Research Article - Clinical Practice (2023) Volume 20, Issue 4
Comparative study of airway assesment scoring of modified mallampatti versus cormack and lehane grading by video laryngoscope
- Corresponding Author:
- Tarun Kumar Yadav
Department of Obstetrics and Gynecology, Government Medical College, Ambedkar Nagar, UP, India
E-mail: shikhatarun15@gmail.com
Received: March 07, 2023, Manuscript No. FMCP-23-91076; Editor assigned: March 10, 2023, PreQC No. FMCP-23-91706 (PQ); Reviewed: March 25, 2023, QC No. FMCP-23-91706; Revised: May 10, 2023, Manuscript No. FMCP-23-91706 (R); Published: May 18, 2023, DOI: 10.37532/2044-9038.2023.20(4).1-9
Abstract
Background: The unanticipated difficult laryngoscopic intubation places the patient at increased risk of complications ranging from sore throat and serious airway trauma to aspiration of gastric contents. This study was undertaken to compare the modified mallampatti scores with cormack and lehane scoring by video laryngoscope and to find the correlation of modified mallampatti scoring with cormack and lehane scoring through video laryngoscope.
Methodology: This cross sectional was conducted in the department of anaesthesiology and CCM, Nehru hospital, BRD medical college, Gorakhpur, U.P. India. Patients aged between 18-65 years of either gender belonging to ASA grade I and II, undergoing elective procedure from all surgical specialities requiring endotracheal intubation by anaesthetics video laryngoscopy were enrolled.
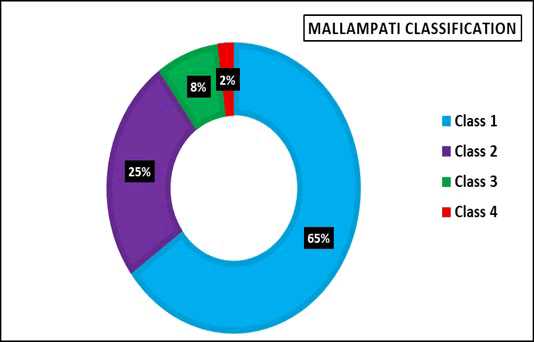
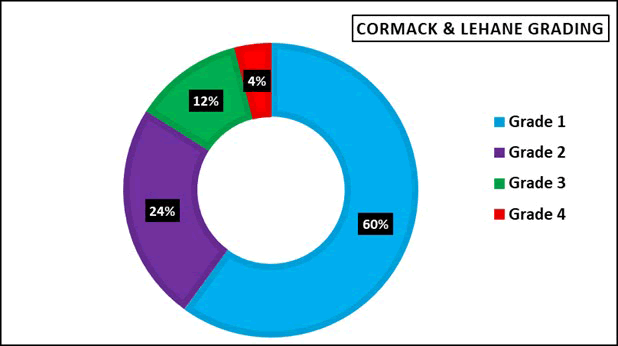
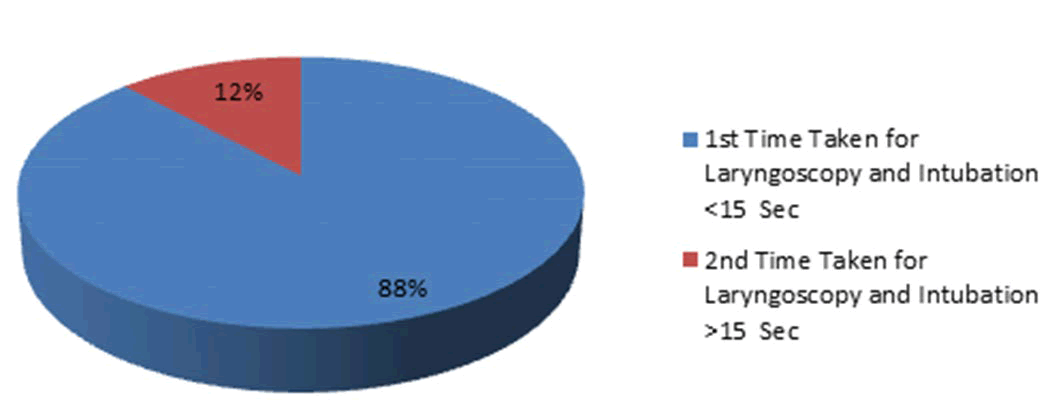
Results: Out of 100 cases 78 (78%) patients were females and 22 (22%) were males. The cases with ASA grade I and II were in proportion 54% and 46% respectively. According to mallampati classification the majority of cases were with class 1 (65%), class 2 (25%), class 3 (8%) and class 4 (2%) respectively. According to Cormack and Lehane grading the majority of cases belonged to grade 1 (60%), grade 2 (24%), grade 3 (12%) and grade 4 (4%) respectively. Out of 100 cases the modified mallampati and CL grading shows same level correlation in 71 cases while in 29 cases it was different or non-correlated. Eighty eight cases had time taken less than 15 seconds while 12 cases took more than 15 seconds for laryngoscopy and intubation.
