebral Disc (IVD) is a very complex structure in manufacturing. IVD is made up of proteoglycans, collagens, and fibro chondrocytes that serve to divide the forces exerted on the spine during weight-bearing [1].
Per Year cost of treatment of disc-related low back pain in the USA is thirty-one billion dollars [2]. The most common direction of herniation of the lumbar disc is posterior and lateral, it causes nerve compression of the same side which leaves at the level of the dural sac that mainly causes a problem in the L4-L5 segment and L5- S1 root level. It may cause Radiculopathy or may be present as localized symptoms [3].
Radiculopathy usually comes from sciatic origin; if the sciatic nerve gets irritated due to compression then it causes pain in course of the nerve called sciatic radiculopathy. The course of radiation of this pain is typically from the lower back to the posterior part thigh and radiating down below the knee joint posteriorly [4].
Sciatic nerve radiculopathy causes shooting pain, a sense of burning, numbness of the supplied area, or tingling sensation from the low back area and outer upper buttock quadrant down to the back of the thighs and leg.
Severity sciatic radiculopathy makes walking difficult. Symptoms of sciatic radiculopathy are sometimes aggravated by movement of the lower limb and bending at the lumbar region, usually relieved by making the spine weight free or by lying down [5].
Diagnosis of radiculopathy is usually correlated with physical examinations of the patient and medical history. Typically, radicular symptoms and certain examination procedures assist healthcare professionals to diagnose sciatic radiculopathy. Sometimes, X-rays and other tests like CT scans, Magnetic resonance imaging, and EMG study are used for further evaluation to find out the exact causes of radiculopathy [6].
Sciatic Radiculopathy results in nerve irritation that causes pain along the pathway of the nerve. The sciatic pain incidence is 5 in 1000 yearly. The sign symptoms of sciatic radiculopathy have radicular pain in the lower leg following the course from the low back, buttock area and back of the thigh followed by weakness of muscle and sensory involvement may be deep tendon reflex are diminished. Treatments of sciatic radiculopathy depend on its severity and cause of nerve irritation [7].
There are many etiological factors of lumbar pain, with or without going with Radicular manifestations, constituting idiopathic, degenerative, trauma-related, inflammatory, inherent, neoplastic, metabolic, postural and gynecological, rectal, or rectal fundamental pathologies [8]. Lumbar radiculopathy might be depicted as sharp pain starting in the area of the lower back and spread into one or both lower appendages. It as a rule takes after particular dermatomal dissemination, demonstrating the level of spinal nerve root contribution. Tactile side effects are annoying for patients, regularly comes with paresthesia’s, deadness; Structural manifestations incorporate muscle shortening, decreased profound ligament contour.
Lumbosacral radiculopathy is a very debilitating type of pain as it can limit daily activities as well, even leads to disability in some patients. Lumbar plate herniation with radiculopathy might be characterized as restricted uprooting of disc material and the typical edges of the intervertebral disc space bringing about low back sharp pain, or potentially shortcoming, paresthesia or deadness in a myotomal or, then again dermatomal distribution [9].
Manual therapy as a treatment option has always seemed to be the best intervention for the management of pain and in both neural and nonneural types of disc-related lower back pain, the functional outcomes of this technique are very good as well [10]. Mulligan’s spinal mobilization is the most favorably used technique as it seems to be very beneficial in dysfunction of spinal joints as well as neurodynamics abnormality [11]. Many varieties of exercise are available as treatment options strategies for low back pain. Exercise includes Flexion bias and Extension bias exercises. Inflection bias William flexion exercises are the recommendation. In the Extension bias plan, McKenzie exercises are the choice of treatment [6].
Therefore, the objective of this study was to compare the effectiveness of two nonsurgical treatment strategies in patients with lumbar disc-related Radiculopathy.
Methodology
■ Study design
Randomized Control Trial (RCT).
■ Settings
Conducted in the Outpatient Department of Jinnah teaching hospital Gujranwala and Life Care Physiotherapy and Rehabilitation center.
■ Duration
From February 2017 to December 2017.
■ Sample size
The sample of the study consisted of 48 patients. The sample size was estimated by using G Power 3.1.7 software at 90 percent power and the effect size of 1.01 at a significance level of 0.05 (α) came out to be 48 i.e. minimum 24 in each group.