Conclusion: Modified mallampati scoring and cormack and lehane grading is a good predictor for tracheal intubation. Despite of video laryngoscopy use the modified mallampati classification did not correl ate grade to grade with cormack and lehane grading in all cases. Regular use of video laryngoscopy may improve the overall ease of intubation.
Keywords
Modified mallampati scoring, Cormack and lehane grading, Laryngoscopic, Anaesthesia, Trauma
Introduction
The term airway management is the cornerstone of anaesthesia [1]. Direct laryngoscopic intubation is difficult in 1%-4% cases and impossible in 0.05%-0.35% of patients who have seemingly normal airways [2].The unanticipated difficult laryngoscopic intubation places the patient at increased risk of complications ranging from sore throat and serious airway trauma to aspiration of gastric contents [3,4]. Failure to intubate the trachea is even less common, being 1:2302 in the non-obstetrics population and 1:300 in obstetric patients [5,6].
Mallampatti proposed a score to correlate the oropharyngeal space with the predicted ease of direct laryngoscopy and endotracheal intubation. With the observer at eye level, the patient holds the head in neutral position opens the mouth maximally and protrudes the tongue without phonating mallampati and associates described a clinical sign to predict difficult tracheal intubation based on the size of the base of the tongue [7]. A mallampati classification of I to III is assigned, based on the visibility of the faucial pillars, uvula and soft palate when the patient is seated upright with the head neutral, the mouth open, the tongue protruded and no phonation. The modified mallampati classification is the most commonly used airway assessment test in current anaesthesia practice and is defined as follows: Class I: Faucial pillars, uvula and Soft palate are visualized, class II: Base of uvula and soft palate are visualized, class III: Soft palate only is visualized and class IV: Hard palate only is visualised. A mallampati zero classification has been proposed when the epiglottis can be visualized during examination of the oropharynx; this finding is usually associated with easy laryngoscopy [8,9].
The commonly used tests for airway evaluation are mallampati classification, cormack and lehane grading, thyromental distance and tests devised by Wilson. Cormack and lehane classified the view at laryngoscopy in four grades based on visualization of glottis and epiglottis. The grades range from I to IV, beginning with grade I (the best view), in which the epiglottis and vocal cords are in complete view, and culminating with grade IV (the most difficult view) in which the epiglottis and the larynx cannot be visualized.
Tracheal intubation by video laryngoscope is the most innovative advancement. Intubation with video laryngoscope is successfully done in shorter time as compared to conventional direct laryngoscopy with Macintosh laryngoscope [10]. The video laryngoscope is provides an enlarged video image of airway structures [11]. Video laryngoscpoe has been shown to improve glottic visualisation, compared with direct laryngoscopy, in both routine management and in the predicted difficult airway. Intubation success rates of 94% and 99% have been reported for video laryngoscopy as a rescue modality after failed direct laryngoscopy [12,13]. Video laryngoscopy is now included in the ASA difficult airway algorithm as an alternative approach to intubation and should be considered for patients with known or predicted difficult airway [14].
Advantages of video laryngoscopy are improved laryngeal visualisation because eyes and airways need not be lined up as in direct laryngoscopy, less force is used than during direct laryngoscopy, less cervical spine movement and possibly less hemodynamic stress response to the laryngoscopy and intubation.
The technique is considered one of the major advances in anaesthesia practice during recent years, the role of VL in difficult intubation scenarios has recently been recognized in both ASA and DAS guidelines [15-17]. Today there is a number of commercially available video laryngoscopes with advantages or disadvantages depending on the situations the clinicians have to manage [18]. Among them the storz C-MAC (Karl Storz GmbH and Co. KG, Twittling, Germany) was the first macintosh type laryngoscope, in corporating the features of a conventional and video laryngoscope in one device. The manipulation of the blade to the oral and pharyngeal structures and the technique of laryngoscopy is identical to conventional macintosh blade laryngoscopy. However, when the conventional laryngoscopy results in poor glottis view, due to inability to align the oral, pharyngeal and laryngeal axes, C-MAC can be used as a video laryngoscope. In this case a midline insertion technique without sweep of the tongue can achieve an unobstructed view in the vertical axis and 800 field of view in the horizontal axis [19].
A metaanalysis including 16 articles confirmed that in difficult airways the storz C-MAC showed superior success rates glottic visualization and less external larymgeal manipulations compared to macintosh [20]. Nevertheless despite different video laryngoscope “success story”, including storz C-MAC, the problem of failed intubation could not be fully eliminated upto now, the technique of awake fiberoptic intubation under local anaesthesia and mild sedation for the management of an anticipated difficult intubation is considered the safest. With the above background this study was undertaken to compare the modified mallampatti scores with cormack and lehane scoring by video laryngoscope and to find the correlation of modified mallampatti scoring with cormack and lehane scoring through video laryngoscope.
Materials and Methods
The prospective observation study was conducted on adult patients aged between 18-65 years old of either gender belonging to ASA grade I, and II, undergoing elective procedures from all surgical specialties requiring endotracheal intubation at Nehru hospital, BRD medical college, Gorakhpur. The permission of ethical committee was taken. Written informed was taken from all patients on a separate consent form. The Study period was from 1st December 2019 to 30th November 2020.
Sample size was calculated by the formula:
P=50% successful predictions by mallampatti scoring system
Q=100-P=50, Sample size: N=4pq/LxL, N=4 x 50 x 50/10 x 10, N=100 and L=Allowable error 10%
Inclusion criteria: Patient with American Society of Anesthesiologist (ASA) grade I and II are included. Patient aged between 18 to 65 years of either gender were included. Patients undergoing elective procedures from all surgical specialities requiring endotracheal intubation.
Exclusion criteria: Patient refusal, emergency surgical procedures, pregnant patients, patients with unstable cervical spine. Patients with tumor of larynx, Patients with apparent restriction of mouth opening due to pain, with fresh facial injuries, Patients with apparent restriction of neck movement. Patients pre anesthetic checkup and airway assessment was done and MP score noted in pre anesthetic checkup room before surgery. A through preanaesthetic evaluation was conducted in PAC clinic. Airway was assessed using modified mallampati score with the patients in sitting position the mouth fully open and the tounge protruded examiner is also sit at the same level in front of patient.
In the Operation Theatre (OT) standard monitor were attached. Patient was place supine on OT table and all preparations done for laryngoscope and intubation. Pulse oximeter, 5 lead ECG and noninvasive blood pressure, base line measure of B.P., heart rate and oxygen saturation were done. Vital signs were recorded from the time of induction of anaesthesia was begun until patient had been intubated. Before induction of anaesthesia all patients were given inj. Glycopyrolate (10 μg/kg) IV, inj. Fentanyl (1.5 μg/kg) IV, general anaesthesia was induced by using inj. Propofol (2-3 μg/kg) IV. The patient’s head was placed in the “sniffing position”. Once the ability to mask ventilation of pt. was confirmed followed by inj. Vecuronium (0.1 mg/kg) IV induced muscle relaxation. Sevoflurane/Isoflurane was used for maintainance of anaesthesia patient was ventilated via the anaesthesia mask for 3 minute with 100% oxygen until complete relaxation was achieved. All patients were given assisted ventilation with 100% oxygen via face mask followed by laryngoscopy after three minutes of muscle relaxant. An appropriate size of video laryngoscpoe blade was used during laryngoscopy. The cormack and lehane grading is assessed and noted prior to intubation by the trained anaesthesiologist. Correct placement of endotracheal tube was confirmed by the auscultation and end tidal carbon dioxide.
Indirect laryngoscopy is performed whenever the provider visualizes the patient’s vocal cords by a means other than obtaining a direct line of sight. For the purpose of intubation, this is facilitated by fiberoptic bronchoscopes, video laryngoscopes, fiberoptic stylets and mirror or prism optically enhanced laryngoscopes .
For our study anaesthetist video laryngoscope blade of size 3 and 4 were used. Size of the blades and tracheal tubes (7.0-8.5 mm ID) were used at discretion of the intubating anaesthesiologist. After endotracheal intubation further anaesthesia management was continued as per the need of the patients. All information recorded on the working performa and kept strictly confidential and stored in data log book.
Duration of laryngoscopy and intubation: It is defined as time taken from insertion of the laryngoscope blade between the teeth until the endotracheal tube is placed through vocal cords as evidenced by visual confirmation on monitor screen by anaesthesiologist performing laryngoscopy.
Laryngoscopy and intubation using video laryngoscope. Although most video laryngoscope strongly resemble conventional direct laryngo scope, the significant advantages confirred by their video capability require an adjustment in techniques, with conventional direct laryngoscopy, the hands, devices and targets are all in “real world” line of sight and simple hand to eye coordination is required.
In video laryngoscopy, certain aspects are best performed in the same concrete spatial environment, while others capitalize on the superior view and access provided by the video image. It is important to distinguish which video laryngoscope steps works best using direct hand to eye coordination and which are best done in video environment. Accordingly, video laryngoscope was approached using 4 step technique: Introduce the laryngoscope, obtain the best view, Introduce the endotracheal tube and Intubate.
Statistical analysis: The results were analyzed using descriptive statistics and making comparisons among various groups. Categorical data were summarized as in proportions and percentages (%) while quantitative (discrete) data were summarized as mean ± SD.