■ Sampling technique
Non-probability consecutive sampling
■ Sample Selection
Inclusion criteria
▪ Age 25-55 years.
▪ Pain radiate from the lower lumbar area to the posterior aspect of the leg up to the plantar surface of the toes. Grade 0 (normal), Grade 1 (contact), Grade 2 (deviation), Grade 3 (compression) [12]
▪ Patient with confirmed L4-L5, L5-S1 disc herniation in diagnostic MRI
▪ The numeric pain rating scale value is more than 4
Exclusion criteria
Any red flags (tumor, fracture, metabolic diseases, rheumatoid arthritis, osteoporosis, Prolong History of hypertension), Pregnancy, Prolong use of steroids, and Lumbar spondylolisthesis.
■ Tools
Tools used for data collection were the Numeric Pain Rating Scale (NPRS), Lumber Range of Motion (ALROM), and Modified Oswestry Disability Index (MODI) questionnaire.
■ Study groups
Groups included in the study are Group A: Mulligan SNAG’s Technique +U/S and Short Wave Diathermy. Group B: +Neural mobilization technique U/S and Short Wave Diathermy.
The sample of the study consisted of 48 patients with male (n=16) and female (n=32) both, have a referral to the outpatient department of physiotherapy in Jinnah Hospital Gujranwala and Life Care Physiotherapy and Rehabilitation Center. Patients with diagnosed L4-L5/L5- S1 disc pathology and radicular pain and confirmed from MRI were recruited for this study. An ethical approval letter was received from the institution for study.
Data Analysis
The data were analyzed using SPSS for Windows software, version 17. Statistical significance will be set at p=0.05. Frequency tables, pie charts, bar charts will be used to show a summary of group measurements measured over time. An independent sample t-test was used for differences between groups. Non-parametric test that is used to compare two populations at different various intervals.
Results
There were 50% (n=12) males and 50% (n=12) females in mulligan SNAG’s group compared to 41% (n=10) males and 58% (n=14) females in Neural mobilization group. The mean age of participants in the Mulligan SNAG group was 35 and in the neural mobilization group was 40 years. There was a significant reduction in pain within each group with a p-value <0.05. The mean difference in NPRS score within Mulligan SNAG’s group from pre-treatment to week 4 was 6.167 similarly the mean difference in MODI score within Neural mobilization’s group from pre-treatment to post-treatment (week 4) was 5.583. There was a significant reduction in disability within each group with a p-value <0.05. The mean difference in MODI score within Mulligan SNAG’s group from pre-treatment to post-treatment (week 4) was 47.667 similarly the mean difference in MODI score within Neural mobilization’s group from pre-treatment to week 4 was 49.667 (TABLE 1 AND TABLE 2).
| Study Group | Frequency | Percent | |
|---|---|---|---|
| Mulligan SNAG's | Male | 12 | 50 |
| Female | 12 | 50 | |
| Total | 24 | 100 | |
| Neural Mobilization | Male | 10 | 41.7 |
| Female | 14 | 58.3 | |
| Total | 24 | 100 | |
TABLE 1. Table Summarizes the Gender of Participants of Study.
| Treatment Week | F | Sig. (p value) |
|---|---|---|
| NPRS Pretreat | 0.013 | 0.909 |
| NPRS. W1 | 4.296 | 0.044 |
| NPRS. W2 | 5.921 | 0.019 |
| NPRS. W3 | 0.51 | 0.479 |
TABLE 2. Across group comparison of NPRS (Numeric Pain Rating Scale).
An independent sample T-test was applied to determine any significant difference between post-treatment NPRS at W1, W2, and W3. Results showed no significant difference across these two groups with a p-value >0.05 (TABLE 3).
| Treatment Week | Sig. (p value) |
|---|---|
| MODI. Pre Treatment | 0.634 |
| MODI. W1 | 0.469 |
| MODI. W2 | 0.362 |
TABLE 3. Across group comparison of MODI (Modified Owestry Disability Index).
An independent sample T-test was applied to determine any significant difference between post-treatment MODI at W1, W2, and W3.