The Chi Square test, the arithmetic mean, unpaired t test, paired t test, spearman correlation, sensitivity and specificity and kappa measure of agreement was applied. Data was collected and analysed through appropriate IBM SSPS version. Demographic and hemodynamic results were presented as mean ± standard deviation P<0.05 was considered as statistically significant.
Results
Out of 100 cases, 78 were females while 22 were males. The various diagnosis found were cholecystitis (59%), hernia (11%), appendicitis (4%), gall bladder stone (3%), goitre (3%) and renal stone (2%). The cases with ASA grade I and II were in proportion 54% and 46% respectively. The mean age of study cases was 38.28 ± 13.18 years with insignificant difference between correlated and non-correlated cases (p=0.838). Out of 100 patients cholecystitis patients were (59%), hernia (11%), appendicites (4%), gall blader stone (3%), goitre (3%), renal stone (2%) and others (18%).
The cases with ASA grade I and II were in proportion 54% and 46% respectively. According to modified mallampati classification, the cases with class 1, class 2, class 3 and class 4 were in proportion 65%, 25%, 8% and 2% respectively (FIGURE 1).
According to Cormack and Lehane grading, the cases with grade 1, grade 2, grade 3 and grade 4 were in proportion 60%, 24%, 12% and 4% respectively (FIGURE 2).
The modified mallampati score and CL garding showed same level in 71 cases while in 29 cases it was different. This resulted correlations in 71 cases while in 29 cases the levels were uncorrelated. The spearman correlations between the two score was perfect positive (ρ=1.000, p<0.001) in most of the cases while in non-correlated cases this correlation was 0.144 (p=0.456, non-significant) overall spearman’s correlation between mallampati and Cormack and lehane grading: ρ=0.680, p<0.001 (TABLE 1).
| Between MMP and CL | No. | % | Correlation | p-value | ||
|---|---|---|---|---|---|---|
| Correlation | Correlated | 71 | 71 | 1 | <0.001 | Significant |
| Non-correlated | 29 | 29 | 0.144 | 0.456 | Non-significant | |
Table 1. Distribution of cases according to correlation between modified mallampati and Cormack and Lehane grading (n=100).
The modified mallampati score and CL garding showed same level in 71 cases while in 29 cases it was different. This resulted correlations in 71 cases while in 29 cases the levels were uncorrelated. The spearman correlations between the two score was perfect positive (ρ=1.000, p<0.001) in most of the cases while in non-correlated cases this correlation was 0.144 (p=0.456, non-significant) overall spearman’s correlation between mallampati and cormack and lehane grading: ρ=0.680, p<0.001 (TABLE 2).
| MPS | CL Grading | Total | Kappa | Chi square | p-value | |||
|---|---|---|---|---|---|---|---|---|
| Grade 1 | Grade 2 | Grade 3 | Grade 4 | |||||
| Class 1 | 54 | 8 | 3 | 0 | 65 | 0.463 | 63.16 | <0.001 |
| Class 2 | 6 | 13 | 5 | 1 | 25 | |||
| Class 3 | 0 | 3 | 3 | 2 | 8 | |||
| Class 4 | 0 | 0 | 1 | 1 | 2 | |||
Table 2. Correlation between modified mallampati classes and Cormack and Lehane grading.
Mallampati and CL grading was matched in maximum 54 cases for grade/class 1 and minimum 1 case for grade/class 4. The measure of agreement between mallampati and CL grading was 0.463 and found to be highly significant (p<0.001) (TABLE 3).
| MPS with CL | Correlated | Non-correlated | Total | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Grade 1 | 54 | 90 | 6 | 10 | 60 |
| Grade 2 | 13 | 54.2 | 11 | 45.8 | 24 |
| Grade 3 | 3 | 25 | 9 | 75 | 12 |
| Grade 4 | 1 | 25 | 3 | 75 | 4 |
Table 3. Grade wise distribution of correlations between modiied mallampati and Cormack and Lehane scorings.
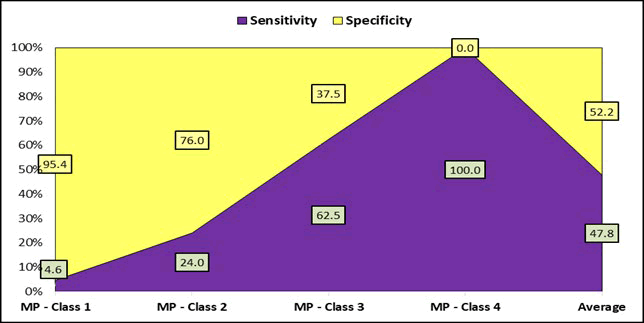
The grade wise distribution of correlations between mallampati and cormack and lehane scorings showed 90% correlation for grade 1, 54.2% for grade 2, 25% for grade 3 and 25% correlation for grade 4. So the correlation was maximum for grade 1 and minimum for higher grades 3 and 4 (TABLE 4 and FIGURE 3).
| Grades | Mallampati | ||||
|---|---|---|---|---|---|
| Class 1 | Class 2 | Class 3 | Class 4 | Average | |
| Cormack and lehane grades 3 and 4 (sensitivity) | 4.6 | 24 | 62.5 | 100 | 47.8 |
| Cormack and lehane grades 1 and 2 (specificity) | 95.4 | 76 | 37.5 | 0 | 52.2 |
Table 4. Sensitivity and specificity of mallampati classes.
Hence the maximum sensitivity was observed for class 4 and maximum specificity for class 1 (TABLE 5).
| No. of Attempts | Number of patients (n=100) | Percent (%) |
|---|---|---|
| One | 88 | 88.00% |
| Two | 12 | 12.00% |
Table 5. No. of attempts.
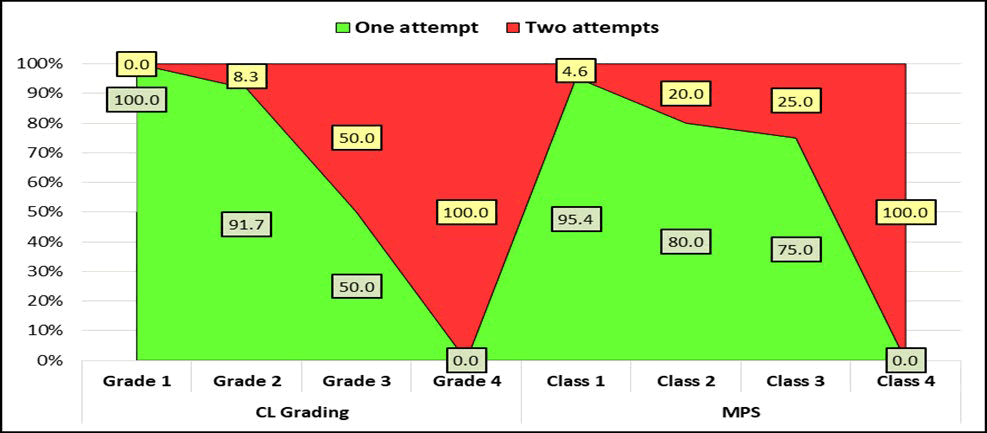
Only one attempt was required in majority 88 cases while in remaining 12 cases two attempts were needed. The significant difference was found in proportion of one and two attempts between various MPS Classes (p<0.001) (TABLE 6 and FIGURE 4).
Out of 100 cases 83 cases don’t required any added maneuver while 8 cases required Stylet, 7 needed BURP and two cases needed Bougie (TABLE 7 and FIGURE 5).
Majority 88 cases had time taken less than 15 sec for laryngoscopy and intubation while 12 cases took more than 15 sec for laryngoscopy and intubation.
| Difficulty in Intubation with added maneuver: BURP/Stylet/Bougie | Number of patients (n=100) | Percent (%) |
|---|---|---|
| Bougie | 2 | 2.00% |
| BURP | 7 | 7.00% |
| Stylet | 8 | 8.00% |
| Nil | 83 | 83.00% |
Table 6. Difficulty in intubation with added maneuver: Bougie/BURP/Stylet/Nil.
| Difficulty | No. | % | |
|---|---|---|---|
| Time taken for laryngoscopy and intubation | <15 sec | 88 | 88 |
| >15 sec | 12 | 12 | |
Table 7. Distribution of cases according to difficulty determinants.
Discussion
Failed intubation is a major cause of morbidity and death. Due to anaesthesia improvements in visualization of larynx using video laryngoscope may potentially increase success rate with laryngoscopy and intubation. Direct laryngoscopy using machintosh laryngoscope has been used for laryngoscopy and intubation since 1943. Video laryngoscope has been introduced to provide better laryngoscopic view on a video monitor and it can also potentially improve ease of intubation [10,11]. The use of video laryngoscope in intubation is well established and has been extensively supported in the literature for managing the difficult airway. With a direct laryngoscope it is necessary to obtain a line of site from the maxillary teeth to the glottis by placing the patients head on a pillow and extending the head on the neck (Sniffing position) to displace the tongue and epiglottis, which frequently obstructs the line of sight. In addition an assistant is frequently required to apply pressure to the thyroid cartilage to obtain a clear view of the glottis, and it is often difficult for the assistant to adjust the direction and the degree of the pressure. With a video laryngoscope because the image of the glottis is captured near the tip of the blade, only a few centimeters of line of sight will be required. In addition an assistant can adjust the direction and degree of pressure on the neck by confirming the improvement of the view of the glottis on a video screen. Therefore a video laryngoscope provides a better view of the glottis and would increase the success rate of tracheal intubation [13,14].