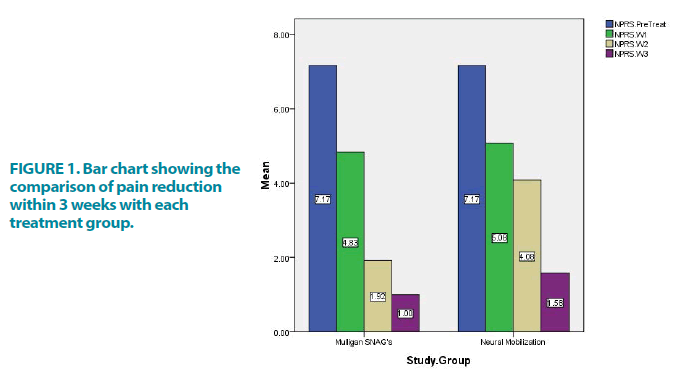
Results showed no significant difference across these two groups with a p-value >0.05 (FIGURE 1).
This bar chart shows the comparison of pain reduction within 3 weeks within each treatment group. There was a significant reduction in pain within each group with a p-value <0.05.
The mean difference in NPRS score within Mulligan SNAG’s group from pre-treatment to week 4 was 6.167 similarly the mean difference in MODI score within Neural mobilization’s group from pre-treatment to week 4 was 5.583.
Discussion
Moorthy et al. done a pilot study in 2015 on 15 patients, he had worked on the efficacy of mulligan SNAGs for the spondylogenic referred pain management in the lower back. The interventional group was treated with mulligan SNAG’s and exercises. Oswestry disability index and Visual Analogue Scale was used in this study as a measuring tool. Change in percentage of a score of post-intervention was also found to be significant in both groups i.e. 16.4% 31.3% p-value 0.001. He concluded that Mulligan SNAG’s proven to be beneficial for short-term disability and pain [13].
Hussien et al. in 2017 done their research on the efficacy of the mulligan concept of lumbar SNAG’s on nonspecific back pain. 42 participants were randomly allocated into 2 groups. The interventional group receives conventional treatment with sustained natural apophyseal glide and the control group underwent conventional treatment without SNAG’s. One-month treatment time with 3 sessions in a week. Pain and function measure by an Isokinetic Dynamometer, VAS, and modified ODI scales were used as measuring tools. Both groups have significant improvement However, the interventional group has more long-lasting and significant results because of adding SNAG’s too conventional methods [14].
Boyd et al. conducted a study in 2009 he concluded that neuro-dynamics techniques seemed to be very beneficial for the activation of distal muscle [15]. Efstathiou et al. did a systematic review for the effectiveness of neural mobilization in lumbar radiculopathy. His results show that neural mobilization is effective for the management of lumbar radiculopathy [16]. The mean change across NPRS in a group of mulligan mobilization was 6.167 as compared to 5.583 in the neural mobilization group. For Lumber flexion, lumbar extension, right side bending, and left side bending in a group of mulligan mobilization group was 9.500, 4.167, 3.000, and 7.750 respectively while in Group of neural mobilization lumbar flexion, lumbar extension, right side bending, and left side bending mean change was 5.417, -1.500, 3.833 and 5.500 respectively. The mean change across MODI in a group of mulligan mobilization was 47.667 as compared to 49.667 in the neural mobilization group.
The results of this study show that Mulligans SNAG is more useful than neural mobilization. As the pairwise comparison of MODI and NPRS clearly shows that in the mean differences that there were more improvements in Mulligan’s SNAG group than of neural mobilizations’ group.
Conclusion
Neural mobilizations are effective as compared to mulligan techniques in reducing pain while mulligan mobilization seems to be more beneficial for the reduction of disabilities.
Recommendations and Limitations
There was some limitation in this study due to certain factors. As a true control group is not present in this study so it seemed to be difficult for differentiation in nature of disorder and effects of the treatment, so the internal validation might be challengeable. As a small sample size was taken in the study it may risk the validation and generalization of results. Prolonged effects cannot be assessable because of the short time duration. It is recommended that post-treatment observation could be for a long time duration. More RCT requires knowing the efficacy of the particular techniques even on radicular and non-radicular back pain.