There have been anecdotal report of successful use of video laryngoscope in patients with difficult airways, in whom tracheal intubation with a macintosh laryngoscope had failed, in a case series of 270 adult patients in whom direct laryngoscopy using a macintosh laryngoscope had been difficult and in 23 patients with predicted difficult intubation and difficult mask ventilation, tracheal intubation with a video laryngoscope was successful in 290 of 293 patients. In addition randomised control studies including the study of Aziz, et al. have reported similar results. Comparing video laryngoscope with the macintosh laryngoscope in adult patients unanimously has shown a higher success rate of intubation with the video laryngoscope [15]. Therefore, it is clear that compared with a direct laryngoscope, video laryngoscope has a higher success rate of tracheal intubation in adult patients with difficult airways. Compared with a conventional laryngoscope a video laryngoscope would be less stressful to the patients, because the video laryngoscope is less likely to require extension and flexion of the head and neck, pressure on the neck and distortion of the upper airway [16]. The movement of the cervical spine during laryngoscopy with a video laryngoscope is less than with a macintosh laryngoscope. The video laryngoscope is less traumatic than the classic laryngoscope for a difficult airway among obese patients.
In our study the cases with ASA grade 1 and 2 were in proportion 54% and 46% respectively. According to modified mallampati classification the cases with class 1 (65%), class 2 (25%), class 3 (8%), class 4 (2%) respectively. According to Cormack and lehane grading the cases of grade 1 (60%), grade 2 (24%), grade 3 (12%) and grade 4 (4%) respectively. Out of 100 cases the modified mallampati and CL grading shows same level correlation in 71 cases while in 29 cases it was different or non-correlated i.e. 71 cases were matched for their modified mallampati class seen during PAC intubating same during video laryngoscopy, i.e. maximum correlation for grade 1 in 54 cases (90%), for grade 2 in 13 cases (54.2%) and minimum for grade 3 and 4 in (25%) cases. In Non-correlated cases out of 29 cases 6 cases (10%) of grade 1, 11 cases (45.8%) cases of grade 2, 9 cases (75%) in grade 3, and 3 cases (75%) in grade 4 [17]. The spearman´s correlation between MMP vs. CL grade for correlated cases was perfect positive (ρ=1.000, p<0.001) while in non-correlated cases this correlation was 0.144 (p=0.456) insignificant. Modified mallampati class and CL grading was matched maximum in 54 cases for class/grade 1 and minimum 1 case for class/grade 4. The measure of agreements between modified mallampati class and CL grading was 0.463 (Kappa value) and found to be highly siginificant (P<0.001) [18]. All cases of Cl grade 1 required only one attempt of intubation while for grade 2, 3 and 4 required one attempt in 91.7%, 50% and 0% cases. 95.4% of the cases of MPS class 1 required only one attempt of intubation while for classes 2, 3 and 4 required one attempt in 80.0%, 75% and 0% cases. Majority 88 cases had time taken less than 15 sec while 12 cases took more than 15 sec for Laryngoscopy and intubation.
Our results are comparable with the study done by Mallampati SR, et al. [19]. Two hundred and ten adult surgical patients (47 men and 163 women) of ASA status one and two are included in the study. A significant correlation exists between the ability to visualize pharyngeal structures and the ease of laryngoscopy (P<0.001). Results are highly significant (P<0.001) and supports the hypothesis that difficult laryngeal visualization can be predicted in most cases by eliciting the visibility of faucial pillars and uvula. If all the three pharyngeal structures in MPS I are visible one can expect adequate exposure of larynx by direct laryngoscopy, on the other hand, if the faucial pillars and uvula are masked in MPS III by the base of the tongue and only soft palate is visible one should anticipate difficult endotracheal intubation secondary to inadequate exposure of larynx by direct laryngoscopy.
Cohen, et al., who compared mallampati grade with CL grading during laryngoscopy and found that mallampati class A patient’s have easy laryngoscopic visualization and relatively easy to intubate as compared to class C patient’s have poor glottic exposure [20]. The study confirms work showing that ability to visualize structures of the hypopharynx is a good predictor of subsequent glottis visualization during laryngoscopy and of ease of intubation. This study is in correlation to our study which shows that in most of the cases modified mallampatti classification and cormack and lehane grading is a good predictor for tracheal intubation. It correlates in most of the cases on video laryngoscopy.
Out of 122 cases, in 83.60% cases of mallampati classification classes successfully predicted cormack and lehane grade I and II (i.e ease of laryngoscopic tracheal intubation), the results of our study are similar to that of Cohen, et al. The average sensitivity of mallampati grade 1-4 in study was 25.52% while the specificity being 74.48%. The mallampati classification with cormack and lehane grading is as good predictor for tracheal intubation. However mallampati classification did not correlate grade to grade with cormack and lehane grading on direct laryngoscopy. This study is comparable to our study out of 100 cases in our study 84% cases of mallampati classification classes successfuly predicted Cormack and Lehane grade I and II (i.e ease of laryngoscopic tracheal intubation). The results of study are similar to Cohen, et al. In our study the sensitivity and specificity of modified mallampati various classes with reference to CL grading revealed that for class I sensitivity and specificity was 4.6% and 95.4% respectively for class II sensitivity was 24% and specificity was 76%. For Class III sensitivity was 62.5% and specificity 37.5%. For Class IV sensitivity was maximum 100 percent but specificity was nil.
On an average sensitivity was 47.8% and specificity 52.2 %. Hence the maximum sensitivity was observed for class IV and maximum specificity for class I. In our study sensitivity means true detection rate (true positive) matching in the sense of detection of difficulty with gold standard while specificity shows the rate of unmatching (true negative) of non difficult cases for intubation.
Our study results are also in agreement with the study done by Kaplan MB, et al. a prospective multicenter trial compared the direct and indirect (video monitor) views of the glottic opening using a new Macintosh blade that is modified to provide a video image of airway structures during laryngoscopy in 867 adults undergoing elective surgery requiring general anesthesia and tracheal intubation. They concluded that video assisted laryngoscopy provides an improve view of the larynx, as compared with direct visualization.
Conclusion
They concluded that the technique may be useful for cases in difficult intubation and reintubation as well as for teaching laryngoscopy and intubation. Our study results are also in agreement with the study done by Jungbauer, et al. in 2009 conducted a prospective comparative study on expected difficult intubation of direct laryngoscopy and video laryngoscopy in 200 patients. They evaluated the conditions and success rate of tracheal intubation in patients with a mallampati score of III or IV. They found that video laryngoscopy (By C-MAC) provided a significantly better view of the cords, a higher success rate, faster intubations and less need for optimizing manoeuvres in difficult intubations. In their study out of 100 cases 45 cases are in CL grade I, 45 cases in CL grade II, 10 cases in CL grade III and zero cases in CL grade IV. Out of 100 cases 99 cases are intubated in single attempt, and the duration of laryngoscopy and intubation was 40 ± 31 sec while in our study out of 100 cases 60 cases are in CL grade I, 24 cases are in CL grade II, 12 cases are in CL grade III while 4 cases are CL grade IV. Out of total 100 cases 88 cases are intubated in first attempt while 12 cases are intubated in second attempt, and the duration of laryngoscopy and intubation in our study was <15% for 88% of the cases and >15 sec for 12% of cases.
Our results are in agreement with the meta analysis done by Su YC, et al. to assess value of video laryngoscope when compared with direct laryngoscopy. It was concluded that video laryngoscopes are a good alternative to direct laryngoscopy during tracheal intubation. The advantage seems to be more prominent when difficult intubation is encountered.
Our results are also comparable with the study by Erol cavus, et al. compared for the first time the CMAC® with conventional direct laryngoscopy in 150 patients during routine induction of anaesthesia. Primary end point was change of glottic visualization; secondary endpoints were time to tracheal intubation and success rate. They concluded that combining the benefits of conventional direct laryngoscopy and video laryngoscopy in one device, the C-MAC may serve as a standard intubation device for both routine airway management and educational purposes.
Cavus E, et al. studied the efficacy of C-MAC (Karl storz, Tuttlinging, germany) a new portable video laryngoscope in 60 patients durig routine induction of anaestheisia. Tracheal intubation was successful in all 60 patients; 52 patients were intubated on the first attempt, 6 on the second and 2 on the third attempt. In 8 patients (13%) a gum elastic bougie was required. The mediim time taken for tracheal intubation was 16 Second (Rnage 6-58 Second). In our study out of 100 pt’s, 88 were intubated in firest attempt while 12 were intubated in second attempt while in difficult cases bougie is used in 2 pt’s; BURP was used in 7 Pt’s; Stylet was used in 8 Pt’s while in 83 Pt’s no added manueuver is added.
In our study the time taken for laryngoscopy and intubation was <15 sec in 88 cases and >15 second in 12 cases. Our study results are comparable with the study done by V Hodgetts, et al. In their study out of 45 patients intubated by C-MAC video laryngoscope 13 patients (28.8%) need additional maneuver (Bougie/BURP or Both) While in our study out of 100 patients 2% patients need Bougie, 7% patients need BURP and 8% patients need Stylet. In total 17% patients need additional maneuver in our study. In their study the median intubation time needed is 29.2 ± 18.6 Seconds while in our study 88% patients need time for laryngoscopy and intubation <15 sec in 88% patients while >15 sec in 12% patients. Our study is also comparable to study done by Kiran DS, et al., in a group of 40 cases intubated by C-MAC video laryngoscope BURP is used in 45% of cases, Stylet used in 30% cases, duration of laryngoscopy was 29.5 ± 19.12 while in our study BURP is used in 7% cases, Stylet used in 8% cases, Bougie used in 2% of cases. Duration of laryngoscopy was <15 sec in 88% cases and >15 sec in 12% of cases.
Our study has the following limitations. As the study period was of 1 year duration the total number of patients included was less in number. Therefore the results of this study are not applicable to large scale population group as a longer period of time is required to validate the results of our study. Also the study includes patients coming under ASA class I and II, the results of the study are not applicable for ASA III, IV and V. Overall from the present study and the other evidences following comparing modified mallampati scoring with Cormack and Lehane scoring through video laryngoscope may improve the overall ease of intubation.
References
- Benumof JL. Management of the difficult adult airway. With special emphasis on awake tracheal intubation. Anesthesiol. 75, 1087-110 (1991).
[Crossref] [Google Scholar] [PubMed]
- Hirsch IA, Reagan JO, Sullivan N. Complications of direct laryngoscopy. A prospective analysis. Anesthesiol Rev. 17, 34-40 (1990).
- Johnson KG, Hood DD. Esophageal perforation associated with endotracheal intubation. Anesthesiol. 64, 281-283 (1986).
[Crossref] [Google Scholar] [PubMed]
- Samsoon GLT, Young JRB. Difficult tracheal intubation: A retrospective study. Anesth. 42, 487-490 (1987).
[Crossref] [Google Scholar] [PubMed]
- Lyon G. Failed Intubation: Six year’s experience in a teaching maternity unit. Anesth. 40, 759-762 (1985).
[Crossref] [Google Scholar] [PubMed]
- Hegde HV, Prasad KC, Bhat MT, et al. Airway difficulty in Mallampati ‘class zero’ patients: A prospective double blind observational study. Eur J Anaesthesiol. 29, 338–342 (2012).
[Crossref] [Google Scholar] [PubMed]
- Ezri T, Warters RD, Szmuk P, et al. The incidence of class "zero" airway and the impact of Mallampati score, age, gender, and body mass index on prediction of laryngoscopy grade. Anesth Analg. 93, 1073–1075 (2001).
[Crossref] [Google Scholar] [PubMed]
- Kaki AM, Markabi WA, Fawzi HM, et al. Use of Airtraq, C-MAC and glidescope laryngoscope is better than macintosh in novice medical students’ hands: A manikin study. Saudi J Anaesthesia. 5, 576-381 (2011).
[Crossref] [Google Scholar] [PubMed]
- Channa AB. Video laryngoscopes. Saudi J Anaesth. 5, 357-359 (2011).
- Apfelbaum JL, Hagberg CA, Caplan RA, et al. American society of anesthesiologists task force on management of the difficult airway. Practice guidelines for management of the difficult airway: An updated report by the American society of anesthesiologists task force on management of the difficult airway. Anesthesiol. 118, 251-270 (2013).
- Asai T, Liu EH, Matsumoto S, et al. Use of the Pentax-AWS in 293 patients with difficult airways. Anesthesiol. 110, 898-904 (2009).
[Crossref] [Google Scholar] [PubMed]
- Aziz MF, Healy D, Kheterpal S, et al. Routine clinical practice effectiveness of the glidescope in difficult airway management: An analysis of 2,004 glidescope intubations, complications, and failures from two institutions. Anesthesiol. 114, 34 (2011).
[Crossref] [Google Scholar] [PubMed]
- Kelly FE, Cook TM. Seeing believes: Getting the best out of video laryngoscopy. Br J Anaesth. 1, i9-i13 (2016).
[Crossref] [Google Scholar] [PubMed]
- Frerk C, Mitchell VS, McNarry AF, et al. Difficult airway society intubation guidelines working group. Difficult airway society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 115, 827-848 (2015).
- Fu- Shan Xue, Qian-Jin Liu, Hui-Xian Li, et al. Video laryngoscopy assisted intubation-new era for airway management. J Anesth Perioper Med. 3, 258-269 (2016).
- Xue FS, Li HX, Liu YY, et al. Current evidence for the use of C-MAC video laryngoscope in adult airway management: A review of the literature. Ther Clin Risk Manag. 13, 831-841 (2017).
[Crossref] [Google Scholar] [PubMed]
- Hoshijima H, Mihara T, Maruyama K, et al. C-MAC video laryngoscope versus macintosh laryngoscope for tracheal intubation: A systematic review and meta analysis with trial sequential analysis. J Clin Anesth. 49, 53-62 (2018).
[Crossref] [Google Scholar] [PubMed]
- Collins SR, Blank RS. Fiberoptic intubation: An overview and update. Respir Care. 59, 865-878 (2014).
[Crossref] [Google Scholar] [PubMed]
- Asai T. Video laryngoscopes: Do they truly have roles in difficult airways? Anesthesiol. 116, 515-517 (2012).
[Crossref] [Google Scholar] [PubMed]
- Jungbauer A, Schumann M, Brunkhorst V, et al. Expected difficult tracheal intubation: A prospective comparison of direct laryngoscopy and video laryngoscopy in 200 patients. Br J Anaesth. 102, 546-550 (2009).
[Crossref] [Google Scholar] [PubMed]